
22 Oct The Silent Killers: 10 Common Diseases You Might Have Without Knowing
The Silent Killers: 10 Common Diseases You Might Have Without Knowing
By Island Hospital | October 22, 2025 10:34:09 AM
We often believe we’re in control of our health, judging it by how we feel. But imagine living with a disease that quietly damages your body every day—without pain, without warning, without any apparent signs.
Many of us only look for solutions or seek professional help once pain sets in. By then, the damage may already be severe, sometimes even irreversible or beyond help. This is the reality of silent diseases— deadly conditions that develop gradually, often without warning, until significant damage has already been done.
What makes it even more concerning is that these diseases are not rare. In fact, they are alarmingly common. Almost every family has someone at risk, whether due to genetics, lifestyle, or age. Together, they affect hundreds of millions of people and claim millions of lives each year, often only discovered after a medical emergency.
In this article, we’ll explore 10 diseases that show no symptoms until it’s too late — why they’re so dangerous, and most importantly, what you can do today to protect yourself and your loved ones.
The Silent Threats: Your Comprehensive Guide to Early Detection
Not all dangers to your health come with obvious warning signs. Some of the most serious conditions develop quietly, often with no symptoms at all, until the damage is already advanced.
We’ve seen how silent diseases can put your health at risk, but what exactly are they, and why are they so dangerous? To answer this, let’s take a closer look at five of the most common conditions that often progress unnoticed until it’s too late.
| Disease | Subtle Signs | Screening Test | Recommended Frequency |
|---|---|---|---|
| Hypertension (High Blood Pressure) | Usually none; headaches or dizziness only when severe | Blood pressure measurement | Yearly (healthy adults); every 3–6 months if high risk |
| High Cholesterol | Xanthelasma (yellow eye deposits), xanthomas, chest pain (late) | Lipid panel (blood test) | Every 4–6 years (20+); every 1–2 years if high risk |
| Silent Heart Attacks | Jaw/back pain, shortness of breath, nausea, unexplained fatigue | ECG, echocardiogram, stress test | Every 1–2 years if over 40 and at risk |
| Lung Cancer | Persistent cough, coughing blood, chest pain, weight loss | Low-dose CT scan (LDCT) | Annual (50–80 yrs, heavy smokers/current/quit within 15 years) |
| Colon Cancer | Blood in stool, bowel changes, abdominal pain, anaemia | Colonoscopy (gold standard) | Every 10 years from 45+; stool tests every 1–3 years |
| Type 2 Diabetes | Excess thirst, frequent urination, blurred vision, dark skin patches (acanthosis nigricans) | Blood sugar (fasting glucose, HbA1c) | Every 3 years after age 35; yearly if high risk |
| Chronic Kidney Disease (CKD) | Fatigue, swelling in ankles/feet, foamy urine, frequent night urination | Blood test (creatinine/eGFR), urine test | Every 1–2 years after 40; yearly if diabetic or hypertensive |
| Cervical Cancer | Irregular bleeding, discharge, pelvic pain | Pap smear + HPV test | Pap every 3 years (21–29); Pap+HPV every 5 years (30–65) |
| Prostate Cancer | Frequent urination, weak flow, blood in urine/semen, pelvic pain | PSA test + digital rectal exam | Discuss from 50 (40–45 if high risk); every 1–2 years |
| Fatty Liver Disease | Fatigue, upper right abdomen discomfort, weight issues, jaundice (late) | Liver function blood tests, ultrasound, FibroScan | Every 1–2 years if overweight, diabetic, or high cholesterol |
Cardiovascular and Metabolic Killers
1. Hypertension (High Blood Pressure)
Hypertension, often nicknamed the “silent killer,” is one of the most common health problems worldwide, affecting over 1.4 billion adults in 2024 alone. It develops gradually, quietly straining the arteries and vital organs over time, and greatly increases the risk of stroke, heart attack, kidney disease, and even vision loss.
Why it’s silent?
Blood pressure rises gradually over time, and the body quietly adapts to these changes. Even when readings are dangerously high, most people continue to feel perfectly normal.
Unlike pain or fever, there are no obvious warning signals to alert you, which is why hypertension can go undetected for years without regular checks. For many, the condition is only discovered after a serious complication such as a stroke or heart attack.
