04 Jul When Does Pancreatitis Require Surgery? Signs, Options, and Expert Insights
When Does Pancreatitis Require Surgery? Signs, Options, and Expert Insights
By Island Hospital | July 04, 2025 10:10:00 AM
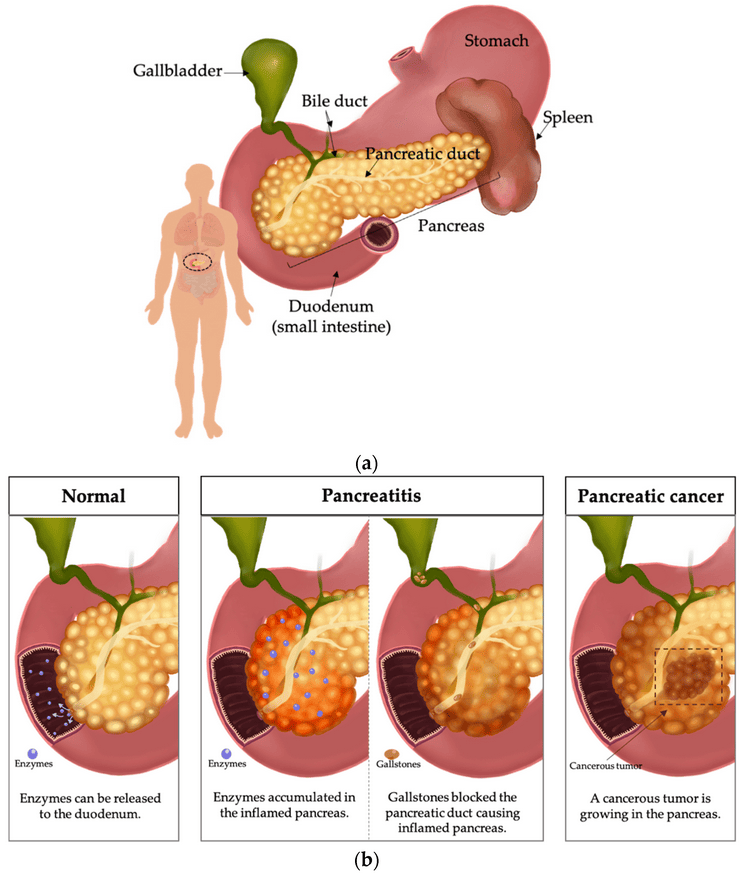
Hearing the word “pancreatitis” might sound a bit daunting at first, but think of it simply as an inflammation of the pancreas – a challenge your body might face.
The good news is, for many, this journey begins with straightforward medical care, focusing on positive lifestyle tweaks, delicious dietary adjustments, and helpful medications.
But for those times when these conventional helpers need a boost, surgical intervention can be a true game-changer, not just a possibility, but a vibrant step forward to renewed health and a thriving quality of life.
Consider this article your helpful companion, guiding you through when surgery for pancreatitis might be the right choice, what an empowering process it can be, and how making timely decisions can truly open the door to incredible improvements.
Why Many Patients Delay Addressing Surgical Needs
It’s natural to feel apprehension when faced with the prospect of surgery. Common fears include the invasiveness of the procedure, the recovery period, potential complications, and the uncertainty of life post-surgery.
Much of the widely available information, and even initial consultations, often emphasises the causes of pancreatitis and general medical treatments, inadvertently downplaying the potential for surgical needs.
However, delaying necessary surgical intervention for chronic or severe pancreatitis can have profound and debilitating effects on daily life.
Patients often endure ongoing, persistent pain, a constant fear of eating due to potential flare-ups, frequent and often prolonged hospital visits, and significant nutritional deficiencies.
This constant burden can severely impact their physical and mental well-being, transforming simple daily activities into challenging endeavors. Understanding the severe impact of untreated pancreatitis can be a powerful motivator for seeking the right treatment at the right time.
Speak with your health professional today if you face any concerning symptoms that seem abnormal.
