
21 Oct Prostate Cancer: Essential Facts You Need to Know
Prostate Cancer: Essential Facts You Need to Know
By Island Hospital | October 21, 2024 12:00:00 PM
Medical Reviewer: Dr Devindran A/L Manoharan, Urologist
“Prostate cancer is only an old man’s disease.”
“If I don’t have symptoms, I can’t have prostate cancer.”
“Screening tests do not help in detecting prostate cancer.”
Are these your preconceptions about prostate cancer? If so, take a moment to read this article. It offers fresh insights that challenge these common misconceptions and provides vital information for men of all ages.
From early detection to treatment and management, we’ll cover all you need to know about prostate cancer.
What is Prostate Cancer?
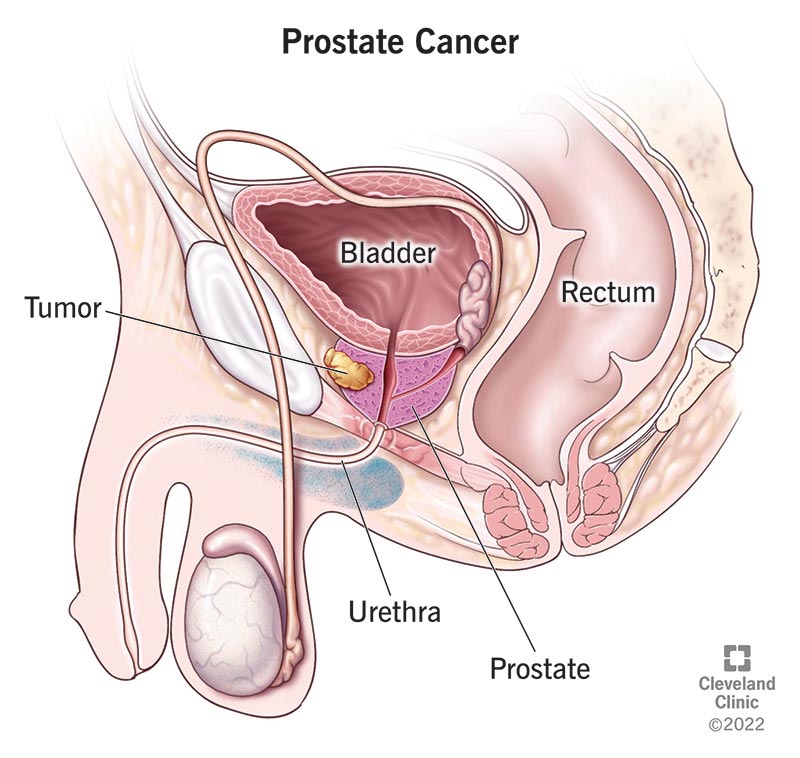
Photo by Cleveland Clinic
Prostate cancer occurs in the prostate – a walnut-sized gland located just below the bladder in men.
The prostate plays a vital role in men’s reproductive health and function. It is responsible for producing seminal fluid and controlling urination and ejaculation.
Prostate cancer typically happens when abnormal cells in the prostate grow uncontrollably. It remains one of the most prevalent and challenging health issues faced by men today – ranking as the second most common cancer in males worldwide!
Types of Prostate Cancer
Prostate cancer is classified based on the cells from which the cancer originates. Here are the main types of prostate cancer:
- Adenocarcinoma
Adenocarcinoma develops in the gland cells of the prostate, making up the vast majority of prostate cancer cases – more than 95%! - Small Cell Carcinoma
This rare type accounts for less than 1% of all prostate cancers. However, it tends to spread quickly to other body parts and is often diagnosed at an advanced stage. - Neuroendocrine Prostate Cancers
These cancers arise from neuroendocrine cells in the prostate, representing less than 2% of all prostate cancers.
Their behaviour varies, with some being slow-growing while others are more aggressive. - Transitional Cell Carcinomas (Urothelial Carcinomas)
These cancers start in the cells lining the urethra, the tube that carries urine out of the body, which runs through the prostate.
Notably, they’re quite rare in the prostate (less than 5% of cases) but more common in the bladder. - Sarcomas
Prostate sarcomas are extremely rare, accounting for less than 0.1% of all prostate cancers.
They develop in the soft tissues of the prostate and tend to grow and spread more quickly than adenocarcinomas.
Stages of Prostate Cancer
Staging prostate cancer typically involves 3 key components:
The Gleason Score
This system measures how aggressive your prostate cancer cells appear under a microscope. It divides prostate cancers into 3 categories:
- A score of 6 or less indicates low-grade cancer, meaning the cells look more like normal prostate tissue. These cancers tend to grow slowly and are less likely to spread.
