21 Jan Cervical Cancer: The second most common cancer in women
Cervical Cancer: The second most common cancer in women
By Island Hospital | Jan 21, 2021 5:09:56 PM
After breast cancer, cervical cancer is the second most common cancer among women in Malaysia. In parts of the world where pap smear tests are not available, then it becomes the most common cause of death by cancer for women.
While cervical cancer is the second most common cancer in women, the good news is that it is also the easiest one to prevent through routine screening. What causes cervical cancer? How can I prevent it? Does it take a long time for cervical cancer to develop?
Here are the answers to some of the questions you might have.
As the name suggests, cervical cancer is cancer that starts in the cervix, which is what connects the uterus (womb) to the vagina. It also helps to keep babies inside the womb until the baby is due.
There are two different types of cells in the cervix; the squamous cells form the surface of the cervix wall while the glandular cells are the deeper parts of the wall. Most forms of cervical cancer begin at the surface (squamous cells), although there are cases where the cancer cells are difficult to detect because they form in a deeper area (glandular cells).
Approximately 90% of all cervical cancer cases are caused by the human papillomavirus (HPV). This virus is a sexually transmitted virus and comes in many different types.
Do not panic if you’re told that you have an HPV infection, as not every type of HPV causes cancer. In fact, most HPV infections will usually go away without treatment; but there are a small percentage of HPV infections can develop into cancer.
HPV can also be transmitted by means other than sexual intercourse. Some of the non-sexual ways HPV can be transmitted are:
- From mother to child (rare)
- Very close physical contact
Some studies also find that smoking, a weakened immune system (as a result of a different disease), having other sexually transmitted infections (STIs) or early sexual activity may contribute to an increased risk of cervical cancer.
Fun fact: There are more than 100 types of the human papillomavirus (HPV), but only 20 are classified as high-risk types. Approximately 70% of all cervical cancers are caused by two types of HPV, the HPV-16 and HPV-18.
Like most other cancers, early-stage cervical cancer produces little to no symptoms. When symptoms begin to develop, it is potentially more advanced and a visit to the doctor is highly recommended. Some of the signs and symptoms of advanced cervical cancer are:
- Vaginal bleeding after intercourse, between periods or after menopause
- Pelvic pain during intercourse
- Watery, bloody discharge from the vagina that is heavy and has a foul smell
- Bleeding from the rectum or bladder
- Pain in one side of the legs
Some women with cervical cancer have little to no symptoms.
During a pap smear test, your doctor may mention the term CIN, which is short for cervical intraepithelial neoplasia.
CIN is what you can call a pre-cancerous condition. Cancer usually develops when the cells in an area undergo mutation and doesn’t stop multiplying/spreading. CIN can be considered the stage where abnormal cells grow on the surface of the cervix, but has not invaded beyond the base of the lining.
CIN is caused by HPV, and just like an HPV infection, most people with CIN do not necessarily develop cervical cancer. Cervical cancer that develops from CIN takes years to develop, meaning there is plenty of time to find and remove problematic cells.
This condition is also split into grades, from a grade of 1 to 3. A more advanced stage of CIN usually means that a large portion of the cervix surface wall has been affected by the abnormal cell change.
Timeline of HPV infection
When an HPV infection starts, there are two outcomes.
- The infection is cleared by the body’s immune system
- The infection is persistent (remains in the body)
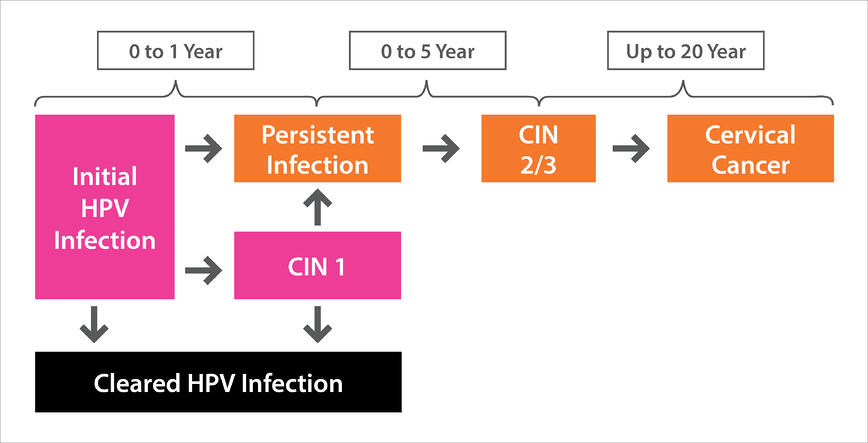
A persistent infection will eventually develop into CIN 2, and if left untreated; develop into cervical cancer.
