
22 Jan Colonoscopy Procedure: What to Expect
Colonoscopy Procedure: What to Expect
By Island Hospital | Jan 22, 2026 12:00:00 PM
Not all health problems are easy to spot, and issues affecting the colon are among the most difficult to detect. Unlike a sprain or cut that’s visible from the outside, changes inside the digestive tract often go unnoticed until they become serious.
This is why colorectal cancer remains one of the most common yet preventable cancers today, with over 50% of cases potentially avoidable through simple lifestyle changes and regular screening. That’s where a colonoscopy becomes an essential procedure.
Still, many people feel anxious at the thought of getting one. The idea alone can seem intimidating, often creating more fear than the procedure itself. But the truth is that a colonoscopy is one of the simplest, safest and most effective ways to protect your long-term digestive health.
In this article, we walk you through everything you need to know — how to prepare, what happens during the procedure, and what recovery looks like, so you can approach your colonoscopy with clarity and confidence.
What Is a Colonoscopy?
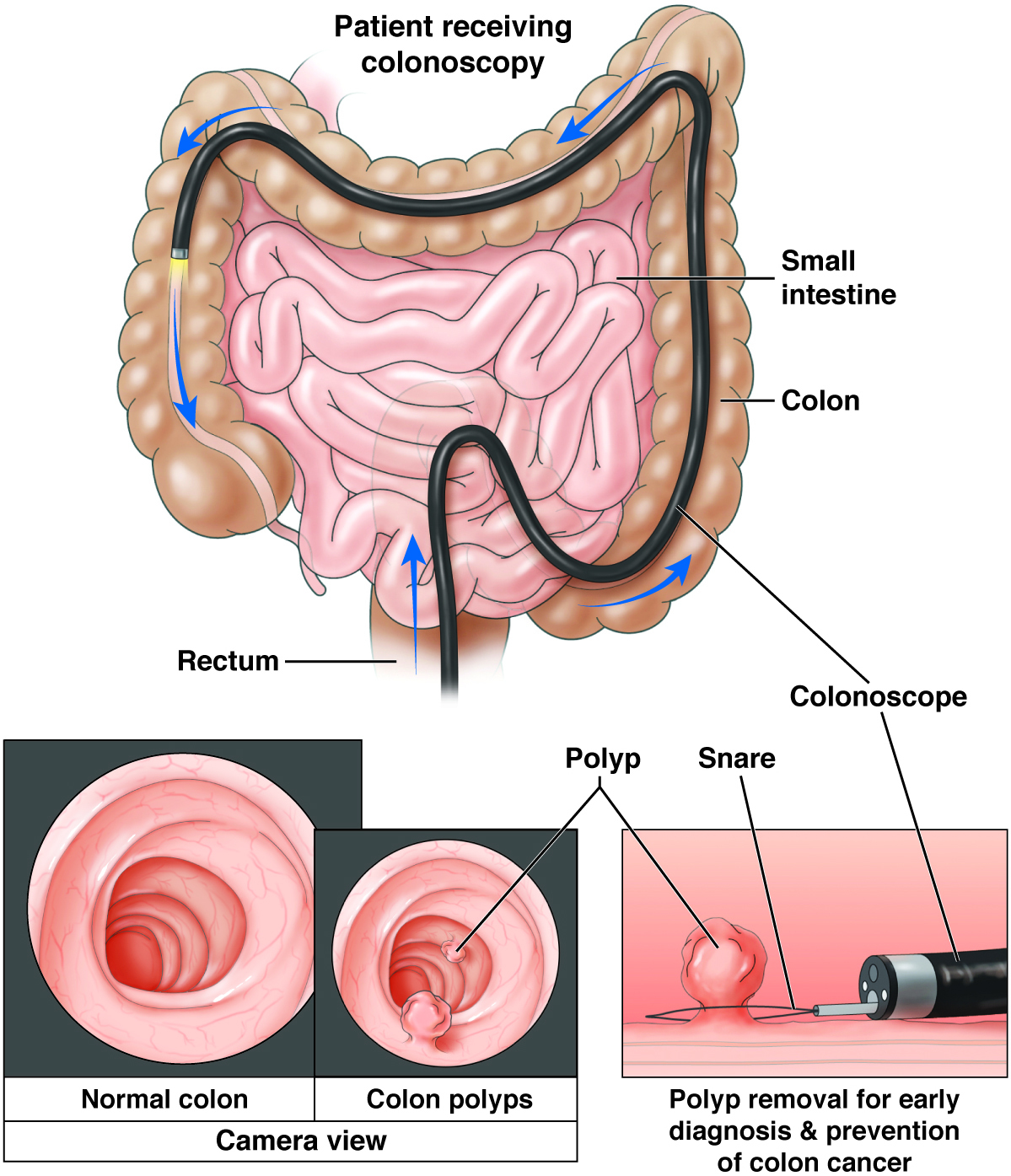
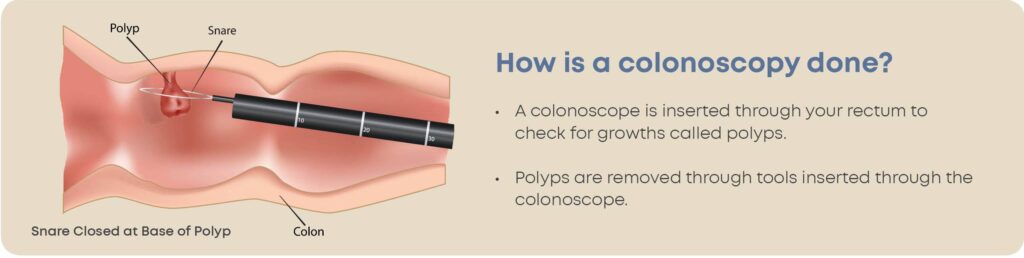