- A score of 7 is considered an intermediate-grade cancer.
- Scores of 8 to 10 indicate high-grade cancer, meaning the cells look different from normal tissues and are more likely to grow and spread rapidly.
The TNM System
This system provides a comprehensive evaluation of the cancer’s extent by assessing the primary tumour size (T), the lymph node involvement (N), and the presence of distant metastasis (M).
- T is graded from 1 to 4, with higher grades indicating larger tumour size.
- N score ranges from 0 to 3, with higher grades denoting that prostate cancer has spread to the lymph nodes and many of them have been affected.
- M is graded from 0 to 1, with 1 indicating that the prostate cancer has spread to other body parts.
The Number Staging System
Based on the spread extent of prostate cancer, the Number Staging System is utilised to categorise prostate cancer into 4 main stages:
- Stage 1: The cancer cells have grown into tumours in the prostate tissue, but they haven’t spread to the lymph nodes or other body parts.
- Stage 2: The cancer cells have grown into larger tumours. They may have spread to the nearby lymph nodes but not to other body parts.
- Stage 3: The cancer cells have formed tumours and may have spread from the prostate to nearby lymph nodes, seminal vesicles, and other tissues next to the prostate, such as the rectum, pelvis wall, and bladder.
- Stage 4: The cancer cells have spread to distant lymph nodes and other body parts, such as bones.
Symptoms of Prostate Cancer
Most men may not experience any symptoms in the early stage of prostate cancer. However, some early signs to be aware of include:
- Burning sensation or pain during urination
- Difficulty starting or stopping urination
- Frequent urination, especially at night
- Decreased flow of urine
- Blood in urine or semen
- Loss of bladder control
- Erectile dysfunction
- Painful ejaculation
If left untreated, prostate cancer may spread beyond the prostate gland, leading to a host of new symptoms, such as:
- Unexplained weight loss
- Fatigue or general weakness
- Loss of appetite
- Persistent bone pain, particularly in the spine, hips, or ribs
- Fractures from weakened bones
- Swelling of legs or pelvic area
- Numbness or pain in the hands, feet, or legs
- Loss of bowel control
If you’re experiencing any of these symptoms, be sure to consult your doctor.
To learn more about other urologic conditions or warning signs of other urologic cancers, check out these articles:
Risk Factors of Prostate Cancer
Understanding the risk factors of prostate cancer is the key to early detection and prevention. These factors include:
|
|
|
|
|
|
|
|
|
Diagnosis of Prostate Cancer
The diagnosis of prostate cancer involves several key tests aimed at detecting the disease, determining its extent, and guiding treatment options.
Here’s an overview of the primary diagnostic methods used for prostate cancer:
1. Prostate-Specific Antigen (PSA) Test
This blood test measures the level of prostate-specific antigen (PSA). While elevated PSA levels can suggest prostate cancer, they can also be caused by non-cancerous conditions like prostate inflammation.
Therefore, if your PSA level is high, your healthcare provider may recommend additional tests listed below to determine if prostate cancer is present.
2. Digital Rectal Exam (DRE)
During a DRE, your healthcare provider inserts a lubricated, gloved finger into your rectum to feel your prostate for any abnormalities, such as lumps or hard areas.
This exam is often performed alongside the PSA test to provide additional information about the prostate’s condition.
3. Prostate Biopsy
If PSA levels are elevated or abnormalities are detected during a DRE, a prostate biopsy may be recommended. This procedure involves removing small samples of prostate tissue for laboratory examination to check for cancer cells.
The biopsy results are crucial for diagnosing prostate cancer and determining its aggressiveness.
4. Imaging Tests
Imaging tests may also be conducted to assess whether the cancer has spread beyond your prostate:
a) Magnetic Resonance Imaging (MRI): Used to visualise your prostate and surrounding tissues.
b) Computed Tomography (CT) Scan: Helps evaluate the condition of your lymph nodes and other organs.
How is Prostate Cancer Treated?
Prostate cancer treatment varies based on the stage of the disease, the patient’s overall health, and personal preferences.
There are several types of treatment for prostate cancer, as listed below:
1. Active Surveillance
This method involves closely monitoring prostate cancer without immediate treatment. It is often recommended for low-risk prostate cancer that does not show any symptoms and appears to grow slowly.
While this method can help avoid or delay the side effects of treatments, it does carry the risk of the cancer progressing, potentially making it more difficult to treat later on.
2. Surgery
Surgery is another effective treatment option for prostate cancer, especially in localised cases and early stages.