The subtle signs
- Severe headaches, nosebleeds, or dizziness (usually only when levels are dangerously high)
- Blurred vision or shortness of breath in advanced cases
- For many, the first “warning” is a medical emergency like a stroke or heart failure
Steps to protect yourself
- Screening test
The primary screening for hypertension is a blood pressure measurement, which evaluates the force of blood against the artery walls. A normal reading is usually around 120/80 mmHg, although this can vary slightly with age, sex, and health status. The test is quick, painless, and highly accurate, and can be performed at a clinic, pharmacy, or even at home with a digital monitor. If your blood pressure is consistently above the normal range, your doctor may recommend regular monitoring or additional tests to assess cardiovascular health. - At home monitoring
Investing in a home blood pressure monitor is one of the best ways to stay on top of your health between medical visits. By keeping a record of your daily or weekly readings, you can identify trends early and share accurate information with your healthcare provider.This proactive approach helps your doctor adjust treatment plans more effectively if needed. - Lifestyle habits
Beyond medical checks, daily lifestyle choices play a crucial role in blood pressure management.Reducing salt intake, maintaining a healthy weight, exercising regularly, limiting alcohol, managing stress, and quitting smoking are proven ways to lower the risk of hypertension and its complications. - Combine with other screenings
Because hypertension often goes hand-in-hand with other silent conditions, it’s best to combine blood pressure checks with tests for cholesterol, blood sugar, and kidney function.Together, these screenings give a more complete picture of cardiovascular risk and help doctors intervene early if needed. - Recommended Frequency
For healthy adults, blood pressure should be checked at least once a year. However, those considered high-risk, such as individuals over 40, smokers, people who are overweight, or anyone with a family history of heart disease, should undergo screening every three to six months.In some cases, especially when high readings are detected, your doctor may advise even closer follow-up to prevent complications.
2. High Cholesterol
High cholesterol is another hidden danger that can quietly damage your health. Cholesterol itself isn’t bad, as your body needs it to build cells and produce hormones.
But when levels of “bad” cholesterol (LDL) are too high, fatty deposits build up in the arteries. Over time, these deposits harden into plaques that narrow blood vessels and restrict blood flow. Left unchecked, this process can lead to coronary artery disease, heart attack, or stroke, often without you ever realising it.
Why it’s silent?
Unlike conditions that cause pain or discomfort, high cholesterol produces no symptoms. You can feel completely well and still have dangerously high levels. In fact, many people only discover the problem after a major cardiovascular event, such as a heart attack, or when blood tests are carried out for another reason.
The subtle signs
Most people with high cholesterol will never notice any outward signs. In rare cases, however, these may appear:
- Xanthelasma – yellowish deposits around the eyes
- Xanthomas – small fatty lumps on the skin, often on the elbows, knees, or tendons
- Chest pain or angina – but usually only once the arteries are already significantly narrowed
Although these signs are rare, they should not be overlooked. If you notice any symptoms, it’s essential to have your cholesterol levels checked.
Steps to protect yourself
- Screening test
The primary screening for high cholesterol is a lipid panel — a simple blood test that measures total cholesterol, LDL (“bad”), HDL (“good”), and triglycerides. This test gives doctors a clear picture of how fats are being processed in your body and whether your arteries may be at risk. - Lifestyle habits
Diet and lifestyle play a crucial role in managing cholesterol levels. Reducing intake of saturated fats, avoiding trans fats, eating more fibre-rich foods, exercising regularly, and maintaining a healthy weight all help lower LDL levels while boosting protective HDL cholesterol. - Combine with other screenings
Because high cholesterol often goes hand-in-hand with hypertension and diabetes, it is best tested alongside blood pressure and blood sugar checks. Together, these results provide a comprehensive view of your cardiovascular risk profile. - Recommended frequency
Adults should have their cholesterol checked at least once every four to six years, starting in their 20s. However, if you are overweight, diabetic, a smoker, or have a family history of heart disease, testing should be done more frequently, often every one to two years, or as advised by your doctor.
3. Type 2 Diabetes
Type 2 diabetes is one of the fastest-growing health concerns worldwide. It occurs when the body either resists the effects of insulin or doesn’t produce enough to maintain normal blood sugar levels.
Over time, persistently high glucose damages blood vessels, nerves, kidneys, and eyes. Left untreated, it can lead to serious complications such as heart disease, kidney failure, blindness, and amputations.
Why it’s silent?
In its early stages, type 2 diabetes usually develops slowly and without clear warning signs. Many people can live with the condition for years without realising it, often dismissing subtle changes as stress, ageing, or lifestyle-related fatigue. By the time obvious symptoms appear, organ damage may already be underway.
