
10 Jun Colorectal Cancer prevention & treatment
Colorectal Cancer prevention & treatment
By Island Hospital | Jun 10, 2020 3:43:18 PM
Cells in our intestine regenerate constantly, growing and dividing in an orderly manner. When certain mutations or conditions occur; the regeneration process is disrupted and cause cells to continue dividing when not needed, eventually causing colorectal cancer.
When the cells in our colon or rectum divide and grow uncontrollably, the cells cluster together and form a polyp. Polyps are small bumps along the walls of the colon and rectum that may grow in size to cause complications. When a polyp continues to grow, it may develop into a cancerous polyp, resulting in colon cancer or rectal cancer. From there, the cancerous polyp can break past the wall of the colon or rectum, spreading cancer to other parts of the body.
Colorectal cancer is used to refer to both cancer that begins in your colon (colon cancer) and also cancer in your rectum (rectal cancer).
The statistics tell us that colorectal cancer is the third most common cancer in the world and the second leading cause of death by cancer; but we’re not often told that colorectal cancer is also one of the most preventable forms of cancer.
This is because most polyps take an average of 8 to 10 years to develop into cancerous polyps. During this time period the polyps can easily be discovered and removed during a colonoscopy, preventing or treating early colorectal cancer.
However, when the polyps are left undiscovered or untreated for a long time, the cancerous polyps will eventually grow into tumors and break past the colon wall. From there, the cancer will either:
- Spread to the surrounding organs (stomach, liver, pancreas)
- Spread to other parts of the body via lymph nodes (stage IV cancer)
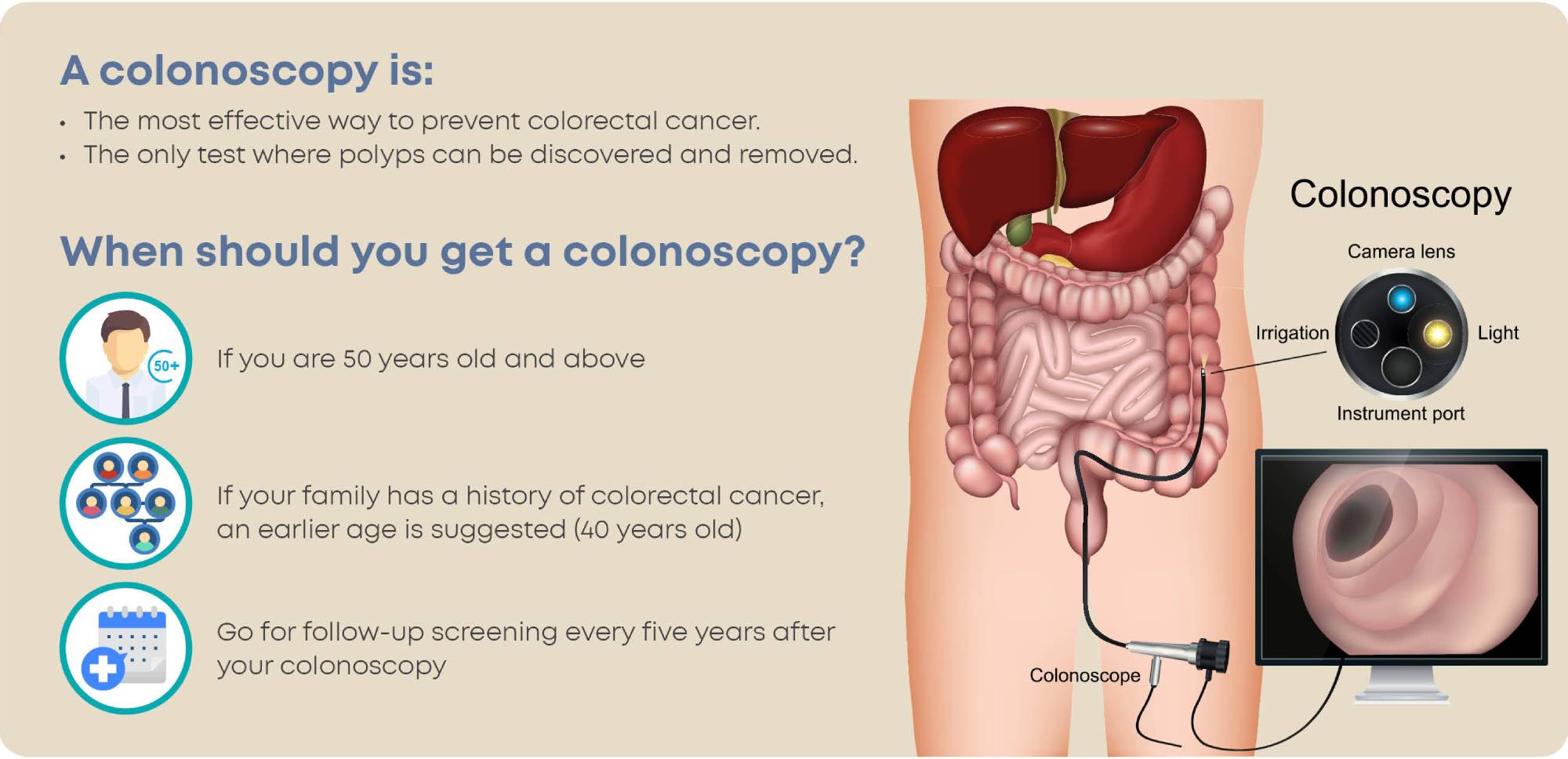
It is recommended for the average person to have their first colonoscopy done at the age of 50, while individuals with a high risk factor may have to do it earlier in their lifetime (age 40 or younger).
Follow-up visits are recommended every few years after your first colonoscopy, and you probably won’t need another colonoscopy for another 5 to 10 years if your risk for cancer is low.
