
08 Oct Can PCOS Cause Infertility? What You Need to Know
Can PCOS Cause Infertility? What You Need to Know
By Island Hospital | October 8, 2025 10:34:09 AM
Being diagnosed with polycystic ovary syndrome (PCOS) can be overwhelming. The irregular or absent periods, excessive hair growth (hirsutism), stubborn acne, weight gain, and emotional challenges such as depression and anxiety can already make day-to-day life feel like an uphill climb.
Add to that the hope of starting a family, and the journey can become even more daunting. For many women, PCOS turns the path to parenthood into an emotional rollercoaster — filled with uncertainty, false starts, and countless questions. As worrisome as this can be, you’re far from alone.
PCOS affects roughly 1 in 10 women of reproductive age, making it one of the most common causes of infertility worldwide. Yet here’s the encouraging truth: with the right medical care and lifestyle adjustments, up to 80% of women with PCOS are able to conceive.
In this article, we’ll explore how PCOS affects fertility, the treatment options available, and the practical steps you can take to improve your chances of conception so that you can move forward on your journey with clarity, hope, and confidence.
What is PCOS
Polycystic ovary syndrome (PCOS) is a common hormonal disorder that affects women of reproductive age. While the exact cause isn’t fully understood, it’s believed to result from a combination of genetic and environmental factors.
In PCOS, the ovaries produce higher-than-normal levels of androgens (male hormones), which can disrupt the menstrual cycle and interfere with ovulation.
PCOS can also cause:
- Irregular or absent periods – due to infrequent or absent ovulation.
- Ovarian cysts – multiple small, fluid-filled sacs on the ovaries (common, but not present in every case).
- Excess androgen symptoms – such as hirsutism (unwanted hair growth on the face or body), acne, and thinning scalp hair.
- Metabolic concerns – including insulin resistance, weight gain, and a higher risk of developing type 2 diabetes.
These hormonal imbalances can prevent the ovaries from releasing an egg each month (anovulation), making it harder to conceive naturally. However, with the right medical care, lifestyle adjustments, and sometimes fertility treatments, many women with PCOS go on to have healthy pregnancies.
Do I Have PCOS?
PCOS can look different for every woman, and many only have mild symptoms. Sometimes these symptoms are so subtle that they go unnoticed until trying for a baby.
This is especially true if you’ve been using hormonal contraception. While on the pill, the bleeding you experience isn’t true ovulation but a withdrawal bleed caused by the hormones, which can mask the irregular cycles PCOS often causes.
If you’re wondering whether you might have PCOS, think about whether you’ve experienced any of the following:
- Irregular or missed periods (menstrual cycles shorter than 21 days, longer than 35 days, or absent for months at a time)
- Changes in skin health, such as persistent acne or oily skin
- Increased hair growth on the face, chest, stomach, or back
- Thinning hair or hair loss from the scalp
- Gradual weight gain or difficulty losing weight despite a healthy lifestyle
- Darkened patches of skin, often around the neck, underarms, or groin
- Difficulty getting pregnant after trying for several months
If two or more of these symptoms feel familiar, it’s worth speaking to a healthcare provider. Only a medical professional can diagnose PCOS, usually through a combination of your medical history, physical examination, hormone testing, and ultrasound scans of the ovaries.
Ready to take the stress out of preparing for parenthood? Dive into our comprehensive maternity guide, where Island Hospital’s experts walk you through every stage, from pregnancy expectations to newborn care.
How PCOS Affects Fertility
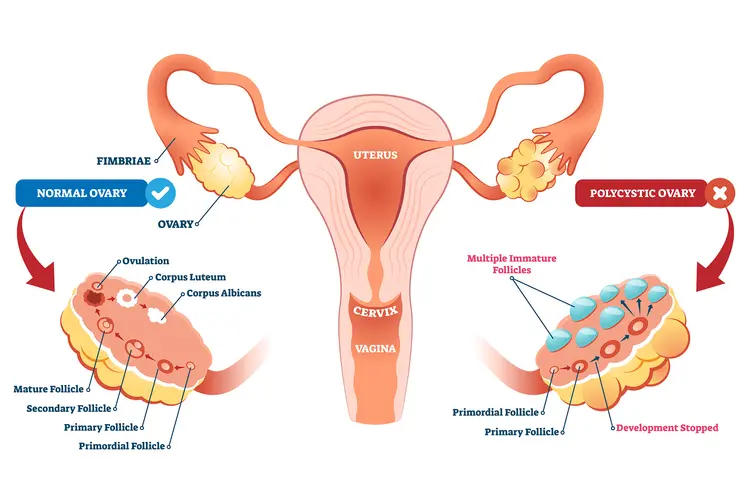
PCOS is one of the leading causes of infertility in women, largely because it disrupts ovulation, the process by which an ovary releases an egg each month. In a healthy menstrual cycle, the ovaries contain many small sacs called follicles, each holding an immature egg (ovum).
