
27 Jan What to Expect During Chemotherapy: Preparation, Side Effects, and Recovery
What to Expect During Chemotherapy: Preparation, Side Effects, and Recovery
By Island Hospital | Jan 27, 2026 12:00:00 PM
Starting chemotherapy often comes with many unknowns. While a cancer diagnosis itself is life-changing, beginning chemotherapy can leave patients with a new set of unanswered questions, concerns, and emotions about how their body will cope and whether life will feel normal again during treatment.
Chemotherapy is a powerful and commonly used cancer treatment, but the experience differs for everyone. While some people manage treatment with minimal disruption to daily life, others may need more time to adjust physically, emotionally, and mentally.
Understanding what to expect before, during, and after chemotherapy can make a meaningful difference throughout your cancer journey.
This guide is designed to support patients and caregivers by offering practical information on treatment preparation, common side effects, and ways to manage daily life during chemotherapy—so you can approach treatment feeling informed, supported, and more in control of your journey.
What Is Chemotherapy?
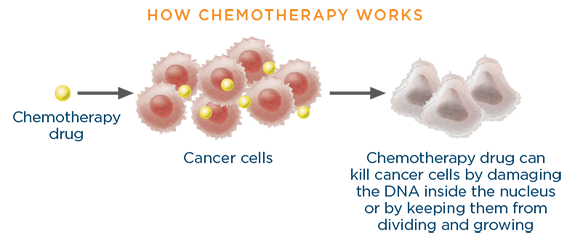
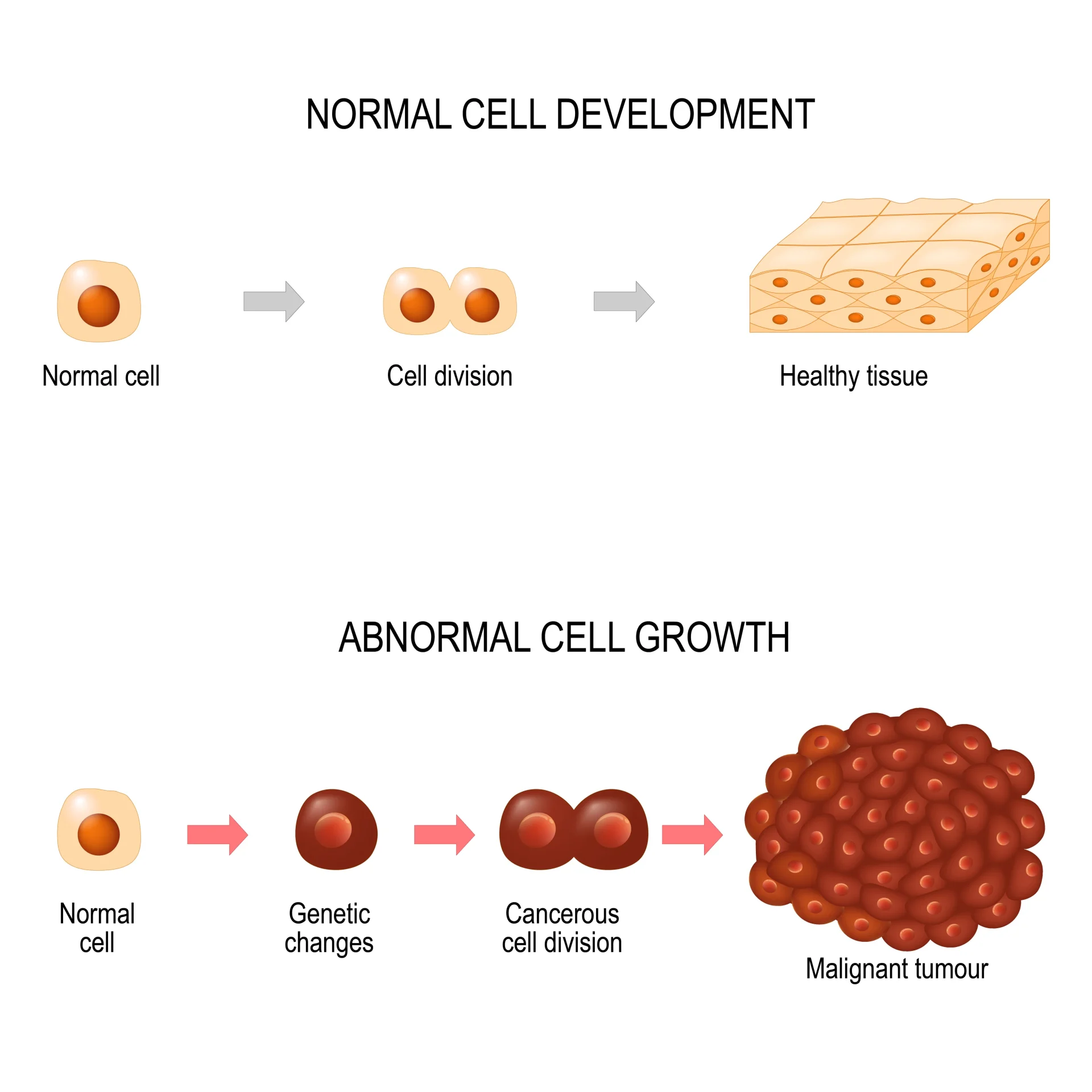
Chemotherapy is a type of cancer treatment that uses medicines to destroy cancer cells or slow their growth. Cancer cells tend to grow and divide more quickly than most normal cells in the body, and chemotherapy works by targeting these fast-dividing cells to stop them from multiplying and spreading.