Early detection is the key to preventing serious health problems. Check out Island Hospital’s comprehensive screening services in this article.
Clear Signs That Surgery Might Be Needed
While pancreatitis is typically managed initially with conservative measures like lifestyle and dietary modifications, medication, and enzyme supplements, certain signs indicate that surgery may be the most appropriate course of action.
It’s essential to recognise the following indicators and discuss them thoroughly with your medical team. Some clear signs that may require surgery include:
1. Persistent Pain Beyond 4-6 Weeks
Severe abdominal pain is one of the hallmarks of pancreatitis. When this discomfort continues relentlessly for weeks despite conservative treatments, it often signals a more entrenched problem that may benefit from surgical intervention.
This sustained discomfort significantly impacts quality of life and indicates that the underlying inflammation or other complications is not resolving on its own.
2. Recurring Acute Attacks
For some individuals, pancreatitis manifests as repeated acute flare-ups. If these attacks become frequent and severe, even with adherence to medical management, surgery may be considered to address the root cause of the recurring inflammation or to manage complications that predispose to these attacks.
3. Potential Complications
Pancreatitis can stem from various identified causes; however, in certain cases, the underlying reason remains elusive, leading to a diagnosis of idiopathic pancreatitis.
As pancreatitis becomes more severe, additional symptoms like fever and chills, dehydration, and even abnormal heart rhythm (tachycardia) may develop.
If left untreated for a long time, it leads to more life-threatening and serious complications such as:
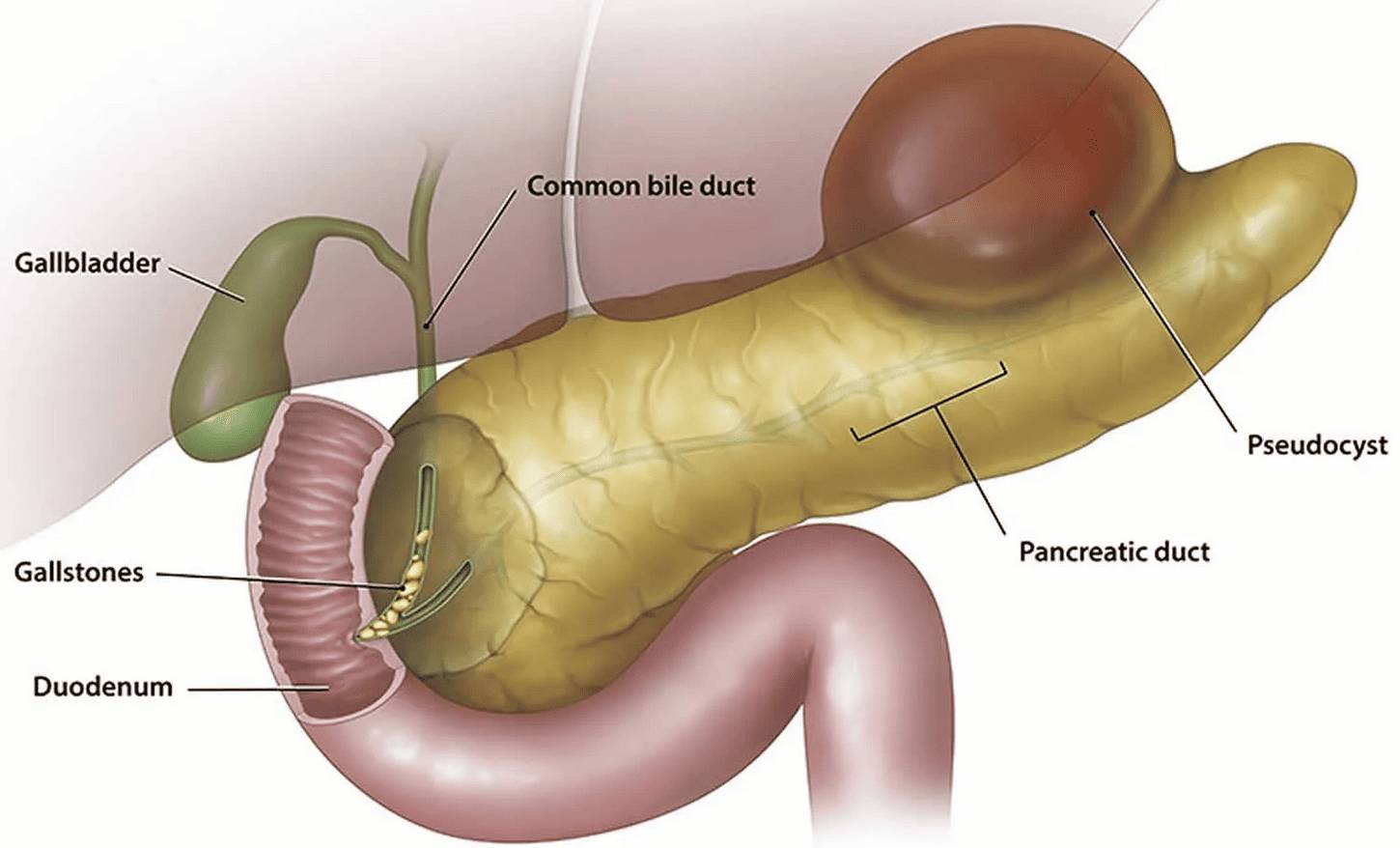
- Pseudocysts
These are fluid collections that form around the pancreas when pancreatic fluids leak from the pancreatic ducts due to injury or inflammation. It normally occurs after an episode of pancreatitis, which can be acute (sudden) or chronic (long-term).
While some resolve on their own, large, symptomatic, or infected pseudocysts often require drainage, which can be performed surgically.
- Necrosis