Typically, one follicle grows and matures, then releases its egg into the fallopian tube during ovulation. With PCOS, this process doesn’t happen regularly. The follicles often fail to mature or release an egg, meaning ovulation may occur infrequently or not at all.
Instead, these underdeveloped follicles can accumulate in the ovaries, which may appear as “many cysts” on an ultrasound scan, hence the name polycystic ovary syndrome. Without regular ovulation, it becomes much harder to conceive naturally.
The main ways PCOS interferes with fertility include:
1. Irregular or absent ovulation
High levels of androgens and disrupted reproductive hormones can prevent the release of a mature egg, reducing the chances of fertilisation.
2. Poor egg quality
Infrequent ovulation can result in eggs that don’t mature properly, making fertilisation and a healthy pregnancy less likely.
3. Insulin resistance
Many women with PCOS have insulin resistance, which can lead to higher insulin levels in the blood. This not only impacts weight and metabolism but also worsens hormonal imbalance, making ovulation less frequent.
4. Endometrial changes
Irregular cycles can cause the lining of the uterus (endometrium) to build up excessively or at the wrong time, making it less receptive for implantation of a fertilised egg.
Although this may sound discouraging, having PCOS doesn’t mean you can’t have children. With targeted treatment, from lifestyle changes to ovulation-inducing medication, and in some cases, assisted reproductive techniques like IUI or IVF, many women with PCOS successfully conceive.
Management and Treatment Options for PCOS
The right treatment for PCOS isn’t the same for everyone; it depends on your symptoms, medical history, other health conditions, and whether or not you’re trying to get pregnant.
Your doctor will also consider factors such as your age, the severity of your symptoms, how long you’ve been experiencing them, and your fertility goals. In many cases, treatment involves a combination of medication and lifestyle changes to address both the symptoms and the underlying hormonal imbalance.
If you’re not currently planning to get pregnant
If you’re not currently trying for a baby, treatment typically focuses on managing symptoms, regulating menstrual cycles, and reducing long-term health risks like diabetes and heart disease. These options are generally non-surgical and may include:
- Hormonal birth control – Pills, patches, vaginal rings, hormonal IUDs, or injections can help regulate cycles, reduce menstrual pain, improve acne, and control excess hair growth.
- Insulin-sensitising medication – Metformin, commonly used to treat type 2 diabetes, can help the body process insulin more effectively, which can improve cycle regularity and support weight management.
- Anti-androgen medications – Certain drugs can block the effects of excess male hormones to help reduce unwanted hair growth and acne.
- Lifestyle adjustments – A balanced diet, regular exercise, and maintaining a healthy weight can significantly improve insulin sensitivity and hormonal balance.
If you are trying to get pregnant now or in the near future
When pregnancy is your goal, treatment is tailored to improve ovulation and maximise your chances of conception. Your doctor will assess how long you’ve been trying, your age, and any additional fertility factors before recommending options such as:
- Ovulation-inducing medication – Clomiphene citrate or letrozole are often prescribed to stimulate ovulation. If oral medications aren’t effective, gonadotropin injections may be used instead.
- Ovarian drilling (surgery) – In rare cases, a surgical procedure can be used to restore ovulation by reducing androgen-producing tissue in the ovaries. This is less common now due to the effectiveness of newer medications.
- Intrauterine Insemination (IUI) – If ovulation induction alone is not successful, IUI can be used, sometimes in combination with medication. This procedure places sperm directly into the uterus at the optimal time in your cycle.
- In Vitro Fertilisation (IVF) – If other treatments fail, IVF may be an option. This involves retrieving eggs, fertilising them in a lab, and transferring embryos into the uterus. IVF has high success rates for many women with PCOS, particularly those under 35.
