
29 Jun What should I know about scoliosis?
What should I know about scoliosis?
By Island Hospital | Jun 29, 2020 11:00:14 AM
Scoliosis is a medical condition where a person’s spine curves to the side, usually in the shape of an “S” or “C”. A stable and mild case of scoliosis does not cause major lifestyle complications, but severe cases with pronounced curves can be bad for a person’s health.
Scoliosis is often discovered in children or teenagers, but is also known to affect adults and the elderly at a lower rate. Minor curves require little to no intervention, but if the curve continues to progress and worsen, then treatment will be provided based on the degree and location of the curve.
In adults, scoliosis can occur as a result of aging, muscle/bone degeneration or complications from a surgery in the past.
People mistakenly believe that carrying heavy bags, poor body posture, playing sports or sleeping on one side can cause the spine to curve, but that is not true. In fact, approximately 80% of all scoliosis cases have no known cause. These cases with no known cause are known as idiopathic scoliosis.
While nobody knows what exactly causes idiopathic scoliosis, there are a few risk factors that have been identified and associated with idiopathic scoliosis:
Age: Most cases occur when a child reaches their growth spurt at the age of 10 and older, during their adolescence. There are also rarer cases that occur earlier in their lifetime, ones that occur at the age of 3 to 9 (juvenile scoliosis) and curves discovered in babies younger than 3 years old (infantile scoliosis).
Sex: Girls are eight times more likely to develop scoliosis than boys.
Family History: Scoliosis can be inherited from parents or affect siblings. If scoliosis is discovered in a child, it would be wise to check on the other siblings for scoliosis.
Cases of scoliosis with a known cause are rarer than idiopathic scoliosis cases, occurring in an average of 1 in every 10,000 people. Non-idiopathic scoliosis is often caused by a poorly developed spine or as a side effect of other diseases.
Neuromuscular scoliosis: The second most common type of scoliosis, caused by nerve or muscular disorders such as cerebral palsy, muscular weakness and spinal cord injury. When the back muscles are weakened or paralysed, there is insufficient support from the back muscles to keep the spine straight.
Unlike idiopathic scoliosis, the spinal curves caused by neuromuscular scoliosis are more likely to progress and continue to curve even as the patient grows into adolescence or adulthood.
Congenital scoliosis: Congenital scoliosis is caused by a defect during the baby’s development in the womb where some parts of the spine are not fully formed or absent. The missing segments of the spine result in a curve as the spine continues to develop. Additional curves may also develop as the spine attempts to straighten or correct the scoliosis, forming double curves or increasing the severity of the curve.
A misleading conception about congenital scoliosis is that there is always a curve in the spine at birth, but that is not true. Some defects do not cause a curve until later in a person’s life.
Degenerative scoliosis: The most common form of scoliosis in adults and the elderly, degenerative scoliosis often occurs in the lower back (lumbar) as part of the natural aging process. Loss of bone mass, deteriorating joints, arthritis or previous spine surgery are all factors that can cause the spine to shift sideways.
Like a building’s structure with a weakened base, degenerative scoliosis may progress as a person continues to age and their spine gradually grows unstable over time. Approximately 60% of adults above the age of 60 are suspected to have mild degenerative scoliosis due to aging. When the degeneration is concentrated on one side of the spine more than the other, a curve may form and progress.
