16 Mar Whipple Surgery offers hope and potential cure for pancreatic cancer
Whipple Surgery offers hope and potential cure for pancreatic cancer
By Island Hospital | Mar 16, 2020 3:04:07 PM
The pancreas is an important digestive organ located in the back of the abdomen, behind the stomach. It is about 6 inches long, an oblong-shaped organ surrounded by the stomach, small intestine, liver, spleen and gallbladder. The widest part of the pancreas is the head, the middle section is the body, and the thinnest part is the tail.
To visualise the position of the pancreas, try this: touch your right thumb and right little finger together, keeping the other three fingers together and straight. Then, place your hand in the centre of your belly just below your lower ribs with your fingers pointing to your left. Your hand will be the approximate shape and at the approximate level of your pancreas.
The pancreas serves 2 main functions: it produces enzymes that aid in digestion and it secretes important hormones, such as insulin, that help control metabolism. Hormones help the body use or store the energy that comes from food. The pancreas also makes pancreatic juices which contain enzymes that help digest food. The pancreas releases the juices into a system of ducts leading to the common bile duct. The common bile duct empties into the duodenum, the first section of the small intestine.
Pancreatic cancer is the fourth leading cause of cancer-related deaths worldwide. Cancer of the pancreas is caused when mutated cells grow out of control. Most pancreatic cancers begin in the ducts that carry pancreatic juices. Cancer of the pancreas may be called pancreatic cancer or carcinoma of the pancreas. Because of the deep location of the pancreas, tumours of the pancreas are rarely palpable (able to be felt by pressing on the abdomen). This explains why most symptoms of pancreatic cancer do not appear until the tumour has grown large enough to interfere with the function of the pancreas or other nearby organs such as the stomach, duodenum, liver, or gallbladder.
Pancreatic cancer is especially aggressive and its central location makes it easy for it to spread into adjacent structures and organs such as the liver or stomach. It is usually diagnosed late after it has spread into surrounding organs such as the liver and lymph nodes.
While the exact cause of pancreatic cancer is not known, certain risk factors are strongly linked to the disease, including;
- Smoking is the leading preventable cause of pancreatic cancer.
- Diabetes mellitus can be a symptom of pancreatic cancer, and long-standing adult-onset diabetes also increases the risk of pancreatic cancer.
- Age The risk of developing pancreatic cancer increases with age. With nearly 90% of all pancreatic cancers found in people aged 55 and older
- Family history It has been estimated that ten percent of pancreatic cancers are hereditary.
- Chronic pancreatitis Long-term (chronic) inflammation of the pancreas (pancreatitis) has been linked to cancer of the pancreas.
- Obesity significantly increases the risk of pancreatic cancer. Believe it or not, it has been estimated that 8% of cancers are related to obesity.
Knowing if you are at increased risk can help you and your doctor decide if you should have tests to look for pancreatic cancer early, when it might be easier to treat.
Unfortunately, most pancreatic cancer cannot be prevented, but you can reduce your risks by maintaining a healthy weight, stopping smoking and limiting your alcohol intake. Other risk factors include chronic pancreatitis and family history. Occasionally, precancerous lesions can be identified and, if removed early, can prevent pancreatic cancer from developing.
Pancreatic cancer in the early stages typically causes vague nonspecific symptoms. But if you notice unintentional weight loss, jaundice (yellowish tint to the skin and the whites of the eyes) and unusual stomach pain, it is recommended that you see a doctor immediately to rule out any possible scares.
But, as the cancer grows, symptoms may include:
• Yellowish tint to the skin and the whites of the eyes from jaundice
• Unusual pain in the upper abdomen or upper back
• Weakness/ Lethargy
• Loss of appetite
• Nausea and vomiting
• Weight loss
• Recent diagnosed diabetes
These symptoms are not sure signs of pancreatic cancer. Anyone with these symptoms should see a doctor immediately.
Understanding when symptoms are a sign of something serious and either diagnosing the disease or confirming a previous diagnosis require expertise from specialists trained and experienced in treating pancreatic cancer. At Island Hospital, our team of experts treat all stages of the disease.
If a person has signs and symptoms that might be caused by pancreatic cancer, certain exams and tests will be done.
The most common tests used are an abdominal ultrasound, CT Scan and MRI is especially useful if patient has painless jaundice.
Abdominal ultrasound This may be the first test done because it is easy to do and it does not expose a person to radiation. However, with ultrasound it still may miss the pancreatic tumour as the pancreas is located behind the stomach which may block the sound waves.
CT Scans are important to diagnose pancreatic cancer because they can show the pancreas fairly clearly. They can also help show if cancer has spread to organs near the pancreas, as well as to lymph nodes and liver. A CT scan can help determine if surgery is a possible treatment option.
MRI Like CT Scan, it can also scan the pancreas. Moreover it is radiation-free. The images however are not as clear as a CT Scan. Is it ood for people where radiation is contraindicator (a condition or factor that serves as a reason to withhold a certain medical treatment due to the harm that it would cause the patient – for example, pregnant ladies) Sometimes both are done (CT Scan & MRI)
Blood tests for tumour markers are also available in pancreatic cancer detection.
Tumour markers that may be helpful in pancreatic cancer are:
CA19-9 is a type of tumour marker. Tumour markers are substances made by cancer cells and CA19-9 measures this type of protein in the blood that is often associated with pancreatic cancer.
CEA (CarcinoEmbryonic Antigen) is also a type of tumour marker blood test. The level of CEA may also be raised if pancreatic cancer is present.