Because chemotherapy travels through the bloodstream, it can reach cancer cells throughout the body. This makes it an effective treatment not only for shrinking tumours, but also for treating cancer that may have spread or for reducing the risk of cancer returning after surgery or radiation therapy.
Types of Chemotherapy
Chemotherapy can be given in different ways, depending on the type of cancer, the drugs used, and the patient’s overall treatment plan. Your oncologist will recommend the most effective and suitable method for your condition.
1. Intravenous (IV) Chemotherapy
IV chemotherapy is delivered directly into a vein, usually through a drip, port, or catheter, and is commonly used for treatments given over a longer period.
2. Oral Chemotherapy
Oral chemotherapy is taken by mouth as tablets or capsules and must be taken exactly as prescribed, even though treatment is given at home.
3. Chemotherapy Injections
In some cases, chemotherapy may be given as an injection under the skin or into a muscle, depending on the medication and treatment plan.
Looking to understand skin cancer better? This detailed article on skin cancer has all the information you need!
Before Chemotherapy: How to Prepare
The days leading up to chemotherapy can bring a mix of emotions, from anxiety to uncertainty. Preparing for treatment is not only about medical tests and appointments, but also about taking practical steps to feel physically and emotionally ready.
1. Medical Assessments and Planning
Before starting chemotherapy, your oncologist will carry out several assessments to ensure the treatment is safe and appropriate for you. These may include:
- Blood tests to check blood counts and overall health
- Imaging tests (such as scans) to understand the extent of the cancer
- Organ function tests, including heart, kidney, or liver assessments, depending on the chemotherapy drugs planned
- Review of current medications, supplements, and allergies
- Assessment of overall fitness and medical history to personalise your treatment plan
These assessments help your care team determine the most suitable chemotherapy type, dosage, and schedule. You will also discuss how often treatment is given, how long each session may take, and potential side effects to watch for.
2. Understanding Your Treatment Schedule
Chemotherapy is usually given in cycles, with treatment days followed by rest periods to allow your body time to recover. Knowing your schedule in advance can help you plan work, family responsibilities, transport, and rest time.
3. Preparing Emotionally and Mentally
Feeling anxious before chemotherapy is common. Talking openly with your healthcare team or loved ones can help you feel more supported. Writing down questions before appointments may also make discussions easier.
4. Practical Preparation at Home
At home, small preparations, such as arranging help with daily tasks, preparing simple meals, and planning transport to and from treatment can make recovery days more manageable. Keeping a notebook or digital record to track appointments, medications, and side effects can also be helpful as treatment progresses.
What to Bring to Your Chemotherapy Appointment
Being prepared can go a long way on chemotherapy days. Knowing what to bring with you can help you focus on your treatment and make the experience more manageable and less stressful.
| Category | Checklist Items |
|---|---|
| Documents and Information | Identification (IC or passport) Appointment details or referral letters List of current medications, supplements, and allergies |
| Comfort and Clothing | Comfortable clothing (layers recommended) Light jacket, shawl, or blanket |
| Personal Items | Mobile phone, tablet, or laptop Headphones or earphones Charger or power bank Reading material |
| Food and Drinks | Light snacks you tolerate well Water bottle or preferred drinks |
| Support | Notebook or notes app for questions Family member or friend for emotional support and transport |
What to Expect on Your First Day of Chemotherapy
The first day of chemotherapy is often the most unfamiliar part of treatment. Knowing what typically happens can help reduce uncertainty and make the day feel more manageable.
