23 Jun Celiac Disease: Complete Guide to Diagnosis, Treatment, and Gluten-Free Living
Celiac Disease: Complete Guide to Diagnosis, Treatment, and Gluten-Free Living
By Island Hospital | June 23, 2025 10:15:00 AM
Living with celiac disease can often feel like navigating a minefield, where everyday foods pose hidden threats to your well-being.
Beyond the immediate discomfort, this autoimmune condition can have far-reaching consequences you might not even connect to your diet.
But you’re not alone in this journey. If you’re proactively seeking strategies to reclaim your health and live vibrantly, this guide offers actionable insights into managing celiac disease through mindful lifestyle changes and cutting-edge medical approaches.
Island Hospital understands the intricacies of celiac disease and is committed to equipping you with clear, transparent guidance and comprehensive support.
Let us empower you at every stage, enabling you to live a full and healthy life.
What is Celiac Disease?
While you likely know that celiac disease is a serious autoimmune disorder triggered by gluten (a protein found in wheat, barley, and rye), it’s important to understand a bit more about its effects on your body.
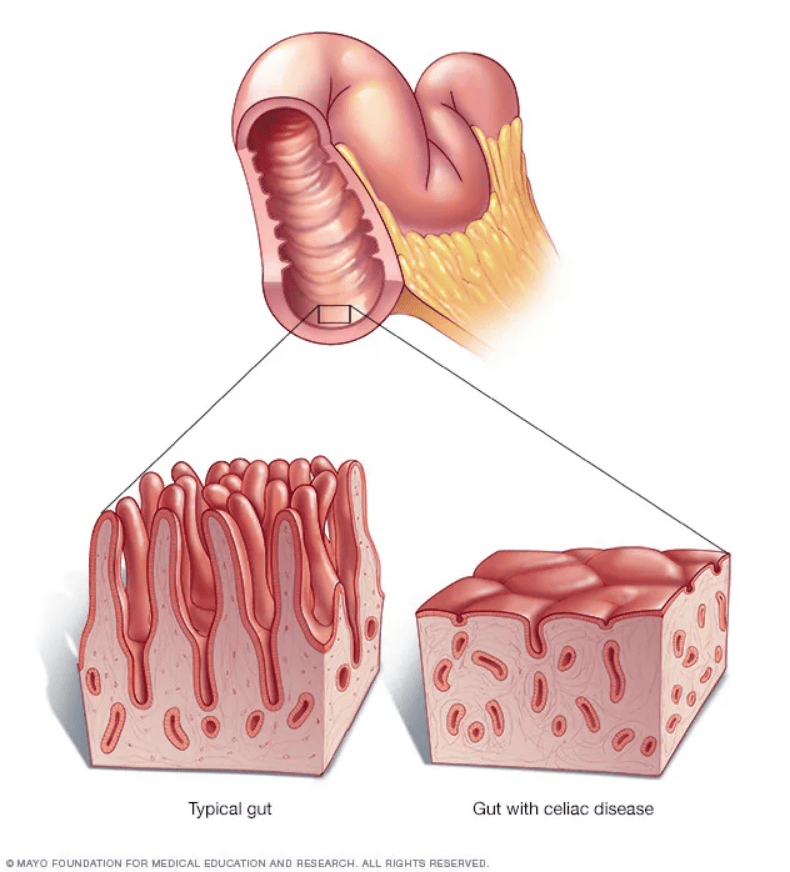
When someone with celiac disease consumes gluten, their immune system mistakenly attacks the lining of the small intestine. Over time, this damages the villi, the tiny finger-like projections responsible for nutrient absorption.
Celiac disease presents with a wide array of symptoms that can differ significantly between individuals and also manifest differently in children compared to adults. Here is the breakdown:
| Symptom Category | Children | Adults |
|---|---|---|
| Digestive | Abdominal bloating and pain, diarrhea, constipation, vomiting, pale and foul-smelling stools, poor appetite | Diarrhea, fatigue, weight loss, bloating and gas, abdominal pain |
| Others | Delayed growth, failure to thrive, delayed puberty, irritability. Dental enamel defects, weight loss, fatigue | Anemia (usually iron deficiency), fatigue, bone or joint pain, osteoporosis or osteopenia, skin rash (dermatitis herpetiformis), nerve damage (neuropathy), headaches and migraines, mouth ulcers, acid reflux, elevated liver enzymes, infertility or recurrent miscarriage. |
For non-classical Celiac, symptoms extend beyond the typical digestive issues where individuals may experience problems like chronic fatigue or iron-deficiency anemia without significant gastrointestinal distress. This often leads to delays in diagnosis.