A colonoscopy is a medical procedure that allows a doctor (usually a gastroenterologist) to examine the inside of your large intestine (colon) using a flexible, camera-equipped tube called a colonoscope. This device provides high-resolution images and gently moves through the rectum and colon, providing a clear, detailed view of the intestinal lining.
During the procedure, your doctor can:
- Detect early signs of colon cancer
- Identify inflammation, bleeding or ulcers
- Find and remove polyps (small growths that may develop into cancer)
- Take tissue samples (biopsies) if needed
The procedure is performed under sedation, ensuring comfort, relaxation and minimal awareness. Most people wake up with little memory of the process — and a lot of relief that it was easier than expected.
Want to understand colorectal cancer better — from prevention to early detection to treatment? This article on colorectal cancer has all the details you need!
Who Should Get a Colonoscopy?
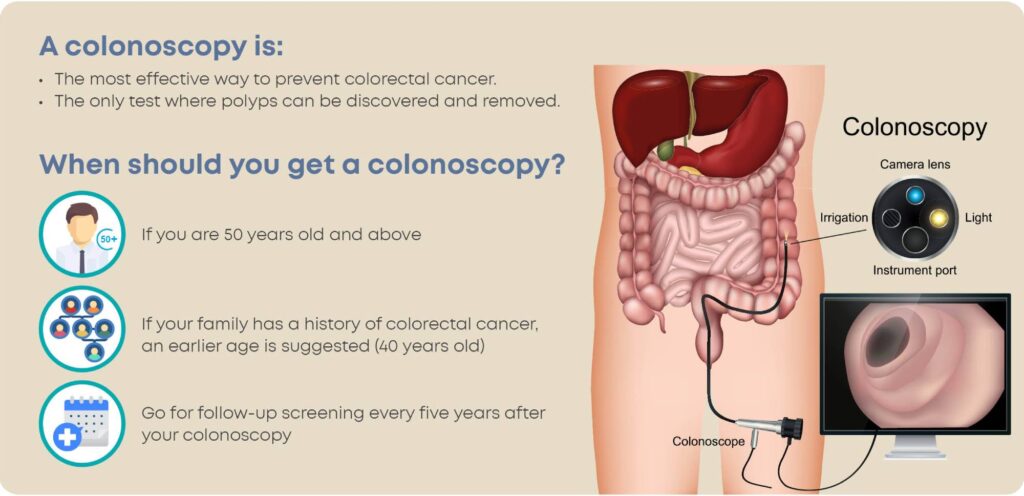
A colonoscopy isn’t only for people with symptoms — it’s one of the most important tools for early detection and prevention, even when you feel completely healthy. Here’s when you should consider getting one:
1. Adults Aged 45 and Above
Medical guidelines now recommend starting routine colorectal cancer screening at age 45, even if you have no symptoms. Early screening helps detect polyps or cancer at a stage when they are easiest to treat or prevent altogether.