However, neither of these tumour marker tests is accurate enough to tell for sure if someone has pancreatic cancer.
Levels of these tumour markers are not high in all people with pancreatic cancer, and some people who do not have pancreatic cancer might have high levels of these markers for other reasons.
Early diagnosis is KEY: Survival rates increases dramatically if the tumour is found earlier and resectable.
Surgery may be suggested as a potentially curative treatment to improve the patient’s quality of life if the tumour is resectable.
The type of surgery required depends largely on the location of the tumour in your pancreas. Your surgeon will recommend the procedure that removes the tumour and affected tissue while safely preserving as much of the pancreas as possible.
People with pancreatic cancer may have several treatment options. Depending on the type and stage, pancreatic cancer may be treated with surgery (Whipple Surgery), radiation therapy, targeted therapy or chemotherapy. Some patients have combination of therapies.
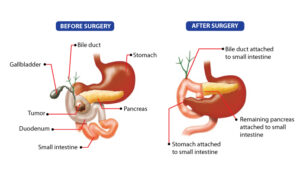
The Whipple Surgery involves removing the head of the pancreas (approximately 30%-35% of the organ), first portion of the small intestine (duodenum), gallbladder, part of the bile duct, occasionally a small portion of the stomach (approximately 10 percent). The goal of this complex surgery is to completely remove the tumour and all surrounding lymph nodes. At the end of the surgery, the surgeon reconnects the remaining pancreas, bile duct and small intestine to restore continuity in the digestive tract.
Whipple Surgery is normally carried out for tumour of the head of pancreas and duodenum.
These may be for;
- periampullary cancer
- lower common bile duct cancer (cholangiocarcinoma)
- pancreatic carcinoma
- duodenum cancer
Whipple Surgery offers the best potential outcome for pancreatic cancer (head of pancreas)
The Whipple Surgery is a technically difficult operation. There are obviously risks in the operation.
These may include:
- Bleeding at the surgical areas
- Infection of the incision area or inside your abdomen
- Delayed emptying of the stomach, which may make it difficult to eat or to keep food down temporarily
- Leakage from the pancreas or bile duct connection
- Diabetes, temporary or permanent
Today, the risk of surgery are low and very acceptable. Mortality rate is about 3-5% and morbidity rate 10%-20%.
Act Fast
All cancers are horrible, but today you are able to do more than ever before. With early detection and treatment, survival rates have improved significantly over the years. But because this type of cancer spreads rapidly, it is crucial to meet with your surgeon and develop a plan as quickly as possible.
If you have been diagnosed with pancreatic cancer, Island Hospital grants you access to the latest diagnostic and treatment advances. Providing you with the best possible patient care is our number one priority. Island Hospital has one of the most experienced teams of surgeons in the country.
Island Hospital is one of the few hospitals in the country that offer the Whipple Surgery; our surgeons have performed more than 100 Whipple Surgeries over the past 4 years. In 2019 alone, our surgeons have successfully completed 38 Whipple Surgeries.
Who is eligible for Whipple Surgery?
Anyone who has been diagnosed with early head of pancreas cancer is potentially eligible for the Whipple Surgery.
At Island Hospital, a group of oncologists, surgeons, radiologists and pathologists with special expertise in pancreatic cancer meet to discuss every case. This team offers guidance about the best course of treatment for each patient.
What are the long term effects of Whipple Surgery?
Complete recovery from the Whipple Surgery can take from one to two months. You will be able to eat normally after recovery. Patients usually need to take a daily vitamin with iron and a daily medication to reduce stomach acid. Those with pre-existing diabetes may require insulin after their surgery.
What other treatment(s) will I need after the Whipple Surgery?
Patients may need chemotherapy as part of their treatment depending on the stage of the cancer. Prior to surgery, chemotherapy is given to shrink the size of the tumour and treat the entire body. If the patient received less than six months of chemotherapy before surgery, the remaining course is given after the patient has recovered from the operation.
Am I too old for Whipple Surgery?
While there is no age limit for the Whipple Surgery, age-related issues and conditions may impact a patient’s medical course and outcome. Island Hospital oncologic surgeons will go through a thorough evaluation of the overall health condition of older patients before considering the surgery.
What are the risk of Whipple Surgery?
Whipple Surgery is a major operation. A patient undergoing Whipple Surgery may face a complication from the operation. About one-third of patients may experience complication from the operation. Complications can be major or minor and can include bleeding, infection and pneumonia.
Why should I choose Island Hospital for my Whipple Surgery?
If you have been diagnosed with pancreatic cancer, Island Hospital grants you access to the latest diagnostic and treatment advances as soon as possible. Providing you with the best possible patient care is our number one priority. Island Hospital has one of the most experienced teams of surgeons in the country performing the Whipple Surgery.
Experience matters
Studies show that hospitals performing a high volume of Whipple Surgeries achieve a lower mortality rate than hospitals that perform few pancreatic resections. The Whipple Surgery itself is complex, taking several hours to perform and requiring a high level of surgical training coupled with excellent technical skills.
Island Hospital is one of the few hospitals in the country that offer the Whipple Surgery; our surgeons have performed more than 100 Whipple surgeries over the past 4 years. In 2019 alone, our surgeons have successfully completed 38 Whipple Surgeries.
The multidisciplinary team in Island Hospital integrates experts in the fields of surgical oncology, pathology, radiology and medical in treating pancreatic cancer.
At Island Hospital, our philosophy is, that at the very least, every patient deserves hope, even when there seems to be little.