Necrosis refers to the death of pancreatic tissue due to severe inflammation and this happens from contracting acute pancreatitis. For individuals with necrotising pancreatitis, infection poses the most serious risk, developing in up to 20% of cases.Infected necrosis is a life-threatening complication that almost always requires surgical removal of the dead tissue to prevent further infection and sepsis. - Infected Tissue
Any infection within or around the pancreas is a serious concern and often necessitates surgical debridement (removal of infected tissue) to control the infection and prevent its spread. - Pancreatic Cancer
Acute pancreatitis may be a temporary infection and the pancreas is designed to heal on its own.

However, in another worse case scenario, as this inflammation persists over an extended period, it can lead to chronic pancreatitis, which is unfortunately a known significant risk factor for developing pancreatic cancer. This isn’t a direct cause-and-effect in every case, but rather a heightened susceptibility.
4. Bile or Pancreatic Duct Obstruction
Inflammation or scarring from pancreatitis can block the bile duct (leading to jaundice) or the pancreatic duct (impairing enzyme flow).
Such obstructions can worsen pain and lead to further complications, often requiring surgical or endoscopic procedures to relieve the blockage.
Weighing the Options Between Surgical vs. Non-Surgical Approaches
The decision between surgical and non-surgical approaches is a complex one, with distinct pros and cons for each.
It remains crucial that you consult your medical professional before making any informed decision to proceed with either approach.
Let’s have a look at the options:
| Features | Non-Surgical (Conservative) Care | Surgical Intervention |
|---|---|---|
| Typical Approach | Primarily involves medical management. | Involves operative procedures. |
| Key Components | Pain management, intravenous fluids, dietary restrictions, enzyme supplements, and managing underlying causes (e.g., gallstones, alcohol abuse). | Procedures designed to directly address structural problems within the pancreas or surrounding areas. |
| Pros |
|
|
| Cons |
|
|
| When Considered | In cases of mild acute pancreatitis. | When conservative care has failed to resolve symptoms or prevent recurrence |
| Doctors' Recommendation |
|
|
Island Hospitals’ Gastroenterology FAQs provide valuable insights into common digestive concerns and offer expert guidance on nurturing a healthy gut for optimal well-being. Dive into the details here!