Wondering if it’s the real thing or just PMS? Discover 14 early pregnancy signs that could give you clearer clues—feel more confident before reaching for that test.
Lifestyle Changes to Improve Fertility with PCOS
Medication is often important in treating PCOS, but it’s not the only tool. Small, consistent lifestyle changes can make a big difference, helping to regulate cycles, balance hormones, and improve fertility.
1. Diet
A PCOS-friendly diet doesn’t mean restriction. It’s about choosing foods that help keep your blood sugar and insulin levels stable.
- Opt for low glycemic index (GI) foods: Whole grains, legumes, non-starchy vegetables, and most fruits keep blood sugar steady and reduce insulin spikes.
- Limit refined carbs and added sugars: Processed snacks, white bread, and sugary drinks can worsen insulin resistance and make symptoms more complicated to manage.
- Add lean proteins and healthy fats: Foods like eggs, fish, poultry, nuts, seeds, and olive oil support satiety and hormone regulation.
By focusing on whole foods and balancing protein, healthy fats, and complex carbohydrates, you can create meals that naturally support hormone balance and fertility.
For example, something as simple as a yoghurt bowl with fruit and seeds for breakfast, a balanced lunch with lean protein and whole grains, or a dinner built around fish and leafy greens can go a long way toward keeping your cycle on track and boosting your chances of conception.
2. Exercise

Regular physical activity helps improve insulin sensitivity, support weight management, and reduce androgen levels.
- Aim for at least 150 minutes per week of moderate exercise like brisk walking, cycling, or swimming.
- Strength training (e.g., bodyweight workouts, resistance bands, or weights) can be especially effective at improving insulin response and supporting healthy ovulation.
- The key is consistency. Pick activities you enjoy, so they become a sustainable part of your routine.
3. Weight Management

For women with PCOS who are overweight, even a modest weight loss of 5–10% of body weight can significantly improve menstrual regularity and the likelihood of ovulation. The goal doesn’t have to be drastic — small, gradual changes in eating and movement often make the most significant long-term impact.
4. Sleep and Stress Management
Sleep and stress are closely tied to hormone health. Poor sleep can worsen insulin resistance, while chronic stress raises cortisol, which further disrupts the delicate hormonal balance in PCOS
- Prioritise quality sleep: Aim for 7–9 hours each night, with consistent sleep and wake times.
- Practice stress-relieving habits: Meditation, yoga, journaling, or even daily walks can calm the nervous system.
- Build emotional resilience: Counselling, support groups, or talking with others who share your journey can help manage the anxiety and uncertainty that often come with PCOS.
Emotional Support and Mental Well-being
Living with PCOS while navigating fertility challenges isn’t just a physical journey; it can also take a significant emotional toll.
The stress of irregular cycles, repeated disappointments, and uncertainty about the future can leave many women feeling anxious, isolated, or overwhelmed. Acknowledging these emotions is just as important as managing the physical symptoms.
Coping Strategies and Everyday Tools
- Journaling – Writing down feelings, tracking symptoms, or simply reflecting can help release stress and provide perspective.
- Support groups – Whether online or in person, connecting with others who share the same challenges can ease feelings of isolation and offer encouragement.
- Therapy & counselling – Speaking with a mental health professional can provide strategies for coping with anxiety, depression, or the strain of infertility treatments.
Planning for the Long-Term
Fertility journeys with PCOS can sometimes require patience and multiple attempts. Thinking ahead can make the process feel less overwhelming:
- Egg freezing – For women who aren’t ready to conceive right away, this can provide peace of mind by preserving fertility for the future.”
- Treatment pacing – Working with your doctor to plan realistic timelines and breaks between treatment cycles can help protect both your emotional and physical health.
- Managing expectations – Understanding that some women may need several treatment rounds can reduce frustration and help you stay resilient.
Support at Island Hospital
At Island Hospital, care extends beyond medication and procedures. Our team is here to support your whole well-being — physically, emotionally, and mentally, with counselling and patient services to help you manage the challenges of PCOS and infertility. physical and emotional aspects of PCOS.
Whether it’s through one-on-one counselling, group sessions, or access to trusted resources, you’ll have a support system to lean on throughout your fertility journey.
Take the first step today, reach out to us, and let’s walk this journey together!
Ready to Boost Your Chances of Conception?