Conversely, individuals with silent celiac disease are characterised by the presence of intestinal damage caused by gluten, as seen in biopsies, but without any noticeable symptoms.
Despite the lack of outward signs, the internal damage and risk of complications are still present.
Why is Celiac Disease Often Misdiagnosed?
It’s worth considering that symptoms you might attribute to conditions like irritable bowel syndrome (IBS), migraines, or chronic fatigue could actually point towards a higher likelihood of having celiac disease.
There are multiple reasons why Celiac disease is often misdiagnosed:
1. The Chameleon Effect of Overlapping Symptoms
Celiac disease is a master of disguise. Its symptoms, particularly those beyond the typical digestive upset, frequently overlap with a host of other more common conditions.
For instance, fatigue could be attributed to stress or anemia, joint pain to arthritis, and skin rashes to eczema. Even digestive issues like bloating and diarrhea are hallmarks of IBS or lactose intolerance.
This mimicry makes it easy for both individuals and healthcare providers to initially suspect and treat other ailments, delaying consideration of celiac disease.
2. The Enigmatic Nature of Silent Celiac
Perhaps the most significant contributor to diagnosis is the existence of “silent” celiac disease. Individuals with this form experience intestinal damage due to gluten consumption but exhibit no noticeable symptoms.
Without any outward signs prompting investigation, the condition can remain undetected for years, silently increasing the risk of long-term complications.
These individuals might only be identified through screening, often triggered by a family history of celiac disease or the presence of another autoimmune condition.
In essence, the diagnostic challenge arises from the fact that celiac disease doesn’t always present in the textbook manner which underscores the critical importance of increased awareness and comprehensive testing strategies.
Hope to expand your knowledge on heart diseases? This article on knowing the characteristics of heart disease has all the details you need!
Living with Celiac Disease
Embracing a gluten-free lifestyle is the fundamental strategy for managing celiac disease and reclaiming your well-being.
It’s about understanding that even the smallest exposure to gluten can have significant consequences for your health, making vigilance a constant companion.
1. What a Gluten-Free Life Really Means
When we say “gluten-free,” it’s easy to immediately think of eliminating bread, pasta, and obvious wheat-based products. However, for individuals with celiac disease, the reality is far more nuanced.
A truly gluten-free diet demands meticulous attention to detail, because even trace amounts of this protein can ignite the damaging autoimmune response in the small intestine.
It includes complete avoidance to allow the gut to heal and prevent further complications.
2. Food with Hidden Gluten

Besides food, another challenge lies in the fact that gluten is a surprisingly versatile ingredient and can be insidiously hidden in a vast array of products you might not suspect.
Gluten can be a silent contributor in:
- Beverages like processed drinks or even beer
- Cosmetics and personal care products
- Medicine, vitamins, and supplements
- Processed foods (e.g. meat substitutes)
- Sauces and dressings (e.g. thickening agents, soy sauce, and creamy dressings)
This underscores the critical need to become a diligent label reader, turning it into an essential habit for safeguarding your health.
3. Decoding food labels effectively
Once you’re familiar with what to look for on packaging, identifying gluten-free options becomes simpler:
- Identify Gluten-Containing Ingredients: Be on high alert for the explicit mention of wheat, including its various forms (e.g., durum, semolina, spelt, kamut), barley, rye, and malt.
- Beware of “May Contain” Warnings: These statements, such as “may contain wheat” or “processed in a facility that also processes wheat,” indicate a risk of cross-contamination during the manufacturing process. While the product itself may not contain gluten ingredients,the potential for trace amounts is present, and individuals with celiac disease often need to avoid these products as well.