The surgery can be divided into 2 main types
a) Radical Prostatectomy: Removal of the entire prostate gland and some surrounding tissue and lymph nodes.
b) Retropubic Surgery: Removal of the entire prostate gland through an incision in the wall of the abdomen.
3. Radiation Therapy
This method involves using high-powered energy to kill the prostate cancer cells. It is often used for localised cancer or as an adjuvant treatment after surgery.
There are 2 types of radiation therapy, namely:
a) External Beam Radiation Therapy (EBRT): High-energy rays are directed at the prostate to kill cancer cells.
b) Brachytherapy: Radioactive seeds are implanted directly into or near the prostate to deliver localised radiation.
4. Hormone Therapy
Hormone therapy aims to reduce levels of male hormones (androgens), particularly testosterone, which can fuel prostate cancer growth.
It works well in slowing down tumour growth in advanced stages and shrinking tumours before radiation therapy in the early stages.
This therapy can be performed in 2 ways:
a) Medications: Use medicines that stop testosterone production in the testicles or prevent testosterone from reaching cancer cells.
b) Surgical option: Removal of testicles to eliminate the main source of testosterone.
5. Chemotherapy
This therapy uses drugs to kill rapidly dividing cancer cells, typically used for advanced or metastatic prostate cancer.
6. Immunotherapy
This treatment helps your immune system to recognise and fight off cancer cells. It works well in treating advanced prostate cancer, too.
7. Targeted Therapy
This therapy, often used for advanced prostate cancer, involves medications that target genetic mutations or specific pathways that drive the prostate cancer’s growth.
Want to learn more about the treatments for other cancers? Check out these informative articles:
Side Effects of Prostate Cancer Treatments
Prostate cancer treatments can lead to a variety of side effects, which may vary based on the type of treatment chosen.
Here are the common side effects associated with various treatment options:
- Erectile dysfunction
- Urinary incontinence
- Changes in orgasm (e.g., dry orgasm)
- Infertility
- Fatigue
- Hot flushes
- Weight gain
- Reduced libido
- Painful and frequent urination
- Bowel problems
- Nausea and vomiting
- Loss of appetite
- Osteoporosis
Should you have any concerns regarding your treatment journey, do not hesitate to consult our doctors to learn more about the risks involved.
Living with Prostate Cancer
Receiving a prostate cancer diagnosis can be life-changing. In this section, we will explore the key aspects of navigating life with prostate cancer:
- Managing Side Effects
Many prostate cancer treatments can cause side effects like urinary incontinence, erectile dysfunction, and bowel problems.Hence, it’s important to discuss any side effects with your doctor and explore ways to manage them, such as pelvic floor exercises, medications, or devices. - Emotional Support
Dealing with a prostate cancer diagnosis and treatment can be emotionally challenging.Seeking support from family, friends, support groups, or mental health professionals can help you cope with the stress and anxiety due to the diagnosis. - Fertility Preservation
If you plan to have children in the future, discuss fertility preservation options with your doctor before starting treatment, as some treatments can affect fertility.
Measures to Prevent Prostate Cancer
While there is no guaranteed way to prevent prostate cancer, certain measures can potentially reduce the risk, including:
1. Practise A Healthy Diet
To lower the risk of prostate cancer, your diet should be rich in vegetables, whole grains, legumes, and fruits while low in fats and sugars.
Among various dietary patterns, research shows that the Mediterranean diet has been linked to a reduced risk of prostate cancer.
This diet emphasises plant-based foods like fruits, vegetables, legumes, and nuts, along with lean proteins such as poultry and fish, as well as healthy fats from olive oil and avocados.
However, for those who prefer a local approach, the Malaysian Healthy Plate (MHP) offers similar benefits. Like the Mediterranean diet, MHP also promotes the consumption of vegetables, fruits, and healthy carbohydrates and proteins.
2. Exercise Regularly
Engaging in regular physical activity has been linked to a lower risk of developing prostate cancer.
Aim for at least 30 minutes of moderate exercise most days of the week, as studies suggest that vigorous activity can significantly reduce the risk.
If you are new to exercising, start off slow and gradually lengthen your exercise time.
3. Maintain a Healthy Weight
Obesity is associated with an increased risk of advanced prostate cancer. Therefore, maintaining a healthy weight through diet and exercise can help mitigate this risk.
If you are struggling with excess weight or obesity despite lifestyle changes, check out our articles on Body Composition Analysis (BCA) and bariatric surgery for more information!
4. Limit Alcohol Consumption
Reducing alcohol intake can help reduce the risk of prostate cancer.