2. People With Digestive Symptoms
You should get a colonoscopy if you experience:
- Rectal bleeding or blood in the stool
- Persistent changes in bowel habits (diarrhoea or constipation)
- Unexplained abdominal pain, bloating or cramping
- Unexplained weight loss
- Chronic fatigue related to iron deficiency
These symptoms don’t always mean cancer, but they do need proper evaluation.
3. Individuals With a Family History
Your risk is higher if a first-degree relative (parent, sibling or child) has had:
- Colorectal cancer
- Precancerous polyps
In these cases, screening often begins before age 45, depending on your doctor’s recommendation.
4. People With a Personal Medical History
You may need more frequent colonoscopies if you have:
- Previous polyps
- A history of colorectal cancer
- Inflammatory bowel disease (Crohn’s disease or ulcerative colitis)
These conditions increase your risk and require regular monitoring.
5. High-Risk Groups
A colonoscopy is recommended if you belong to a group with elevated risk, such as:
- Individuals with hereditary syndromes (e.g., FAP, Lynch syndrome)
- Long-term smokers
- People with obesity or a sedentary lifestyle
Your doctor will advise how often you should be screened based on your profile.
Colonoscopy vs Other Screening Tests
There are many screening options for colorectal cancer, but they’re not all equal in accuracy or prevention. If you’re unsure whether a colonoscopy is right for you, this comparison will help you understand how it stands against other tests.
| Test | Colonoscopy (Gold Standard) | FIT Test (Faecal Immunochemical Test) | Stool DNA Test (e.g., Cologuard) | CT Colonography (“Virtual Colonoscopy”) |
|---|---|---|---|---|
| Accuracy | Highest | Moderate | Good | High |
| Frequency | Every 5–10 years | Yearly | Every 3 years | Every 5 years |
| Cost | Higher | Low | Moderate–High | Moderate–High |
| Pros | - Detects & removes polyps in the same session - Most accurate test - Direct visual exam | - Simple home test - No prep or sedation | - At-home convenience - Detects DNA changes linked to cancer | - Non-invasive - Quick scan |
| Cons | - Requires prep & sedation - Recovery time needed | - Only detects hidden blood - Cannot remove polyps - Positive result still needs a colonoscopy | - Higher false positives - Still requires a colonoscopy if abnormal | - Cannot remove polyps - May expose you to radiation - Polyps still require a colonoscopy |
If you want the most reliable, one-and-done screening tool, colonoscopy is the gold standard. It not only detects abnormalities but can also remove polyps immediately, preventing cancer before it starts.
Considering an upper GI endoscopy? This article walks you through the process — what it is, how to prepare, and what happens during and after the procedure.
How to Prepare for a Colonoscopy
Preparing for a colonoscopy is often the part people worry about most — but with a simple plan, it becomes much easier. Good preparation ensures your colon is clear, which helps your doctor get accurate results and avoids the need to repeat the procedure.
Here’s a step-by-step guide to help you get ready.