The subtle signs
Most early symptoms are easy to miss, but these subtle signs can sometimes appear:
- Acanthosis nigricans – dark, velvety patches of skin on the neck, armpits, or groin
- Frequent urination – often accompanied by excessive thirst
- Blurred vision – caused by fluctuating fluid levels in the eyes
- Fatigue and slow-healing wounds – due to impaired circulation and nerve function
- Numbness or tingling in hands and feet – a sign of nerve damage in more advanced cases
Steps to protect yourself
- Screening test
The main tests for type 2 diabetes include fasting blood glucose, an oral glucose tolerance test, and HbA1c, which measures your average blood sugar levels over three months. These tests are simple blood draws that provide critical insight into how your body regulates glucose. - At-home monitoring
If diagnosed, your doctor may recommend at-home blood sugar monitoring with a glucometer or continuous glucose monitor (CGM). This allows you to track patterns and adjust lifestyle or treatment accordingly. - Lifestyle habits
A healthy diet, regular physical activity, weight management, and stress control can significantly reduce the risk of developing type 2 diabetes or help manage it if already diagnosed. Avoiding excessive sugar and processed foods is key to preventing blood sugar spikes. - Combine with other screenings
Because diabetes is strongly linked to heart disease, kidney disease, and eye problems, blood sugar tests should be combined with blood pressure checks, cholesterol panels, and annual eye exams. - Recommended frequency
Adults should begin screening for diabetes at age 35, repeating every one to three years if results are normal. However, if you are overweight, sedentary, have high blood pressure, or a family history of diabetes, testing should begin earlier and occur more frequently as recommended by your doctor.
4. Silent Heart Attacks
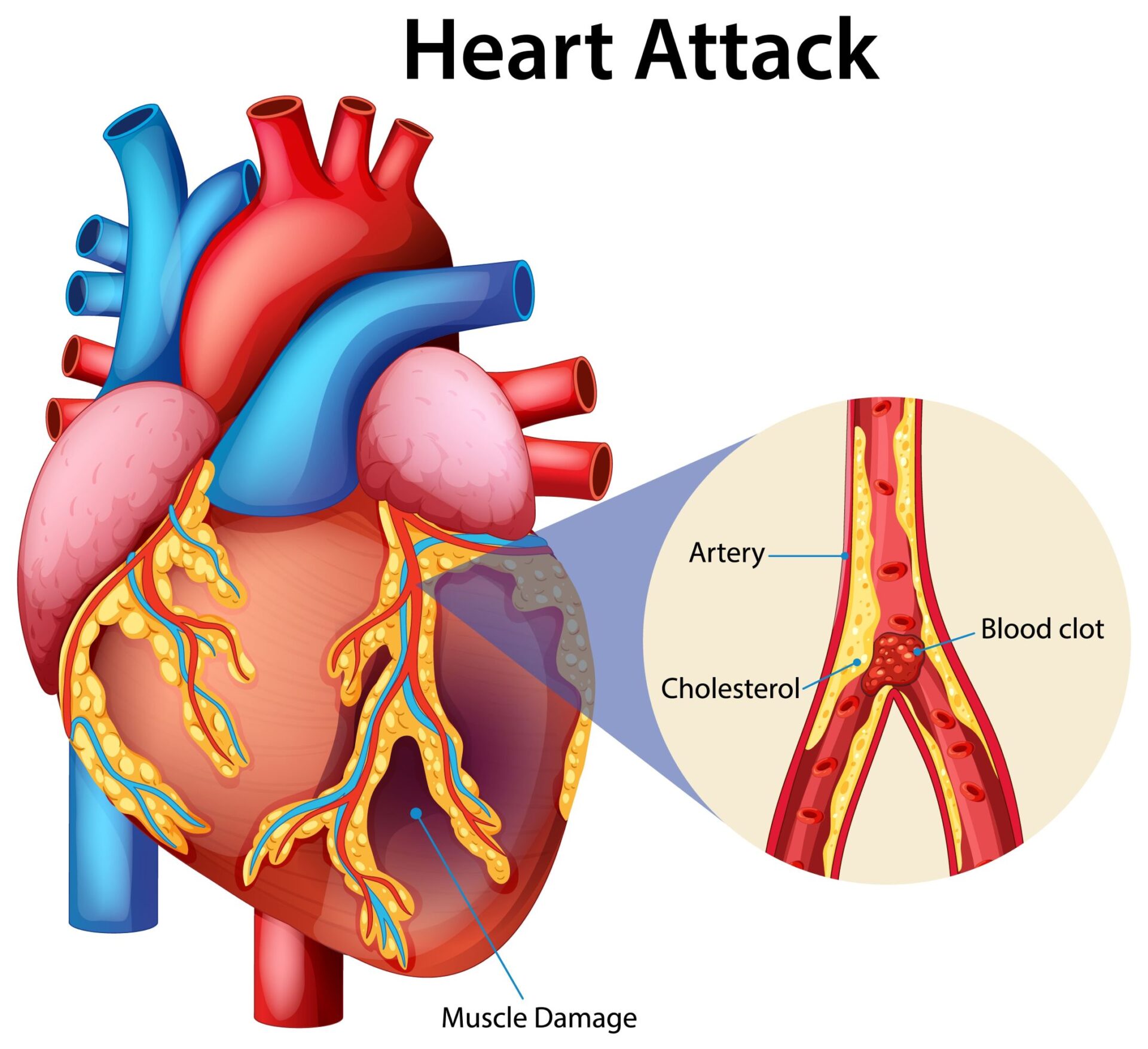
A heart attack is usually imagined as sudden, dramatic chest pain, but not all heart attacks announce themselves this way. A silent heart attack happens when blood flow to the heart muscle is blocked, but the warning signs are so mild, unusual, or easily dismissed that the person doesn’t realise they’ve had one.