- Seek Certified Gluten-Free Labels: Many countries and organisations have certification programs for gluten-free products. Looking for these official seals of approval can provide an added layer of assurance that the product meets strict gluten-free standards (typically less than 20 parts per million of gluten). This can significantly simplify your grocery shopping.

3. Protecting Your Gluten-Free Lifestyle
Even if you are meticulous about choosing gluten-free foods, cross-contamination can unknowingly introduce gluten into your diet. This can happen both within your own kitchen and when eating out:
At Home: Implement strict protocols by:
- Using separate cutting boards – one for gluten-free and one for gluten-containing items.
- Investing in a dedicated gluten-free toaster.
- Maintaining separate utensils (knives, spoons, forks) or washing them thoroughly before using them for gluten-free preparation.
- Being mindful of shared condiments (e.g., butter, jams) where crumbs can easily transfer. Consider using squeeze bottles or individual portions.
- Cleaning kitchen surfaces and appliances thoroughly to remove any gluten residue.
Eating Out: This requires careful communication and trust:
- Inform your server that you have celiac disease and need a completely gluten-free meal due to a medical condition.
- Ask detailed questions about food preparation methods to ensure your food won’t come into contact with gluten-containing ingredients or surfaces.
- Inquire about dedicated gluten-free preparation areas and utensils.
- Be cautious with fried foods, as shared fryers are a common source of cross-contamination.
- Don’t hesitate to politely decline a dish if you are unsure about its gluten-free status.
Diagnosis and Treatment
Effectively managing celiac disease extends beyond simply adopting a gluten-free diet with consistent and collaborative ongoing medical care to address potential complications and fine-tune your management plan.
This includes:
- Monitoring your nutrient deficiencies through regular blood tests where essential vitamins and minerals like iron, folate, vitamin B12, and vitamin D are tested.
- Follow up with your Gastroenterologist on your progress, manage any persistent symptoms, and screen for potential complications.A dietician
- Specialised testing like serology testing (looks for antibodies in blood) or genetic testing for individuals with refractory (not responding to a gluten-free diet) or nonresponsive celiac disease.
If the initial tests suggest the possibility of celiac disease, your doctor will likely order either endoscopy or capsule endoscopy for test confirmation.
Living Well with Celiac Disease: A Food-Focused Approach
Adopting a gluten-free lifestyle requires adjustments in various aspects of your life. Here’s a breakdown to help you going:
- Committing to a Strictly Gluten-Free Diet
It’s not a temporary fix but a lifelong commitment to eliminating all sources of gluten from your diet that requires meticulous attention to food labels, understanding ingredient lists, and being aware of hidden gluten in processed foods.
It’s about becoming an informed consumer and making conscious choices with every meal and snack.
- Preventing Cross-Contaminations
Gluten can be a sneaky adversary, lurking in unexpected places. Cross-contamination, the unintentional transfer of gluten to gluten-free foods, is a significant concern. This demands meticulous practices in your kitchen – using separate cutting boards, toasters, and utensils; cleaning surfaces thoroughly; and being mindful of shared condiments.
- Traveling Gluten-Free with Confidence
Travel doesn’t have to be a source of anxiety. With proactive planning, you can explore the world while staying safe. This involves researching gluten-free dining options at your destination, perhaps contacting restaurants in advance.
You can even pack your own supply of trusted gluten-free snacks during transit or in situations with limited options. Online resources and gluten-free travel communities can offer invaluable tips and recommendations.
- Emotional Support and Mental Health
Living with a chronic condition like celiac disease can bring emotional challenges. The constant vigilance required, potential social limitations, and the impact on daily routines can sometimes lead to feelings of frustration, anxiety, or even isolation.
Seeking support from family, friends, or celiac support groups can provide a sense of community and understanding. If you find yourself struggling with persistent negative emotions, don’t hesitate to reach out to a mental health professional for guidance and coping strategies.
- Building a Supportive Ecosystem
It is important to help your family, friends, and colleagues understand the importance of your gluten-free diet. You can do that by explaining what it is, where it’s found, and the potential health consequences of accidental exposure.