1. Arrival and Check-In
When you arrive at the treatment centre, you will check in and be guided to the chemotherapy unit. A nurse will check your vital signs, such as blood pressure, temperature, and weight. In some cases, a blood test may be done on the same day to ensure it is safe to proceed with treatment.
2. Before Treatment Begins
Once you are settled, chemotherapy will be prepared. This may involve inserting an intravenous (IV) line or connecting treatment through a port or catheter if you have one. You will also receive medications beforehand to help prevent side effects such as nausea or allergic reactions.
3. During Treatment
Chemotherapy is given over a set period of time, which may range from less than an hour to several hours, depending on your treatment plan. During this time, you will be monitored closely by the nursing team.
If you feel unwell at any point, it’s important to inform your nurse immediately.
4. After the Session
After treatment is completed, your IV line will be removed or disconnected. Your nurse will review after-care instructions, including medications to take at home, possible side effects, and when to contact your care team.
Many people use this time to rest, read, or listen to music. If you feel unwell at any point, it’s important to inform your nurse immediately.
5. Later That Day and the Days After
Some people feel relatively normal after their first treatment, while others may notice fatigue or mild discomfort later that day or over the next few days. These effects can vary from one treatment cycle to the next.
Your healthcare team is there to support you, so contact them if any symptoms feel severe or concerning.
Why Chemotherapy Can Cause Side Effects
Chemotherapy is designed to target cancer cells, but it can also affect some healthy cells that divide quickly, such as those in the hair follicles, digestive system, bone marrow, and mouth. This is why side effects may occur during treatment.
Side effects vary widely from person to person. Some people experience only mild changes, while others may need additional support. Your healthcare team will monitor you closely and help manage symptoms as they arise.
1. Fatigue

Fatigue is one of the most common side effects of chemotherapy. It may feel different from usual tiredness and can fluctuate throughout treatment cycles, making rest and pacing important.
2. Nausea and Vomiting
Some chemotherapy drugs can cause nausea or vomiting, particularly in the days following treatment. Medications are often given to help reduce these effects, and adjustments can be made if symptoms persist.
3. Hair and Appearance Changes

Some chemotherapy drugs cause hair thinning or hair loss, while others may not. Hair loss can also affect eyebrows, eyelashes, and body hair. These changes are usually temporary, and hair often begins to grow back after treatment ends.
4. Changes to Skin and Nails
You may notice dry skin, sensitivity, or changes to your nails, such as brittleness or discolouration. Inform your care team if you notice pain, swelling, or signs of infection.
5. Mouth and Taste Changes
Chemotherapy can affect the mouth and taste buds, leading to dry mouth, mouth sores, or changes in how food tastes. Some people find that certain foods taste metallic or bland during treatment.
6. Digestive Changes
Changes in appetite, constipation, or diarrhoea may occur during chemotherapy. Your healthcare team can provide advice or medications if these symptoms become uncomfortable.
7. Numbness or Tingling (Neuropathy)
Some chemotherapy drugs may cause numbness, tingling, or weakness in the hands and feet. It’s important to report these symptoms early, as adjustments to treatment may help prevent worsening effects.
8. Lowered Immunity
Chemotherapy can reduce the number of white blood cells, making it easier to get infections. Your care team will monitor your blood counts closely. Contact your healthcare provider if you develop a fever or signs of infection.
Curious about the most common types of cancer and their symptoms? This article breaks down the key signs you should know in clear, patient-friendly terms!
Emotional, Mental, and Cognitive Effects
Chemotherapy can affect more than just the body. Many patients notice emotional and mental changes during treatment, which are a normal part of the experience and can vary from person to person.
1. Mood Changes and Emotional Fatigue
It is common to experience changes in mood during chemotherapy. Feelings of anxiety, low mood, irritability, or emotional exhaustion may occur, especially as treatment progresses. These emotions can be influenced by physical side effects, treatment stress, and changes to daily routines.