Why it’s silent?
Silent heart attacks often present with vague or non-classic symptoms that people mistake for indigestion, fatigue, or muscle strain.
Unlike the crushing chest pain seen in classic heart attacks, these symptoms are subtle enough that they can go unnoticed. Because of this, many people only discover they’ve had a silent heart attack during a routine ECG or after developing complications such as heart failure.
The subtle signs
Symptoms may vary between men and women, and they’re often mistaken for minor issues:
- Mild chest discomfort – pressure, tightness, or burning that doesn’t feel severe
- Pain in unusual areas – such as the jaw, neck, back, or stomach (more common in women)
- Shortness of breath or light-headedness – often dismissed as stress or fatigue
- Nausea or indigestion-like feelings – sometimes mistaken for gastrointestinal problems
- Unexplained fatigue – especially common in women and older adults
Steps to protect yourself
- Screening test
An electrocardiogram (ECG) is the most common test to detect signs of a past silent heart attack. In some cases, your doctor may also recommend an echocardiogram, stress test, or cardiac enzyme blood test to assess heart function and detect damage. - At-home monitoring
While you can’t detect a silent heart attack at home, monitoring your blood pressure, cholesterol, and blood sugar regularly can reduce your overall risk. Paying attention to subtle but persistent symptoms like unexplained fatigue or chest discomfort is also important. - Lifestyle habits
Maintaining a healthy lifestyle is the best prevention. Eat a heart-healthy diet, exercise regularly, manage stress, avoid smoking, and limit alcohol consumption. Keeping your blood pressure, cholesterol, and diabetes under control greatly reduces your risk. - Combine with other screenings
Because silent heart attacks share risk factors with other cardiovascular diseases, it’s important to combine heart evaluations with cholesterol, blood sugar, and kidney function tests for a complete health profile. - Recommended frequency
There’s no universal screening schedule for heart attacks, but adults over 40, especially those with risk factors such as smoking, high cholesterol, hypertension, or diabetes, should have regular heart health evaluations. Your doctor may suggest ECGs or stress tests every 1–2 years if you’re in a high-risk group.
Silent Cancers
5. Lung Cancer
Lung cancer is one of the most common and deadliest cancers worldwide. It develops when abnormal cells in the lungs grow uncontrollably, often spreading before the disease is detected.
Because the lungs have very few pain receptors and a large reserve capacity, cancer can progress significantly before it interferes with breathing or causes noticeable discomfort. By the time symptoms appear, the cancer is often in an advanced stage, making treatment more difficult.
Why It’s Silent
In its early stages, lung cancer rarely causes noticeable symptoms. Small tumours can grow without affecting breathing or causing pain, which is why many cases are only discovered through imaging done for other reasons, or after the cancer has already spread.
The subtle signs
When symptoms do begin to appear, they are often mistaken for common illnesses like a cold or flu:
- Persistent cough that doesn’t go away or worsens over time
- Coughing up blood, even in small amounts
- Chest pain that is dull, constant, or worse with deep breaths or coughing
- Shortness of breath or wheezing
- Unexplained weight loss and fatigue
Steps to protect yourself
- Screening test
The most effective test for early detection is a low-dose CT scan (LDCT), which can identify small lung nodules long before they cause symptoms. Chest X-rays are less sensitive and may miss early cancers. - At-home monitoring
There’s no reliable at-home test for lung cancer, but being attentive to persistent symptoms like chronic cough, chest pain, or coughing up blood should prompt immediate medical consultation. - Lifestyle habits
The single most important step in reducing lung cancer risk is to avoid smoking or quit if you currently smoke. Limiting exposure to second-hand smoke, air pollution, and carcinogenic workplace chemicals also plays a major role in prevention. - Combine with other screenings
Because smoking and environmental factors also increase the risk of cardiovascular disease and chronic respiratory disease, lung cancer screening should ideally be integrated into a broader health check-up for at-risk groups. - Recommended frequency
Screening is not recommended for everyone, but for high-risk individuals, especially adults aged 50–80 who have a history of heavy smoking (or who quit within the last 15 years), annual LDCT scans are strongly advised. Your doctor may recommend additional testing if you have occupational exposures (like asbestos) or a family history of lung cancer.