“Colorectal cancer statistics | World Cancer Research Fund.” https://www.wcrf.org/dietandcancer/cancer-trends/colorectal-cancer-statistics. Accessed 20 Mar. 2020.
Q: Can colorectal cancer affect both young and old people?
A: Yes. The majority of colorectal cancer cases occur in people at the age of 50 and above, but colorectal cancer is also known to affect younger individuals at a lower rate. In fact, the number of colorectal cancer cases detected in adults younger than 50 (some as young as their 20s) has increased over the past decade. The good news is that with early screening and prevention, the incidence rates in patients older than 50 has continued to decrease over the years.
Q: Is colorectal cancer genetic or inherited?
A: Studies have shown that individuals have a higher chance of developing colorectal cancer when there is a close family member or family history with the disease. It is recommended to get a colonoscopy at an earlier age (most guidelines recommend 40) if someone in your family has colorectal cancer.
There are also a few known gene mutations that increase the risk of colorectal cancer; the most common ones are Lynch syndrome and Familial Adenomatous Polyposis (FAP).
Lynch syndrome is a type of cancer syndrome and gene mutation that increases the risk of colon cancer as well as other diseases linked to the digestive and reproductive systems.
Familial Adenomatous Polyposis (FAP) is a condition where individuals develop many polyps in their colon, growing up to hundreds or thousands as their age increases.
Individuals with inherited genes and family history only account for 30% to 40% of all colorectal cancer cases. The majority of colorectal cancer cases are actually detected in patients who have no prior family history or genetic mutations that increase their risk.
Q: What causes colorectal cancer?
A: Nobody knows what exactly causes polyps to develop into cancerous polyps, but there are several risk factors that are associated with the disease:
- An unhealthy diet (low fruits and vegetables, high-fat and high in processed meats)
- Lack of regular physical activity
- Overweight or obesity
- Family history
- Tobacco usage
- Heavy alcohol use
These are modifiable risk factors that can be changed to help you prevent colorectal cancer.