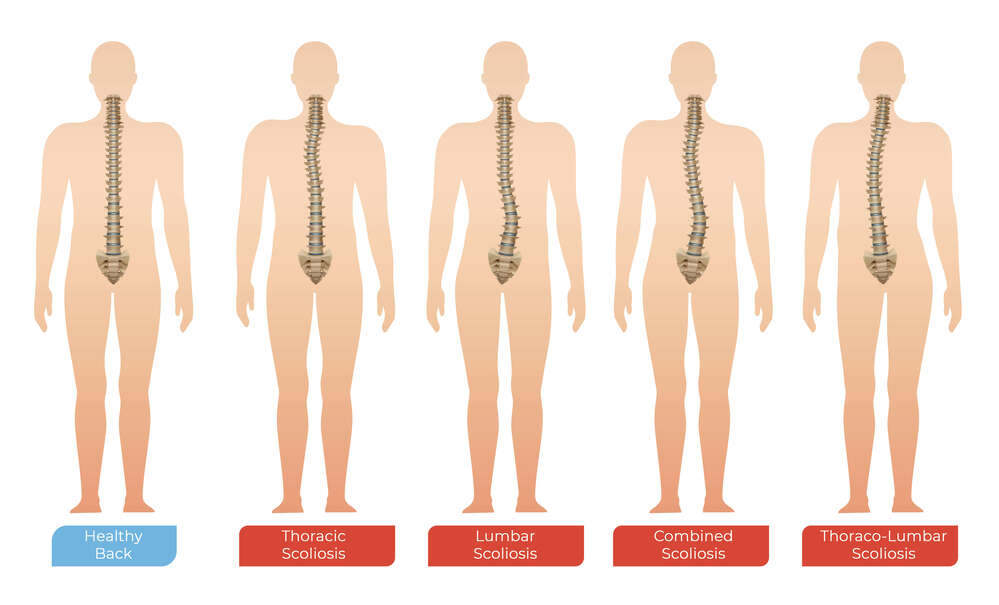
Scoliosis curves are often C-shaped or S-shaped. The curve can also occur in the upper or lower regions of our back, causing the spine to curve in different directions depending on the location of the curve.
Signs of scoliosis become more noticeable as a child grows in age or as the curve progresses, but that doesn’t mean that mild scoliosis is impossible to notice. Generally, you would want to look out for signs of:
- uneven shoulders
- uneven waistline/hips
- one shoulder blade protrudes more than the other side
Scoliosis in children is often discovered during medical checkups when consulting doctors or during a health check-up at school. Clothes can cover up the signs of mild scoliosis.
Adult scoliosis cases are often undiscovered adolescent curves that are noticed only after the skeleton has reached complete growth. Similar to scoliosis in teenagers and children, the signs of scoliosis can be observed when standing straight or bending forward.
In the elderly, pain can be a potential symptom of scoliosis. You might experience one or a combination of the following caused by aging and scoliosis:
- Stiffness or a dull pain in the mid or lower back area.
- A pins-and-needles type of back pain that reaches down to the buttock or legs.
- Shock-like pain that reaches down to the buttock or legs.
Doctors will often use physical exams to check the shape of the spine and test the mobility of the patient. They will also conduct further investigation such as an X-ray or MRI of the spine to determine the severity of the scoliosis and to decide which form of treatment is appropriate.
Treatment for scoliosis varies when it comes to each individual, depending on the age of the patient, degree of the curve, its location and the cause. For mild curves, observation is first carried out during regular check-ups over a period of time to monitor the progression of the curve.
If the curve continues to progress or complications arise as a result of the curve, then the appropriate treatment will be provided. A curve of 25 to 40 degrees is usually considered moderate scoliosis, and is usually treated with a back brace.
Back braces are hard plastic designed to fit around the arms, ribcage and lower back. Wearing a brace will not reverse the curve, but will help slow down or prevent the progression of the spine’s curve in most cases.
The effectiveness of the brace is not necessarily dependent on the brand, rigidity or quality of the brace. It depends if the brace is worn according to the doctor’s advice and recommended time. The usual recommendation is for braces to be worn all the time, including night time and during sleep.
In severe cases of scoliosis, the spine continues to curve even with a brace. Once the curve continues to worsen, doctors will recommend surgery to correct the spine.
Approximately 90% of people identified with idiopathic scoliosis have curves that never progress enough to require bracing or surgery.
Idiopathic scoliosis in adults is a result of undiagnosed scoliosis in adolescents, and as such these cases are handled the same way as scoliosis in children. Observation and assessment are carried out during check-ups before moving on to treatment.