2. “Chemo Brain” (Cognitive Changes)
Some people notice changes in concentration, memory, or mental clarity during chemotherapy, often referred to as “chemo brain.” This may include forgetfulness, slower thinking, or difficulty focusing. These symptoms can come and go and often improve after treatment ends.
3. When to Seek Support
If emotional distress, anxiety, low mood, or cognitive changes begin to interfere with daily life, sleep, or relationships, it’s important to seek support. Your healthcare team can help connect you with counselling, psychological support services, or other resources as needed.
Nutrition and Self-Care During Chemotherapy
Good nutrition and self-care play an important role in supporting your body during chemotherapy. While appetite and energy levels may change throughout treatment, small, thoughtful choices can help you feel more comfortable and maintain your strength.
1. Staying Hydrated
Drinking enough fluids before and after chemotherapy helps your body process medications and may reduce side effects such as fatigue, nausea, and constipation. Water, clear soups, and non-caffeinated drinks are good options. If plain water is difficult to tolerate, flavoured drinks or ice chips may help.
2. Eating Well During Treatment
Eating smaller, more frequent meals is often easier than large meals during chemotherapy. Light, bland foods such as crackers, toast, rice, bananas, or soups are commonly better tolerated when nausea is present. Including protein-rich foods when possible can help support energy and recovery.
3. Managing Taste Changes
Changes in taste are common and may cause food to taste bland, metallic, or unpleasant. Trying different flavours, textures, or temperatures may help. Some people find that mild spices, herbs, or citrus flavours improve taste, while others prefer softer or cooler foods.
4. Support from a Dietitian
An oncology-trained dietitian can provide personalised advice based on your treatment, side effects, and nutritional needs. They can help manage appetite changes, maintain weight, and ensure you’re getting adequate nutrients during chemotherapy.
Living Day-to-Day During Chemotherapy
Chemotherapy can affect daily life in different ways, but with flexibility and small adjustments, many patients are able to continue parts of their usual routine. Finding a balance between activity and rest can help you manage treatment while maintaining a sense of normalcy.
1. Managing Work, Family, and Daily Routines
How much you are able to do during chemotherapy depends on how your body responds to treatment. Some people continue working or caring for family as usual, while others may need to reduce responsibilities or ask for additional support.
Open communication with employers, family members, and caregivers can help set realistic expectations and reduce stress.
2. Physical Activity and Movement
Light to moderate physical activity, such as walking or gentle stretching, may help support energy levels, mood, and sleep during chemotherapy. It’s important to listen to your body and rest when needed, especially on days when fatigue is more noticeable. Always follow guidance from your healthcare team.
3. Sleep, Rest, and Energy Conservation
Fatigue is common during chemotherapy and may change over time. Taking short rest breaks during the day, maintaining regular sleep routines, and planning activities when you feel most alert can help conserve energy.
4. Maintaining a Sense of Normalcy
Many patients find comfort in keeping familiar routines, hobbies, or social connections during treatment. While adjustments may be necessary, continuing activities that bring comfort or enjoyment can support emotional well-being throughout chemotherapy.
After Chemotherapy: Recovery and Home Care
Chemotherapy is only one part of the process—recovery afterward is equally important. What you experience after treatment can vary from cycle to cycle, making post-treatment care an essential part of your overall journey.
1. The First Few Days After Treatment
The first few days after chemotherapy are often when side effects are most noticeable. Some symptoms improve within a few days, while others may fluctuate throughout the cycle. Keeping track of how you feel can help you understand your body’s pattern and communicate effectively with your care team.
| Common and Usually Normal | Needs Medical Attention |
|---|---|
| Mild to moderate fatigue | Fever or chills |
| Temporary nausea or reduced appetite | Severe or ongoing nausea or vomiting |
| General body aches or discomfort | Uncontrolled or worsening pain |
| Mild weakness or low energy | Shortness of breath or chest pain |
| Changes in appetite or taste | Dizziness, fainting, or confusion |
| Mild digestive changes (constipation or diarrhoea) | Signs of infection (redness, swelling, sore throat, persistent cough) |
| Occasional headaches | Any symptom that feels severe, unusual, or different from previous cycles |
2. Recovery After Treatment Ends
After chemotherapy is completed, recovery continues gradually. Fatigue may persist for weeks or months, and hair regrowth often begins after treatment ends, sometimes with changes in texture or colour.