High alcohol intake, especially binge drinking, is linked to a higher chance of prostate cancer and can speed up tumour growth. For those diagnosed with prostate cancer, quitting alcohol is also strongly recommended to slow disease progression.
5. Quit Smoking
Smoking can increase testosterone levels and decrease oestrogen levels in your body. This hormonal imbalance may create an environment that favours prostate cancer development.
Aside from that, cigarettes contain harmful substances like cadmium. These chemicals can interact with hormones in your body, potentially triggering prostate cancer growth.
Hence, quitting smoking is a significant step towards reducing your risk of prostate cancer and improving your overall health.
6. Attend Regular Check-ups
Since prostate cancer often grows slowly, early detection in stages 1 and 2 usually leads to excellent treatment outcomes. This highlights the importance of regular health check-ups, particularly for men with higher risk factors.
Hence, don’t wait for symptoms to appear – take proactive steps to safeguard your health today!
At Island Hospital, we offer comprehensive health screening packages designed specifically for men’s health needs.
Our Comprehensive Plus Package for Males includes:
- A cancer marker test featuring the PSA (Prostate-Specific Antigen) test
- PSA is a crucial indicator of prostate cancer risk.
- An ultrasound of the abdomen and prostate
- This will provide a detailed view of your prostate to detect any potential abnormalities early.
Recognising that health needs vary among individuals, we provide a range of health screening packages to fit different requirements and budgets, too.
Schedule your health screening at Island Hospital today – your future self will thank you for taking this important step towards a healthier life!
Read More:
Island Hospital: Your Trusted Partner for Prostate Cancer Solutions
At Island Hospital, our specialists from the Urology Centre and the Clinical Oncology and Haemato-Oncology Centre are always here to guide you throughout your prostate cancer journey.
Our multidisciplinary approach combines precise diagnostic testing, advanced treatments, and compassionate support services to ensure you receive the highest level of care.
This commitment to excellence has earned us recognition on the global stage. We’re proud to be a finalist in Malaysia’s Flagship Medical Tourism Hospital Programme and to have secured a place on Newsweek’s list of World’s Best Hospitals 2024.
Don’t let prostate cancer control your life any longer – contact us today to learn about our world-class treatment options and our philosophy of providing comforting, patient-centric care.
Book an appointment today and start your journey to recovery.
FAQ
What are the early warning signs of prostate cancer?
The early warning signs of prostate cancer include:
- Burning sensation or pain during urination
- Difficulty starting or stopping urination
- Frequent urination, especially at night
- Decreased flow of urine
- Blood in urine or semen
- Loss of bladder control
- Erectile dysfunction
- Painful ejaculation
Consult a doctor for proper evaluation if you notice any of these symptoms. Learn more about the symptoms of early prostate cancer in this section.
What are the signs that prostate cancer is getting worse?
Signs of advancing prostate cancer may include:
- Unexplained weight loss
- Fatigue or general weakness
- Loss of appetite
- Persistent bone pain, particularly in the spine, hips, or ribs
- Fractures from weakened bones
- Swelling of legs or pelvic area
- Numbness or pain in the hands, feet, or legs
- Loss of bowel control
If you experience any of these symptoms, please visit a hospital promptly to seek treatment before the condition worsens. Learn more about the symptoms of advanced prostate cancer in this section.
Can prostate cancer be 100% cured?
While early-stage prostate cancer can often be successfully treated, it’s difficult to guarantee a 100% cure.
The 5-year relative survival rate for localised or regional prostate cancer is nearly 100%, meaning many men can live long, healthy lives after treatment.
However, there’s always a small chance the cancer may return, so ongoing monitoring is recommended.
If prostate cancer spreads to other body parts, the 5-year relative survival rate can drop to 31%. Hence, early intervention is vital to improve the chances of successful treatment.
How fast can prostate cancer spread?
Prostate cancer often grows slowly, but the rate can vary significantly between individuals. Some forms are slow-growing and may take years to spread beyond the prostate, while more aggressive types can spread more rapidly.
On average, it may take 2-4 years for localised prostate cancer to double in size. However, once it metastasizes, it can spread more quickly to other parts of the body.
Can you live without a prostate?
Yes, men can live without a prostate.
The prostate is sometimes removed (radical prostatectomy) as a treatment for prostate cancer. While this can cause side effects like urinary incontinence and erectile dysfunction, these often improve over time with proper management.
After all, the prostate’s main function is related to reproduction, so its removal doesn’t prevent a man from living a full life.
If you’re concerned about erectile dysfunction after prostate removal, read this article on the available treatments.
Related Doctors
| Derived from | Complications |
|---|