Living with PCOS can feel overwhelming, but you don’t have to face the journey alone. At Island Hospital, we combine over 20 years of specialist fertility care with advanced diagnostics like hormone testing, IVF, IUI, and personalised treatment plans tailored to your unique needs.
Our dedicated team of gynaecologists, equipped with the latest technology, ensures you receive an accurate diagnosis and compassionate guidance at every step. From regulating cycles and improving egg quality to advanced fertility treatments like ovulation induction, IUI, or IVF, we’re here to support every aspect of your journey.
With success rates of up to 65–75% for PCOS patients in leading fertility clinics, there’s every reason to feel hopeful.
Take the first step toward parenthood today — book your consultation at our Fertility Centre with our experienced gynaecologists, and let us help turn your dream of starting a family into reality.
Take Proactive Action Today – Get a Comprehensive Health Screening

We’re offering our Comprehensive Plus Package (Female) at only RM2,799 – giving you a complete head-to-toe health assessment for peace of mind.
Our package includes vital health screenings, such as Gynaecological Assessment, Radiological Screening, Cardiovascular Assessment, Urine Assessments, and more.
What’s Included in Your Screening Experience:
✔ Physical examination
✔ Complete medical report
✔ Consultation by Health Screening Physician/Specialist
✔ Choice of light refreshments
✔ Exclusive Island Hospital woven bag
Note: If you are pregnant or think you might be, please be sure to inform our staff.
FAQs
1. Is PCOS fertility treatment worth it?
Fertility treatment can feel like a big commitment, but for many women with PCOS, it’s one of the most effective ways to achieve pregnancy. Think of it as an investment in parenthood.
In Malaysia, the cost of PCOS fertility treatment can vary depending on the approach. Fertility tests typically range between RM400 and RM2,000, while ovulation-inducing medications are generally more affordable and often used as a first-line option.
For couples who need more advanced interventions, IVF can cost between RM20,000 and RM30,000 per cycle.
Despite these costs, the benefits can be significant:
- Success rates for IVF in PCOS patients are around 65–75% in leading clinics.
- Less invasive treatments (like lifestyle changes and ovulation-inducing meds) can restore natural cycles and increase pregnancy chances.
- Managing PCOS through treatment also reduces long-term risks of type 2 diabetes, metabolic syndrome, and endometrial issues.
2. Can I conceive naturally with PCOS?
Yes. Many women with PCOS are able to conceive naturally, particularly in milder cases. However, because PCOS often disrupts ovulation, studies suggest that up to majority of women will need some form of medical support to achieve pregnancy.
The good news is that treatments such as ovulation-inducing medications and lifestyle changes are very effective. If you’re trying naturally, preparing your body by tracking cycles, eating a balanced diet, exercising regularly, and reducing caffeine intake can help boost your chances.
3. Are fertility treatments for PCOS safe?
Yes. Fertility treatments, including hormone therapies like clomiphene, letrozole, or gonadotropins, are considered very safe — around 95% of women tolerate them well when properly monitored by a fertility specialist.
Side effects can occur (such as bloating, mood changes, or, rarely, ovarian hyperstimulation), but your doctor will closely track your response to minimise risks.
You can prepare for treatment by keeping a healthy weight, limiting alcohol, avoiding smoking, and managing stress levels to support your body through the process.
4. How long does it take to get pregnant after starting treatment?
The timeline varies depending on the type of treatment, your age, and your overall health. For some women, ovulation-inducing medications like clomiphene or letrozole can trigger ovulation within the first few cycles, and pregnancy may happen in as little as 3–6 months.
For others, especially those who need more advanced options like IVF, it may take several months of preparation and multiple cycles before achieving success. On average, many women with PCOS who pursue treatment conceive within 6–12 months of starting.
5. What happens if my first treatment fails?
It’s important to know that needing more than one attempt is common and not a sign that you won’t succeed. If the first treatment doesn’t work, your doctor may adjust the dose of ovulation-inducing medication, switch to a different drug, or recommend moving on to gonadotropin injections, IUI, or IVF depending on your profile.
Lifestyle support (like improving nutrition, weight management, and reducing stress) is usually encouraged alongside medical treatment, since it can increase the success of future cycles. Fertility specialists often remind patients that PCOS treatments are highly effective, but sometimes require persistence and tailored adjustments.