This education empowers them to support you effectively in social situations and within your shared living spaces, minimising the risk of cross-contamination and fostering a more understanding environment.
When Should You Seek Medical Advice? Recognising Important Signals
While managing celiac disease primarily involves dietary adherence, certain situations warrant seeking professional medical advice:
- Persistent digestive symptoms (e.g. diarrhea, bloating, and abdominal pain)
- Emergence of new or worsening non-digestive symptoms (e.g. persistent fatigue, unexplained anemia, new skin rashes, or joint pain)
- If you have a family history of celiac disease
- Continued or worsening symptoms despite a gluten-free diet
- Signs of nutritional deficiencies (e.g. persistent fatigue, weakness, or other signs that might suggest vitamin or mineral deficiencies)
- Childhood growth problems or delayed puberty
Meet with Our Celiac Disease Experts
Island Hospital boasts a team of dedicated gastroenterology specialists committed to providing exceptional care. Our specialists stay abreast of the latest advancements in celiac disease management and utilise state-of-the-art technology to ensure accurate diagnoses and effective treatment plans.

We’re offering our comprehensive Executive Health Screening Package at only RM760 – giving you a complete head-to-toe health assessment for peace of mind.
Our package features vital health screenings, including Cardiovascular Assessment, Full Blood Picture, Radiological Screening, Diabetes Screening, Kidney Function Test, and much more.
What’s Included in Your Screening Experience:
✔ Physical examination
✔ Complete medical report
✔ Consultation by Health Screening Physician/Specialist
✔ Choice of light refreshments
✔ Exclusive Island Hospital woven bag
Still have questions? Schedule an appointment with us today and let us help you with your treatment plan.
FAQ
Is celiac disease hereditary?
Yes, celiac disease has a strong hereditary component. This means it tends to run in families. Celiac disease is not solely caused by genes, but certain genes significantly increase a person’s risk of developing it.
The most commonly associated genes are the HLA-DQ2 and HLA-DQ8 genes. These genes are involved in the immune system.
Individuals who have a first-degree relative (parent, child, or sibling) with celiac disease have a significantly higher risk of developing the condition, estimated to be around 1 in 10. This is much higher than the general population risk of about 1 in 100.
What tests are needed to diagnose celiac disease?
There are a couple of tests carried out to diagnose celiac disease. Other than genetic testing, blood tests, and small intestine biopsy through endoscopy, skin biopsy is also another method to diagnose celiac disease.
If you have a rash called dermatitis herpetiformis, which is strongly associated with celiac disease, your doctor may perform a skin biopsy to look for specific antibody deposits. A positive skin biopsy can sometimes be enough to diagnose celiac disease without the need for an intestinal biopsy.
Am I supposed to start a gluten-free diet before testing?
No, absolutely not! It is crucial that you continue to eat a diet containing gluten until all the necessary tests for celiac disease are completed.
For accurate diagnosis, it’s essential to undergo celiac disease testing before adopting a gluten-free diet. Removing gluten from your diet beforehand can cause blood test results to fall within the normal range, potentially masking the presence of the condition.
What foods should I absolutely avoid if diagnosed?
Upon receiving a medical diagnosis, dietary adjustments often become necessary to aid recovery and alleviate symptoms. Just as avoiding spicy and fried foods can prevent digestive upset during a fever, managing other conditions requires specific food restrictions.
For tailored dietary guidance that aligns with your unique diagnosis and health status, consulting a healthcare professional or a registered dietitian is paramount.
How soon can I see improvement after going gluten-free?
The timeline for seeing improvement after starting a gluten-free diet can vary from person to person, but here’s a general idea of what to expect.
After starting a strict gluten-free diet following a celiac disease diagnosis, many people experience initial relief from digestive and other symptoms within days to weeks.
Continued improvement, including better nutrient absorption, typically occurs within weeks to months. However, complete healing of the small intestine can take months to years, particularly in adults.
Strict adherence to the gluten-free diet and avoidance of cross-contamination are crucial for effective healing and long-term health.
Factors like the severity of initial damage, individual healing rates, and age can influence the timeline. It’s important to be patient and consult a healthcare professional if improvement is not as expected.