Who Should You Consult? Your Partners in Care at Island Hospital
When navigating the complexities of pancreatitis, consulting with specialists experienced in digestive disorders is of utmost importance. Island Hospital Digestive Care proudly boasts a renowned Gastroenterology team that is dedicated to providing you with exceptional services and supporting your speedy recovery throughout your entire journey.

Our team is equipped with the latest diagnostic and treatment technologies to ensure accurate diagnoses and effective interventions to help you find relief and improve your quality of life.
We pride ourselves on our patient-centric approach, evidenced by positive patient reviews and our commitment to adopting advanced techniques. Our specialists work collaboratively to develop individualised treatment plans, ensuring you receive the most appropriate and effective care for your specific condition.
Types of Pancreatic Surgery & What They Address
Pancreatic surgery encompasses various procedures, each tailored to address specific complications or aspects of pancreatitis. Here are the following examples of surgeries for each types:
1. Pancreatic Drainage Procedures
Pancreatic drainage procedures are one of the most common ones to address pancreatitis where it is performed to drain pseudocysts or to relieve blockages in the pancreatic duct. The procedure may involve endoscopic drainage (using a scope to place a stent) or open surgical drainage.
2. Pancreatectomy (Partial or Full Removal)
- Partial Pancreatectomy: The removal of a portion of the pancreas. This is often done for localised chronic pancreatitis, tumors, or severe necrosis in a specific area.
- Total Pancreatectomy: The removal of the entire pancreas. This is a rare and major surgery, typically reserved for widespread severe disease or certain types of pancreatic cancer, leading to lifelong insulin and enzyme dependence.
3. ERCP with Stenting (Endoscopic Retrograde Cholangiopancreatography)
ERCP with stenting is a minimally invasive endoscopic procedure used to diagnose and treat problems in the bile and pancreatic ducts.
Stenting can be placed to open blockages, allowing bile and pancreatic fluids to flow properly especially when it is caused by stones or strictures.
For a more detailed process of how ERCP works, check out this YouTube video.
Each surgery carries its own set of risks, including bleeding, infection, leakage from surgical sites, and potential long-term issues.
However, when performed by experienced surgeons for appropriate indications, the outcomes can significantly improve a patient’s quality of life, alleviating pain and preventing life-threatening complications.
Life After Surgery
Undergoing pancreatic surgery is a significant event, and understanding the recovery process is crucial for a smooth transition back to normalcy. Here’s what to expect after this stage:
1. Typical Recovery Timeline
- Hospital Stay: Your stay in the hospital varies depending on the type of surgery you undergo, but it typically ranges from several days to a week or more for more extensive procedures. During this time, pain management, fluid balance, and monitoring for complications are prioritised.
- Healing Period: Full recovery can take several weeks to a few months. You will foresee a gradual increase in activity levels and return to your usual routines after this period.
2. Dietary Adjustments and Enzyme Supplements
Dietary changes particularly after a pancreatectomy surgery are often necessary for better digestion.
This includes having:
- 6-8 smaller, more frequent meals a day that is spaced 2-3 hours apart
- low-fat foods from healthy sources such as olive oil, canola oil, peanut oil, nuts, seeds and avocados
- and avoiding or consuming small quantities of trigger foods like fried or greasy foods
- small sips of fluids (6-12 cups of fluids a day) or drinking beverages containing calories, nutrients, and protein
Many patients, especially those who have undergone partial or total pancreatectomy, will require lifelong pancreatic enzyme replacement therapy (PERT) to aid in digestion and nutrient absorption.
3. Return to Normal Life
The goal of surgery is to restore normalcy and for many patients, this means pain-free eating, a significant reduction in flare-ups, improved nutrition, and an overall enhanced quality of life that was previously hindered by chronic pain and fear.
Get Ready For Relief!