For more information on the symptoms, stages, myths and facts about colorectal cancer, read more here: https://islandhospital.com/#medical-info/
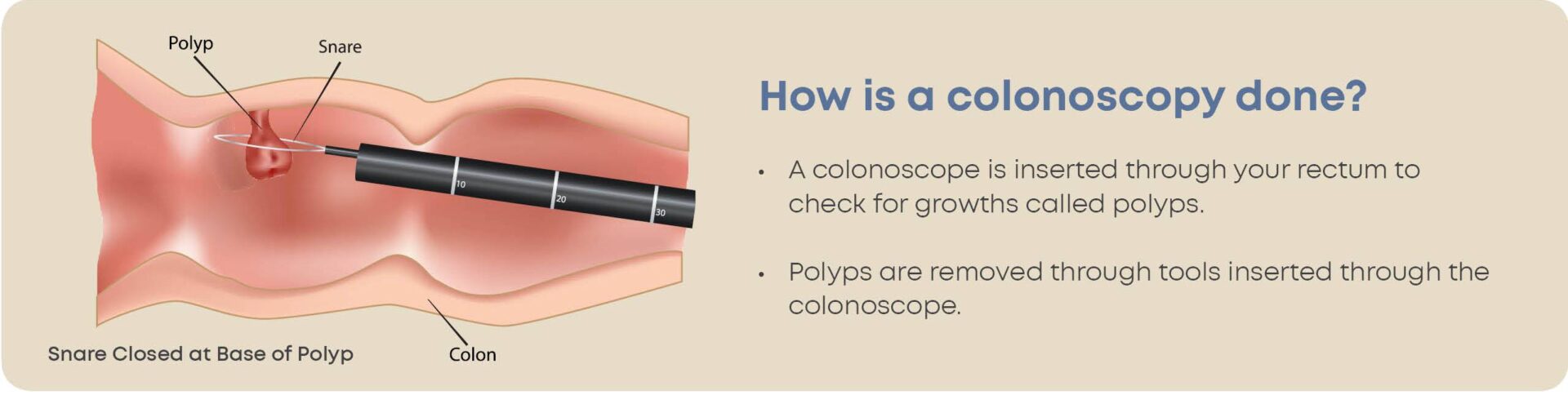
Early colorectal cancer can be treated during a colonoscopy, as the cancer cells are usually contained in polyps (stage 0). Polyps are removed by passing a wire through the colonoscope and then heating it with electricity to burn and cut the polyp off. This process is called a polypectomy.
If the cancer cells have made their way into the colon or rectal wall (stage 1) then a local excision can be used to remove the cancer cells. Like a polypectomy, tools are passed through the colonoscope to cut off the cancerous part of the wall together with a small margin of surrounding healthy tissue to reduce the risk of cancer cells left behind.
When cancerous polyps grow into large tumors that dig into the wall of the colon or grow past the wall, surgery may be required. For cancer in the colon, surgeons will often perform what’s called a colectomy.
Partial Colectomy
During a partial colectomy the surgeon will remove the portion of your colon that contains the cancer, together with a margin of nearby healthy tissues to prevent cancer recurrence. After that, the healthy portions of the colon or rectum are reconnected.
Total Colectomy
This procedure is only necessary when there is a high risk of cancer recurrence in a person’s colon. Inflammatory bowel disease and the aforementioned familial adenomatous polyposis (FAP) are examples of conditions that can greatly increase the risk of colorectal cancer or its recurrence.
A total colectomy will remove the entire patient’s colon and the patient’s small intestine will be connected directly to the rectum at the end of the procedure.
Both a partial and total colectomy can be carried out in 2 ways, either via open surgery or by laparoscopic surgery. A laparoscopic surgery uses smaller incisions and special tools, leading to faster recovery.
Coloanal anastomosis
If the cancer or tumor is located higher above the anus, a coloanal anastomosis can be carried out to remove the rectum along with a margin of surrounding healthy tissue to prevent the recurrence of cancer. Think of it as a colectomy, but removing the rectum instead of a part of the colon.
The colon is then directly connected to the anus and the patient slowly adjusts back to daily life.
Abdominal Perineal Resection (APR)
When the cancer is located extremely close to the anus, both the rectum and anus have to be removed in this procedure to prevent the recurrence of cancer cells. With the absence of the anus your body will require a different way of excreting waste.
A hole known as a stoma will be made in your abdomen, and your colon will be rerouted to the stoma. In order to collect the waste from your colon a pouch will be placed over this stoma. This entire procedure is known as a colostomy.
In cases where the cancer has spread to other parts of the body (metastasis), your doctor may recommend surgery to remove the primary tumor and the metastatic one. For example, if the cancer cells from the colon spread to the liver and form a tumor there, the doctor may recommend surgery to remove both.