6. Colon Cancer
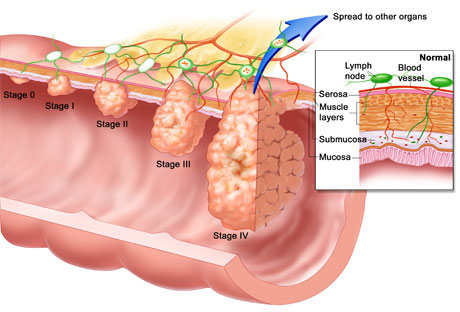
Colon cancer, also known as colorectal cancer, develops when abnormal growths called polyps form in the lining of the colon or rectum. While some polyps remain harmless, others can become cancerous over time.
Because these changes occur slowly and deep within the digestive tract, the disease can progress for years before causing noticeable problems. Colon cancer is one of the leading causes of cancer-related deaths, but it is also one of the most preventable when detected early.
Why it’s silent?
In its early stages, colon cancer often produces no symptoms at all. Small polyps or tumours can grow quietly inside the colon without causing pain or disrupting bowel function. Symptoms usually appear only once the cancer is more advanced, which is why routine screening is the key to catching it before it spreads.
The subtle signs
When symptoms do emerge, they may be vague and easily attributed to other digestive issues:
- Changes in bowel habits such as persistent diarrhoea, constipation, or narrower stools
- Blood in the stool or rectal bleeding
- Persistent abdominal discomfort, cramping, or bloating
- Unexplained weight loss and fatigue
- Anaemia (low red blood cell count) due to hidden internal bleeding
Steps to protect yourself
- Screening test
The gold standard for colon cancer detection is a colonoscopy, which allows doctors to directly view the colon and remove polyps before they turn cancerous. Other options include stool-based tests (such as FIT or FOBT), flexible sigmoidoscopy, and CT colonography.
- At-home monitoring
Stool-based tests (like FIT kits) can sometimes be performed at home and sent to a lab for analysis, but they are not a substitute for colonoscopy if polyps are suspected. Paying attention to ongoing digestive changes and reporting them to your doctor is also important. - Lifestyle habits
A diet high in fibre and low in processed meats, regular physical activity, maintaining a healthy weight, and avoiding smoking and heavy alcohol use can all lower the risk of colon cancer.
- Combine with other screenings
Because colon cancer risk increases with age, it is often recommended alongside other midlife screenings such as prostate, cervical, or breast cancer checks, depending on gender. - Recommended frequency
Adults at average risk should begin colon cancer screening at age 45. Colonoscopies are generally repeated every 10 years if no abnormalities are found, while stool-based tests are recommended every 1–3 years. Those with a family history or other risk factors may need to start earlier and test more frequently.
7. Cervical Cancer
Cervical cancer develops in the cells of the cervix, the lower part of the uterus that connects to the vagina. Most cases are caused by persistent infection with high-risk strains of the human papillomavirus (HPV), a very common virus transmitted through sexual contact.
Because HPV infections are usually symptomless and can take years to develop into cancer, cervical cancer often progresses quietly, making regular screening essential for prevention.
Why It’s Silent?
In its early stages, cervical cancer rarely causes pain or discomfort. Pre-cancerous cell changes in the cervix can exist for years without being noticed. By the time symptoms such as bleeding or pelvic pain occur, the disease is usually more advanced.
This long “silent” period is what makes regular Pap smears and HPV testing so critical.
The subtle signs
When symptoms eventually appear, they may include:
- Unusual vaginal bleeding (between periods, after intercourse, or after menopause)
- Watery or foul-smelling vaginal discharge
- Pelvic or back pain
- Pain during intercourse
These signs can easily be mistaken for minor gynaecological issues, which is why screening is the safest way to detect the disease early.
Steps to protect yourself
- Screening test
The two main tests are the Pap smear (Pap test), which checks for abnormal cervical cells, and the HPV test, which detects the virus that can cause these changes. When combined, these screenings provide the best chance of identifying cervical cancer at a very early and treatable stage. - At-home monitoring
While no at-home test can replace Pap or HPV screening, being aware of unusual bleeding, pain, or discharge and reporting it promptly to your doctor is vital. Some countries are also introducing self-sampling HPV kits, but these should always be followed up with professional testing. - Lifestyle habits
Vaccination against HPV is one of the most powerful preventive measures, especially when given before becoming sexually active. Practising safe sex, avoiding smoking, and maintaining a strong immune system also reduce risk. - Combine with other screenings
Cervical screening is often paired with broader women’s health check-ups, including breast exams, pelvic ultrasounds, and reproductive health assessments, to provide a more comprehensive picture of overall wellness. - Recommended frequency
Women should start Pap smears at age 21, repeating every three years until age 29. Between the ages of 30 and 65, women should undergo either a Pap test every three years, an HPV test every five years, or both tests together every five years. Those with higher risk, such as a weakened immune system or history of abnormal results, may need more frequent screening.