3–5 Days Before the Colonoscopy
1. Switch to a Low-Fibre / Low-Residue Diet
Start easing your digestive system by reducing foods that are harder to digest or leave residue in the colon.
| Recommended foods | Avoid |
|---|---|
| White rice, porridge, congee | Raw fruits and vegetables |
| Soft bread, noodles, pasta | Nuts, seeds and beans |
| Eggs, tofu | Whole grains |
| Lean chicken or fish | Red meat or fatty cuts |
| Yoghurt or smooth dairy | High-fiber cereals |
Hydration Tips:
A well-hydrated body makes bowel prep smoother.
- Drink 6–8 glasses of water daily
- Avoid alcohol
- Limit carbonated drinks
24 Hours Before the Procedure
1. Clear-Liquids Only
Solid foods are not allowed today. Stick to clear liquids such as:
- Water
- Clear soups or broths
- Tea or coffee (without milk)
- Apple juice
- Isotonic drinks
- Jelly (avoid red or purple)
2. Bowel Prep Timing
You’ll be given a laxative solution to empty your colon. Typically taken in two doses:
- First dose: late afternoon
- Second dose: late evening or early morning (depending on your appointment time)
Follow the instructions exactly — a clean colon is key for accurate results.
3. Medication Guidance
Speak to your doctor if you take:
- Blood thinners (aspirin, warfarin, DOACs)
- Diabetes medications
- Iron supplements
- Blood pressure tablets
You may need temporary adjustments for safety.
Malaysian-Friendly 2-Day Meal Plan
1. Day -2 (Two Days Before)
This day focuses on low-fibre, low-residue meals that reduce strain on your digestive system while still keeping you satisfied.
Breakfast: Soft-boiled eggs + white bread
Lunch: Chicken porridge or fish congee
Dinner: Steamed fish + white rice
Snacks: Yoghurt, tofu pudding
2. Day -1 (One Day Before)
Today, no solid foods are allowed. Your diet should consist entirely of clear liquids to help flush out the digestive system.
Breakfast: Clear soup + tea
Lunch: Apple juice + jelly
Dinner: Chicken broth
Allowed Drinks: Water, isotonic drinks, clear juices, black coffee/tea
Colonoscopy Preparation Checklists
3–5 Days Before
| Start a low-fibre diet | |
| Avoid raw vegetables and fruits | |
| Avoid whole grains | |
| Drink 6–8 glasses of water daily | |
| Plan your clear-liquid meals for prep day |
2 Days Before
| Continue low-residue meals |
|
| Avoid fizzy drinks | |
| Finalise transport arrangements |
|
| Confirm medication adjustments with your doctor |
1 Day Before
| No solid foods at all |
|
| Only clear liquids |
|
| Take the first dose of bowel prep |
|
| Complete second dose (if applicable) |
|
| Stop drinking at the clinic’s advised cut-off time |
Day of the Colonoscopy
| Bring your IC and insurance documents |
|
| Bring someone to accompany you (due to sedation) |
|
| Wear comfortable, loose clothing | |
| Avoid makeup, jewellery and contact lenses |
After the Procedure
| Start with light meals |
|
| Avoid driving for 24 hours |
|
| Monitor for red flags such as severe pain, fever or heavy bleeding |
What Happens During a Colonoscopy?
Knowing what to expect can make the whole experience far less intimidating. A colonoscopy is a straightforward procedure, and with sedation, most people don’t feel or remember much of it. Here’s a simple walk-through of what happens from the moment you arrive until you head home.
1. Arrival and Registration
When you arrive at the endoscopy unit, the medical team will:
- confirm your details,
- review your medical history, and
- ensure you’ve completed your bowel prep.
You’ll then change into a hospital gown and have a brief consultation with the doctor performing the procedure.
2. Getting Ready and Sedation
A nurse will insert a small IV line into your arm to administer sedation. Depending on your doctor’s recommendation, you may receive:
- light sedation (you’re relaxed but awake), or
- deep sedation (you’re fully asleep).
Most patients are comfortably asleep throughout the procedure and wake up with little to no memory of it.