If surgery is deemed unnecessary or unsuitable for the patient, alternative forms of treatment are used to treat colorectal cancer in your body.
Chemotherapy
Chemotherapy uses powerful drugs to kill cancer cells. In a colorectal cancer patient, chemotherapy may be used when the cancer tumor has grown past the colon wall; either to kill off the cancer cells or to reduce its size. It may also be used after surgery to kill off any undetectable cancer cells that remain in the body to eliminate the risk of cancer recurrence.
Radiation therapy
Radiation therapy (radiotherapy) kills cancer cells in specific areas of the body by using high-energy beams (X-ray) or by placing radioactive materials in your body. Radiotherapy can also be used to reduce the size of a large cancer before an operation so that it is easier to remove.
Due to age or physical limitations, a patient may be unable to undergo surgery but still experience pain or discomfort. In such cases, radiotherapy can be used to relieve their symptoms.
Targeted therapy
Targeted therapy uses drugs to combat cancer cells, but it is different from chemotherapy. As the name suggests, this therapy targets abnormalities in your cells or tissue that contribute to cancer growth and then blocks that growth, preventing the growth and spread of cancer cells.
This form of treatment benefits older and younger patients who may not be able to go through surgery or other forms of treatment with intense side effects, as the side effects are more manageable than chemotherapy drugs.
Immunotherapy
Rather than use drugs to fight cancer, immunotherapy uses drug treatment to boost your body’s immune system to fight instead. Usually reserved for advanced colon or rectal cancer, immunotherapy has been effective in treating patients with colorectal cancer by interfering with the cancer cells’ ability to fool our immune system’s response.
Every surgery has a chance of risk either before, during or after the procedure; colorectal cancer surgery is no different. Some of the common risks are infections around the surgical wound or area that was operated on (surgical site infection), or urinary tract infection. These risks can be dealt with quickly and effectively as long as the patient looks out for the symptoms.
A major risk to look out for is an anastomotic leak, which is when gastric juices or fluid leaks out of the parts of the colon or rectum that have been reconnected / stapled together. The symptoms of a leak are often diagnosed during the post-operative period or up to a month after surgery, and can be effectively treated when discovered early.
Although the chances of a leak occurring are an average percentage of less than 10%, it is still important for you to be on the lookout for any symptoms of a leak.
Symptoms of an anastomotic leak are:
- Fever
- Abdominal pain
- Diarrhea
- Bleeding
Seek immediate medical help if you experience a combination of any of these symptoms after your surgery.
Following a laparoscopic surgery, you will have to stay and recover in the hospital for a few days, while recovering from an open surgery may require you to stay up to a week.
For the first few months after surgery, you may experience an increase in the number of bathroom visits and may have to stay home more often as a result. Most patients will experience changes in their bowel functions such as increased stool frequency, abdominal cramps and reduced control over their bowel movement.
Your bowel functions will eventually return to normal, but some foods may be handled differently by your body. Give yourself time after surgery to experiment on different foods, some might give you a diarrhea or cause discomfort if your body does not handle it well.
Living with an extra bag
For patients with a colostomy, they will face their own set of challenges. While recovering from your surgery, you will be given appropriate guidance on how to care for your colostomy pouch by our team of doctors and nurses.
Living with a colostomy will require a number of changes in your lifestyle, so to aid the return to your previous daily routine here are some things to keep in mind:
- Skin irritation or infection – If stool leaks under the bag, it can cause skin irritation or infection. Remember to clean the area around the bag and stoma frequently.
- Medication – Some medication can cause constipation or diarrhea. A good tip is to prepare a list of your medications for your doctor or surgeon during consultation, so they can assist you in preparing for taking medications after surgery or colostomy.
- Some foods affect you differently – If your doctor gives you the OK to resume your regular diet, by all means do eat what you like. Some foods may affect you differently after surgery; it doesn’t hurt to try them out at home before eating in public. Knowing how your food affects your digestion helps you manage your expectations better.\
- Life goes on – Your daily life might feel different with the colostomy pouch, but the rest of it is the same. You can go back to work, go back to sports, go out with friends and continue wearing whatever you want. Some of these have to be brought up with your doctor, as certain contact sports with high risk of injury or heavy-lifting work may affect your stoma or pouch.