Most people are able to slowly return to usual activities, including work and exercise, as strength and stamina improve. Recovery is not linear, and allowing yourself time to heal is an important part of the process.
Supporting You Through Every Step of Chemotherapy!
Facing chemotherapy can feel overwhelming, but having the right medical team makes all the difference. Whether you’re preparing for treatment, currently undergoing chemotherapy, or supporting a loved one, expert guidance and compassionate care are essential at every step.
At Island Hospital, our multidisciplinary Oncology team provides personalised chemotherapy care with patient safety, comfort, and outcomes in mind. From diagnosis and treatment planning to recovery and follow-up, we are here to support your journey.
Take the next step with confidence — speak to our Cancer Care Specialists and schedule your appointment today!
Take Control of Your Health with Early Cancer Detection
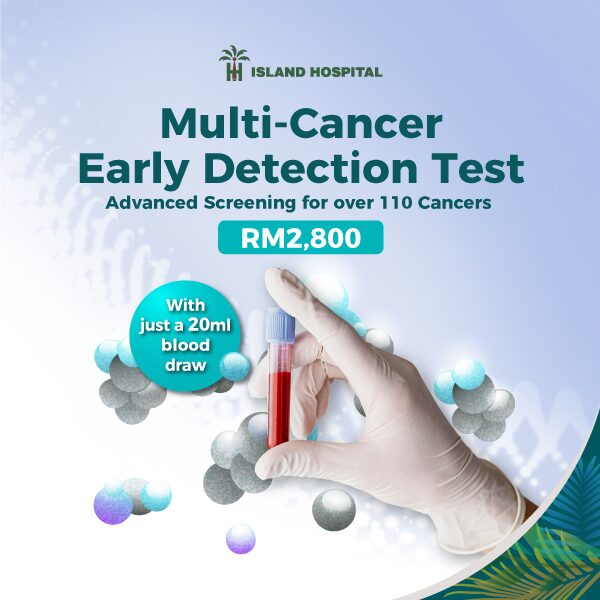
Many cancers develop silently, showing few or no symptoms in the early stages. Early detection plays a crucial role in improving treatment outcomes, reducing the complexity of care, and providing greater peace of mind.
At Island Hospital, the Multi-Cancer Early Detection (MCED) Test offers a proactive approach to cancer screening through a simple blood test. It can detect signals from more than 20 types of cancer, including some not typically found through routine screening.
For RM2,800, you’ll receive:
- A single blood sample collected by a healthcare professional
- Advanced laboratory analysis to detect cancer-related DNA signals
- Review of results by your healthcare provider, with guidance on next steps if needed
Taking a proactive approach to cancer screening empowers you with early insights, allowing for timely intervention and informed health decisions.
FAQ
1. Will chemotherapy be painful?
Chemotherapy itself is usually not painful. Most people feel little to no discomfort during the infusion, though inserting an IV line may cause brief discomfort. Some side effects, such as body aches or soreness, may occur after treatment and can usually be managed with medication and rest.
2. How long does chemotherapy usually last?
The length of chemotherapy varies depending on the type of cancer, treatment goals, and individual response. Some people receive chemotherapy for a few weeks, while others may continue for several months. Your oncologist will explain your treatment schedule and expected duration.
3. Does early cancer detection still matter if someone needs chemotherapy?
Yes. Early detection can influence treatment options, outcomes, and recovery. Screening tools such as the Multi-Cancer Early Detection (MCED) Test may help identify cancers earlier, particularly those not detected through routine screening.
4. Can chemotherapy affect fertility or future family planning?
Yes, some chemotherapy treatments can affect fertility. The impact depends on factors such as the type of chemotherapy drugs used, dosage, treatment duration, and age. For some people, these effects are temporary, while for others they may be long-term.
If fertility or future family planning is important to you, it’s best to discuss this with your oncologist before starting chemotherapy. Fertility preservation options, such as freezing eggs, sperm, or embryos, may be available.
5. Can cancer return after treatment?
Yes, in some cases cancer can return after treatment. This is known as a recurrence. The risk of recurrence depends on factors such as the type of cancer, its stage at diagnosis, how it responded to treatment, and individual health factors. Many people complete treatment and never experience a recurrence.
Regular follow-up appointments, screenings, and monitoring are an important part of cancer care after treatment. These help detect any changes early and provide reassurance.