Facing pancreatitis can be hard, but positive change is absolutely possible with the right intervention. Don’t let symptoms linger if non-surgical options aren’t helping – sometimes, a different approach is exactly what’s needed.
When you’re ready, Island Hospital’s expert Digestive Centre team is here, fully equipped and ready to provide the exceptional care and support you need for a smooth recovery journey.
FAQ
Does surgery completely cure pancreatitis?
No, undergoing a surgery does not always completely cure pancreatitis as it does depend on the type and cause of it:
- Acute Pancreatitis: If acute pancreatitis is caused by an identifiable problem like gallstones blocking a duct, surgery to remove the gallstones or gallbladder can effectively “cure” that specific episode and prevent recurrence from that cause. However, if the pancreatitis has caused significant, permanent damage (like widespread necrosis), surgery might be needed to remove dead tissue, but it won’t magically restore the pancreas to its original, healthy state.
- Chronic Pancreatitis: For chronic pancreatitis, surgery often aims to manage the condition rather than “cure” it. This means relieving pain, addressing complications like duct blockages or pseudocysts, and improving quality of life. While it can significantly improve symptoms and prevent further damage, the underlying disease (chronic inflammation and scarring) often remains, and patients may still require ongoing medical management.
When is pancreatic surgery necessary?
Pancreatic surgery becomes necessary when non-surgical treatments aren’t enough to manage symptoms or when serious complications arise. Common scenarios include:
- Gallstone pancreatitis
- Severe acute pancreatitis with complications
- Chronic pancreatitis
- Suspected cancer
How do you know if your pancreas is failing?
“Pancreatic failure” can refer to different aspects:
- Exocrine Failure (Digestive): This means the pancreas isn’t producing enough digestive enzymes. The symptoms you should look out for are:
- Weight loss despite eating normally.
- Oily, foul-smelling stools (steatorrhea) that may float or are difficult to flush, due to undigested fat.
- Diarrhea and abdominal bloating/cramping after meals.
- Nutrient deficiencies (especially fat-soluble vitamins A, D, E, K).
- Endocrine Failure (Hormonal/Blood Sugar): This means the pancreas isn’t producing enough insulin, leading to diabetes. Symptoms include:
- Increased thirst
- Frequent urination
- Unexplained weight loss
- Increased hunger
- Fatigue
- Blurred vision
If you experience these symptoms, especially in the context of known pancreatitis, it’s crucial to consult a doctor for proper diagnosis and management.
Will I need to take enzymes for life?
The need to take enzymes for life depends on the extent of pancreatic damage or removal.
If a significant portion of your pancreas, particularly the part that produces digestive enzymes (exocrine function), is removed during surgery (e.g., a pancreatectomy), or if chronic pancreatitis has severely impaired its function, then lifelong pancreatic enzyme replacement therapy (PERT) is often necessary.
For less extensive surgeries or milder cases of pancreatitis, enzyme supplementation might only be needed temporarily or not at all. Your doctor will monitor your digestive function and advise accordingly.
Can I avoid surgery if I manage my diet?
While diet is crucial, it may not always prevent the need for surgery.
Dietary management is fundamental for both acute and chronic pancreatitis. Eating a low-fat, easily digestible diet, avoiding alcohol, and sometimes eating smaller, more frequent meals can significantly reduce symptoms, prevent flare-ups, and support pancreatic healing.
For mild cases of acute pancreatitis (e.g., due to alcohol or gallstones), diet and lifestyle changes, along with medical management (like pain control and IV fluids), are often sufficient to resolve the episode and prevent recurrence.
However, diet alone cannot correct structural problems like large duct obstructions, severe necrosis, or pseudocysts that are causing significant symptoms or complications. In such cases, surgery is often the most effective or even necessary intervention to address the underlying issue and prevent life-threatening consequences.
Dietary management is a powerful tool in managing pancreatitis, but it’s part of a broader treatment plan. If symptoms worsen despite diligent dietary adherence and other non-surgical interventions, consulting with specialists for a surgical evaluation becomes a crucial step.