8. Prostate Cancer
Prostate cancer is the second most common cancer among men worldwide. It develops in the prostate gland, which sits below the bladder and surrounds part of the urethra.
In many cases, prostate cancer grows very slowly and causes no symptoms until it is advanced, but some forms are aggressive and spread quickly. This makes regular screening essential, especially as men age.
Why it’s silent?
In the early stages, prostate cancer usually does not interfere with urination or sexual function. Because symptoms overlap with non-cancerous conditions like benign prostatic hyperplasia (BPH), many men ignore them until the cancer is more advanced.
The subtle signs
When symptoms do appear, they may include:
- Frequent urination, especially at night
- Difficulty starting or stopping urination
- Weak urine flow or dribbling
- Blood in urine or semen
- Pain in the hips, back, or pelvis (a sign the cancer may have spread)
Steps to protect yourself
- Screening test
The two main tests are the Prostate-Specific Antigen (PSA) blood test and the digital rectal exam (DRE). While neither test is perfect, when used together, they can help detect cancer earlier, before symptoms develop. - Lifestyle habits
A balanced diet rich in vegetables, regular physical activity, and maintaining a healthy weight may lower risk. Avoiding smoking and limiting consumption of red and processed meats can also help. - Recommended frequency
Men should begin discussing prostate cancer screening with their doctor around age 50. Those at higher risk, such as men of African descent or those with a family history, may need to start earlier, at age 40–45. The frequency of PSA testing depends on results and risk level, typically every 1–2 years.
Curious about the early signals your body sends? This article reveals warning signs of different cancers you shouldn’t ignore and how timely action can make all the difference.
Other Hidden Dangers
9. Chronic Kidney Disease (CKD)
Chronic kidney disease is a condition where the kidneys gradually lose their ability to filter waste and excess fluid from the blood.
It often develops slowly over many years, usually as a complication of high blood pressure or diabetes. By the time symptoms appear, kidney damage is often advanced, sometimes requiring dialysis or a transplant.
Why it’s silent?
The kidneys are remarkably resilient and can continue functioning even when significantly impaired. As a result, early kidney damage often does not cause pain or noticeable symptoms.
Most people only discover CKD after routine blood or urine tests or when they begin to experience complications like swelling, severe fatigue, or changes in urination.
The subtle signs
While early CKD is usually symptom-free, later stages may bring:
- Swelling in the ankles, feet, or hands (fluid retention)
- Fatigue and weakness
- Foamy or bubbly urine (a sign of protein leakage)
- Frequent night-time urination
- Unexplained nausea or poor appetite
Steps to protect yourself
- Screening test
CKD is best detected through a simple blood test that measures kidney function (eGFR) and a urine test that checks for protein or blood, both of which can pick up damage years before symptoms start. - Lifestyle habits
Control blood pressure and blood sugar, stay hydrated, eat a diet low in salt and processed foods, and avoid overusing painkillers like NSAIDs. Quitting smoking also slows kidney damage and protects overall health. - Recommended frequency
Healthy adults should get tested every 1 – 2 years after age 40. People with diabetes, high blood pressure, obesity, or a family history of kidney disease should screen annually or as recommended by their doctor.