3. The Procedure Begins (20–45 Minutes)
Once the sedation takes effect, the procedure begins. You’ll lie on your side with your knees gently tucked toward your chest — a comfortable position that helps the doctor guide the scope smoothly.
What the doctor does:
- Gently inserts the colonoscope through the rectum
- Slowly guides it through the colon
- Examines the lining using a high-definition camera
- Identifies any abnormalities
The colonoscope also has channels that allow the doctor to:
- remove polyps,
- stop minor bleeding, and
- take biopsies (small tissue samples)
4. Air Inflation and Mild Pressure
To get a clearer view, the doctor introduces a small amount of air or carbon dioxide into the colon. This may cause mild pressure or bloating after the procedure, but you won’t feel it during sedation.
5. Waking Up in Recovery
After the colonoscopy, you’ll be moved to a recovery area while the sedation wears off. Here’s what to expect:
- You may feel slightly groggy or sleepy
- Nurses will monitor your vital signs
- You’ll pass gas as your body releases the air — this is normal and expected
Most people feel well enough to go home within 30–60 minutes.
6. Going Home
You won’t be allowed to drive, operate machinery or make important decisions for the next 24 hours, so someone must accompany you home.
Your doctor will explain your preliminary results on the same day. If any biopsies were taken, you’ll receive the results once the laboratory analysis is complete.
Risks, Side Effects and Safety
A colonoscopy is considered a very safe procedure, especially when performed by experienced gastroenterologists. Most people experience only mild, temporary side effects. However, like any medical procedure, there are some risks to be aware of.
Common Side Effects
These symptoms are very normal and usually disappear within a few hours:
- Bloating
- Gas
- Mild cramping
- Light drowsiness from sedation
These symptoms often occur because air or carbon dioxide is introduced into the colon during the procedure to improve visibility.
Uncommon Side Effects
These are less frequent and usually mild, but it’s helpful to be aware of them:
- Small amounts of rectal bleeding, especially if a polyp was removed during the procedure
- Slight tenderness or discomfort in the abdomen
- Temporary changes in bowel habits, such as slightly looser stools for a day or two
A tiny amount of blood — particularly after polyp removal — is not unusual. However, if the bleeding continues or increases, you should contact your doctor for further guidance.
Rare but Serious Risks
Serious complications from a colonoscopy are very rare, occurring in fewer than 44 in 10,000 cases, especially in the hands of experienced specialists. These include:
- Bowel perforation, which is a small tear in the lining of the colon
- Significant or persistent bleeding, especially after removal of larger polyps
- Severe reactions to sedation, including breathing or heart-related issues
- Infection, though this is extremely uncommon due to strict sterilisation protocols
When to Call a Doctor
While most people recover quickly, you should seek medical attention immediately if you notice any of the following:
- Severe or persistent abdominal pain that does not improve
- Heavy bleeding from the rectum or passing large blood clots
- Fever, chills, or signs of infection
- Persistent vomiting or inability to keep fluids down
- Dizziness, fainting, or unusual weakness
- Black or tarry stools
- Difficulty breathing or chest discomfort
These symptoms are uncommon, but recognising them early ensures that any complication can be addressed promptly and safely.
What to Expect After a Colonoscopy
Even though a colonoscopy involves specialised equipment and sedation, the recovery isn’t as complicated as many expect. Most people bounce back quickly once the sedation wears off, and with a bit of guidance, you’ll know exactly what to expect in the hours and days after the procedure.
1. When You Can Eat
You can usually start eating soon after the procedure, once you’re fully awake. Most doctors recommend starting with:
- Light meals (porridge, soup, noodles, toast)
- Soft, easy-to-digest foods (eggs, yoghurt)
- Plenty of fluids to stay hydrated
Avoid for the first 24 hours:
- Heavy, greasy or spicy foods
- Alcohol
- Large meals
Your digestive system may be a bit sensitive after the bowel prep, so gentle foods help ease you back into your routine.