It takes up to 15 years for cervical cancer to develop in someone, but that number can be reduced to 5 years if you have a weakened immune system.
So, between the start of an infection until you develop cervical cancer, a healthy person has up to 15 years to detect and receive treatment for HPV infection / CIN / cervical cancer.
There are two screening tests that are used to screen for cervical cancer:
- Pap smear
- HPV test
During a pap smear, the doctor will scrape cells from the cervix to be tested for any abnormal cells. If abnormalities are found, you will be called back for repeated testing or follow-ups. Unlike some forms of cancer screening, a pap smear can detect abnormal cells even before the cancer starts to develop.
An HPV test is also carried out in the same way as a pap smear. It can be done by collecting a separate sample from the pap smear, or by using the same sample as the pap smear. If you are getting a HPV test done, then it is usually also performed at the same time as your pap smear. Unlike a pap smear, this test does not detect cancer cells, only the presence of HPV.
Most guidelines will recommend for you to get your first pap smear done at the age of 21 if you are sexually active. If there are no abnormalities, our doctors may tell you to wait for 3 years until your next pap smear.
Even if the results of your pap smear are normal for the first few years, it is still recommended to screen for cancer regularly as some cancer cells take years to develop.
The more partners a woman has, the greater the chance of her being infected with HPV. However, studies show that even women who have only one partner have a 10% chance of getting a HPV infection.
Some of the risk factors for a HPV infection are:
- Women who are sexually active
- Women who have (or had) more than one partner
- Women whose partner(s) have had more than one partner
- Women who have a weakened immune system
- Women who started having sex at an early age (before the age of 18)
A woman’s risk may also change according to circumstance (growing older and lifestyle changes) or if they change partners. Just because your risk is low before or now, does not mean it will remain the same in the future. Regular follow-ups or screening are always recommended so changes can be detected early.
As written above, early sexual activity and smoking are some factors that you can change to decrease your risk of cervical cancer. The longer a person waits before having sex, the fewer partners they are likely to have and thus their risk of transmitting HPV is lower.
It is important to be transparent and also try to understand your partner’s sexual activities/history, so you can both take steps to prevent or treat HPV infections. It’s also important to maintain a healthy diet and lifestyle, so that your immune system can fight off and prevent any HPV infection from developing into cancer.
Most importantly, get screened regularly and get a HPV vaccine when possible. Regular screening can detect abnormal cells before they develop into cancer, and a HPV vaccine can help your body fight off infections.
HPV vaccines should be taken before any sexual activity. That is why in Malaysia, school girls are vaccinated at the age of 13 years old.
It is best (if you have not been vaccinated) to get vaccinated as soon as possible. Men and boys can also benefit from vaccination as there are HPV serotypes that can cause cancer in males as well.
Surgery
Cervical cancer is treatable when detected early, and best while it is still in the pre-cancerous stage. Some of the treatment options are:
Cone biopsy: A small operation that removes the tissue of the cervix in the shape of a cone. While this method is used to gather tissue samples, it can also be used to treat and remove abnormal cells. The cells in the cervix will heal and re-grow after a month.
Surgery to remove the cervix and uterus (hysterectomy): A majority of early cervical cancers are treated using this method, which will remove both the cervix and uterus along with a portion of the nearby lymph nodes.
Radiation / radiotherapy
Radiotherapy is treatment for cervical cancer beyond the first stage and is often combined with chemotherapy for more advanced cervical cancers.
*Radiotherapy causes menopause to occur earlier.
Can I still get pregnant after surgery to treat cervical cancer?
Only if surgery was done while the condition was in its pre-cancerous stage.
Does Island Hospital offer the HPV vaccine?
Yes, we do.
If you wish to get vaccinated for HPV, just make an appointment with any of our consultant gynaecologists.
Why do I need to keep getting tested?
Screening tests have a limited validity, so it is possible that:
- Changes or abnormal cells have formed since your last test
- It takes years for the changes to develop and be detected
- Your risk has changed due to the risk factors listed above (new sexual partner, weakened immune system, undetected HPV infection)
Repeated testing will improve the chances of finding and treating any abnormal changes or infection before it gets worse.
Can I get pregnant after radiotherapy?
No. Radiotherapy to treat cervical cancer will cause infertility. If you wish to remain pregnant after treatment, discuss with your doctor on how to preserve your eggs.