10. Fatty Liver Disease
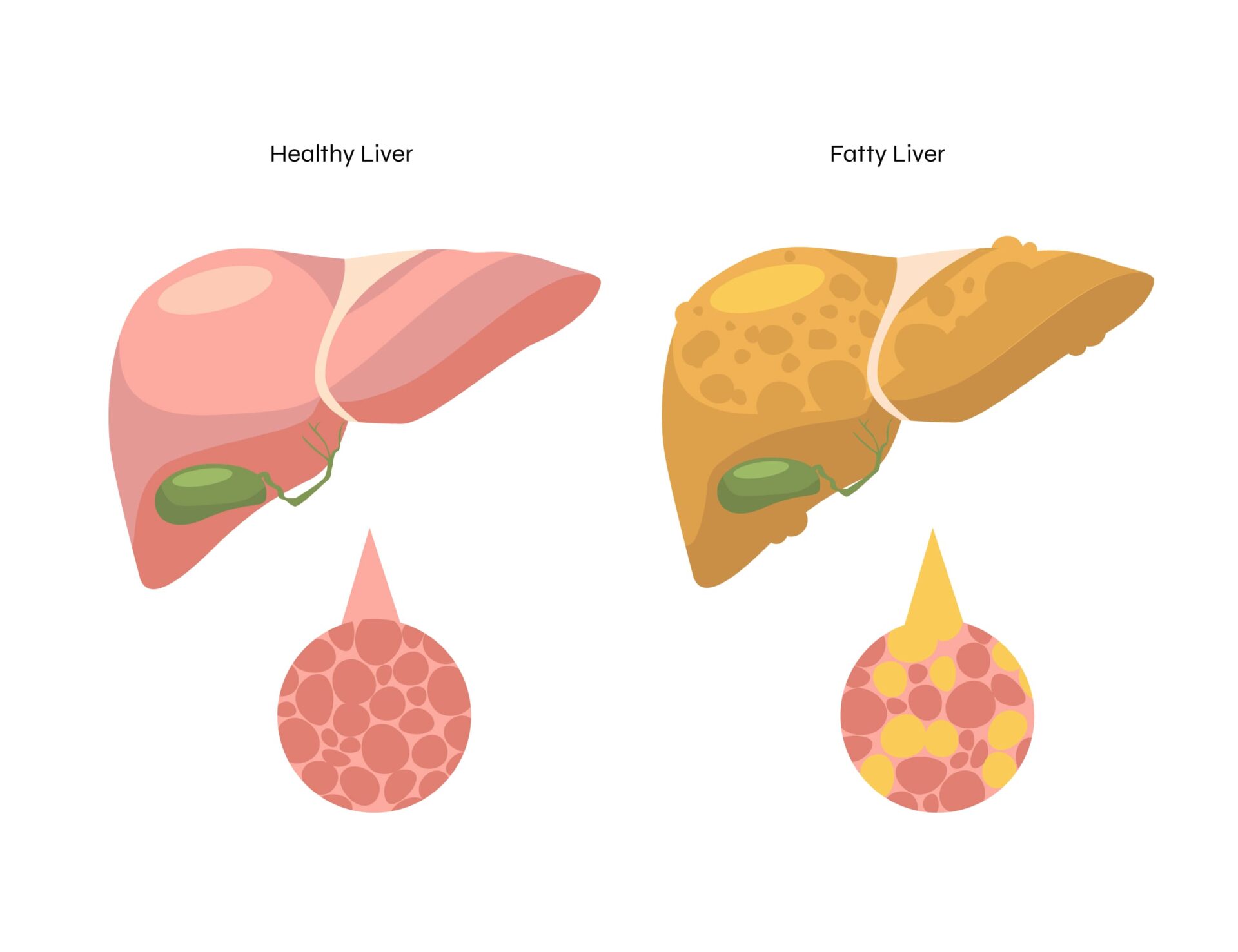
Fatty liver disease occurs when excess fat builds up in the liver cells. There are two main types: non-alcoholic fatty liver disease (NAFLD), often linked to obesity, diabetes, and high cholesterol; and alcoholic fatty liver disease, caused by excessive alcohol intake.
Over time, fatty liver can progress to inflammation (hepatitis), scarring (fibrosis), and even cirrhosis or liver cancer.
Why it’s silent?
The liver has a remarkable ability to repair and adapt, so early fat accumulation usually causes no pain or apparent symptoms. Most people feel completely healthy until significant damage has occurred, making fatty liver a classic “silent” disease. It’s often discovered only through imaging tests or routine blood work.
The subtle signs
Although many people remain symptom-free, possible signs include:
- Persistent fatigue or weakness
- Mild discomfort or fullness in the upper right abdomen
- Unexplained weight gain or difficulty losing weight
- In advanced cases, jaundice (yellowing of the skin or eyes) or swelling in the abdomen and legs
Steps to protect yourself
- Screening test
Fatty liver is usually detected through liver function blood tests (checking enzyme levels) and imaging scans such as ultrasound, CT, or MRI. A FibroScan may also be used to assess stiffness and fat content in the liver. - Lifestyle Habits
Maintain a healthy weight, exercise regularly, and eat a balanced diet low in sugar and processed foods. Limit or avoid alcohol, and manage conditions like diabetes and high cholesterol effectively. - Recommended frequency
Adults at higher risk, particularly those who are overweight, diabetic, or have high cholesterol, should undergo screening every 1–2 years. For healthy individuals, liver checks are often included in comprehensive health screening packages and can be repeated as advised by a doctor.
Hope to expand your knowledge on health screenings? This article on Island Hospital’s comprehensive screening packages has all the details you need!
Your Proactive Health Checklist: What to Do Today
Knowing about silent diseases is only half the battle; the real power lies in taking action. With a few smart habits built into your routine, you can catch problems early, lower your risks, and stay in control of your health.
1. Find a Primary Care Provider
Think of your primary care doctor as your health “quarterback.” They’re not just someone you visit when you’re unwell — they coordinate your overall care, track your health history, and guide you on the screenings you need based on your age, lifestyle, and risk factors.