Non-surgical treatment options will be carried out for a few months to assess the patient’s condition and the severity of their case. Some of the possible treatment options are:
Physical therapy: Stretching and simple exercises can be used to test the patient’s mobility during initial evaluation. The exercise plan is adjusted to fit the patient’s personal needs, improving the mobility of the joints, as well as strengthening the muscles in specific areas to reduce pain.
Medication: If the patient experiences back pain due to inflammation or degeneration, the doctor may prescribe medication to relieve pain.
Bracing: While the curve cannot be reversed, wearing a brace may reduce pain in adults with scoliosis.
Treatment for scoliosis in the elderly focuses on the symptoms; whether the person has difficulty moving or feels pain — rather than trying to fix the curve. If the curve is mild and there are no complications that disrupt the patient’s daily life, then treatment is often not necessary as the goal of treatment in the elderly is to relieve pain and restore function.
Surgery is not immediately recommended for adults unless there are complications such as nerve impairment. If symptoms persist or continue to worsen after a period of treatment and care, then surgery becomes a consideration to prevent further damage.
Self-care for adult scoliosis can be as simple as keeping the spine in proper alignment and practising good posture during your day-to-day life.
The lower region of our spine tends to bear most of our body’s weight, so caring for this part is akin to giving a building a strong foundation. Be mindful of the way your lower back is aligned when carrying out daily activities for long periods of time such as standing, walking or sitting. When carrying heavy bags or objects, be aware of how much stress is applied to your lower back and avoid twisting your body around.
Surgery for scoliosis
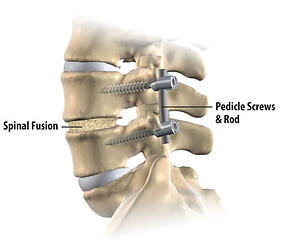
At Island Hospital, Spinal Fusion is performed to correct scoliosis. During a spinal fusion procedure, the surgeon will connect two or more bones in the spine together by placing a bone graft between the vertebrae and then holding it in place using screws or metal rods. Eventually the old and new bone materials will fuse together as the metal rods hold the spine in place.
Spinal fusion surgery is known to be a safe and efficient option to treat scoliosis, although the fused bones will lose mobility. The patient may experience minor limitations when they attempt to bend or twist their back, but the overall mobility of the body remains the same after surgery.
What to expect
Life after spine surgery is not too different from life before surgery. As surgery is reserved for severe curves that cause breathing or functional complications, one can expect these complications to improve over time.
The average hospital stay after spinal fusion is 5 days, while most patients will go through a series of rehabilitation sessions for another week. During the time after surgery in the hospital, the patient will be taught on what they can or cannot do for the months after they return home from surgery.
One can expect the area around the fused bones to feel stiff and sore from time to time, along with some pain. The pain is often mild and does not interfere with daily activities, while some patients may feel a moderate pain that can be relieved using pain medication.
Things to do/not to do!
The most common type of pain felt by scoliosis patients occurs when patients remain in a single position for too long, so it is recommended to change your posture/position every 30 minutes.
Generally, patients will have to avoid lifting heavy objects or activities that put strain on their back, as advised by the doctor. The patient will also have to stay away from potentially strenuous activities like sports and exercise until the doctor gives the OK.
For adults, they will be required to take time off work depending on the nature of their jobs; the average time taken for most adults to get back to work after spinal fusion is 1 month. For patients with jobs that require physical labour, their time away from work may be stretched longer so they can recover as much mobility and strength as possible. However, there is also a possibility that some patients that work at jobs with heavy and intense physical labour may not be able to return to their jobs.
Following a few months of recovery and observation from the doctor, restrictions on physical activity will be lifted and the patient will eventually be able to return to their daily routine.





![[IH 2025] #33 ECG Test_Image 1 medical-machine-ecg-test](https://islandhospital.com/wp-content/uploads/2025/07/IH-2025-33-ECG-Test_Image-1-600x400.png)