2. When You Can Drive
Because sedation affects your reaction time, memory and coordination, you cannot drive for 24 hours after the procedure. You must have someone accompany you and take you home. Avoid:
- Driving
- Operating machinery
- Making important decisions
- Signing documents
3. When You Can Return to Work
Most people feel comfortable returning to work the next day, especially if they have a desk job or light duties. Consider taking an extra day if:
- You had multiple or large polyps removed
- You work in physically demanding or high-risk environments
- You’re still feeling groggy from sedation
4. What’s Normal After a Colonoscopy
These symptoms are common and usually settle within 24 hours:
- Bloating or gas
- Mild abdominal cramping
- Feeling tired or sleepy from sedation
- Passing wind frequently (expected due to air used during the procedure)
- Small amount of blood if a polyp was removed
Most people feel back to normal by the next day.
5. When to Seek Help
Seek medical attention immediately if you experience:
- Severe or persistent abdominal pain
- Heavy or ongoing rectal bleeding
- Fever or chills
- Persistent vomiting or inability to keep fluids down
- Dizziness, fainting or unusual weakness
- Black or tarry stools
- Difficulty breathing
These red flags are rare but important to watch for.
Our Centre of Excellence: Gastroenterology

Accredited by ACHSI as a Centre of Excellence, Island Hospital’s Gastroenterology Program delivers world-class digestive care grounded in safety, innovation, and clinical expertise.
Built on internationally benchmarked standards, the program integrates advanced endoscopic technology, evidence-based practices, and multidisciplinary teamwork to provide accurate diagnoses, effective treatment, and compassionate patient support.
The centre offers comprehensive digestive care, addressing everything from everyday gut issues to complex liver, pancreas, and bowel conditions. With advanced endoscopic and minimally invasive techniques, patients receive accurate evaluation and safe, effective treatment designed to support long-term digestive wellness.
Early Detection Starts with a Colonoscopy!
Colorectal issues often develop silently, but early detection makes all the difference. Whether you’re due for a routine screening or experiencing symptoms that concern you, a colonoscopy can provide clarity, peace of mind, and life-saving early detection.
At Island Hospital, our team of experienced gastroenterologists performs colonoscopies with precision, safety, and patient comfort in mind.
Take control of your health today — Schedule your appointment with us!
FAQ
1. Can I drink coffee before a colonoscopy?
Yes, you can drink black coffee before your colonoscopy, but only without milk, creamers, or non-dairy substitutes. These additives are considered solid intake and can interfere with bowel clarity.
You may drink:
- Black coffee
- Tea (without milk)
- Clear juice like apple juice
- Water or isotonic drinks
2. How long will I be sedated?
Sedation typically lasts 20–60 minutes, depending on your age, weight, medication type, and your response. You may continue to feel groggy or sleepy for a few hours after waking up, and your coordination and judgement may still be affected, which is why you cannot drive or make important decisions for 24 hours.
3. What if the bowel prep isn’t working?
If your stool is not turning into clear or pale yellow liquid, your bowel is not fully cleansed. Before panicking, consider the following:
- Sometimes the prep takes longer to work, especially if you are dehydrated.
- Drink plenty of clear fluids to help activate the laxative.
- Walk around to stimulate bowel movement.
If you are still passing brown, thick, or solid stool, or if no bowel movement happens at all, call your clinic. They may recommend an additional dose or adjust your timing.
4. How soon will I get my results?
Your doctor will usually review the initial findings with you on the same day, once you are awake. If polyps were removed or biopsies taken, lab analysis typically takes:
- 3–7 days, depending on the hospital laboratory schedule
- More complex or unusual findings may take longer
5. Is a colonoscopy painful?
No, most people do not feel pain at all due to sedation. What you may feel:
- A sense of pressure or fullness after the procedure
- Mild bloating from the air used to open the colon
- Slight abdominal cramps, similar to gas
During the colonoscopy itself, patients are usually asleep or deeply relaxed. Many describe it as “a short nap” and are surprised by how quick and comfortable the experience is.