Establishing this relationship early means your doctor can spot subtle changes long before you would, helping to detect problems early and prevent them from becoming serious.
2. Get Regular Check-Ups
Many people believe check-ups are only necessary when something feels wrong. In reality, they’re your best defence against silent diseases.
A quick blood pressure reading, blood sugar check, or cholesterol panel during a regular visit could reveal risks you’d never notice on your own and could quite literally save your life.
3. Know Your Family History
Your genes carry essential clues about your health. If your parents, grandparents, or siblings have had conditions such as diabetes, hypertension, heart disease, or cancer, your risk may be higher.
Sharing this information with your doctor helps them recommend earlier or more frequent screenings tailored specifically to you.
4. Be Aware of Subtle Changes
Your body often whispers before it screams. Learn to recognise the difference between signs (measurable changes, like high blood pressure) and symptoms (what you feel, like fatigue or dizziness).
Pay attention to persistent or unusual changes, whether it’s unexplained tiredness, changes in bowel habits, or gradual vision problems. They may seem minor, but bringing them up with your doctor can make the difference between early treatment and late-stage disease.
5. Follow Screening Guidelines
Screenings are one of the most powerful tools for detecting silent diseases before they become serious, but only if you follow the right schedule. Each stage of life comes with different health risks, which is why doctors recommend age and risk-specific tests.
Planning on getting a health screening?
At Island Hospital, our comprehensive Health Screening Packages bring all the essential checks together in one convenient appointment. No need for multiple visits — you’ll walk away with a complete picture of your health in a single session.
From women’s and men’s wellness screenings, to executive packages for busy professionals, pre-university screenings for students, and more specialised options like cardiac and dental screenings, we cover every stage of life and every health need.
Take charge of your health today — book your screening with Island Hospital and invest in peace of mind for tomorrow.
Catch Silent Diseases Before They Catch You
Silent diseases may not show symptoms, but they don’t have to catch you off guard. With the right knowledge and timely screenings, you can detect problems early when they’re most treatable and protect your future health.
At the Island Hospital Health Screening Centre, our dedicated team and advanced facilities make early detection simple, reliable, and accessible. Whether it’s a routine check, a specialised screening, or a comprehensive full-body assessment, our goal is to give you clarity, confidence, and peace of mind.
Don’t wait for symptoms to appear. Schedule an appointment today!

Your overall health is the foundation of your well-being, and the key to protecting it is early detection. Regular screening helps uncover silent symptoms, prevent complications, and support long-term wellness
At Island Hospital, our Executive Health Screening Package offers a comprehensive check-up designed to catch potential problems early — even before symptoms arise.
For RM760, you’ll receive expert care, advanced diagnostic tests, and a personalised consultation to help you stay ahead of your health.
What’s Included in Your Screening Experience:
- Comprehensive blood tests
- Chest X-ray
- Electrocardiogram (ECG)
- Ultrasound abdomen & pelvis
- Urine analysis
- Physical examination and detailed consultation
Take a proactive approach to your health — this screening package helps detect potential issues early, so you can manage conditions like GERD before they become serious.
FAQs
1. Are all diseases without symptoms life-threatening?
Not necessarily. Some conditions without obvious symptoms may remain stable or cause only minor issues, while others, like hypertension or cancer, can be life-threatening if left undetected.
The real danger lies in not knowing. Without regular check-ups, even manageable conditions can progress into serious health problems before you realise it.
2. What’s the difference between a “sign” and a “symptom”?
A sign is something measurable that a doctor can detect, like high blood pressure, high blood sugar, or abnormal lab results.
A symptom, on the other hand, is something you feel and report, such as fatigue, chest pain, or dizziness. Silent diseases are especially dangerous because they may show signs on tests long before you ever notice any symptoms.
3. Can a healthy lifestyle alone prevent all these diseases?
No. While a healthy lifestyle significantly lowers your risk, it doesn’t guarantee complete protection. Genetics, age, and other risk factors still play a role. That’s why prevention requires both healthy habits and regular screenings — they work best together to protect you.
4. Do women and men experience silent diseases differently?
Absolutely. For example, women may experience subtler symptoms during a heart attack, such as nausea or jaw pain, instead of the classic chest pain seen in men. Hormonal differences, pregnancy, and menopause also affect risks. That’s why screenings and risk assessments are sometimes tailored by gender.
5. How do I choose the right health screening package for me?
The best package depends on your age, gender, lifestyle, and family history. A young adult might need only basic tests, while someone over 40 may benefit from more comprehensive screenings like cardiac or cancer checks.
The safest approach is to consult your doctor or screening centre, who can guide you to the package that fits your needs.






