12 Jan What Are the Best Birth Control Methods for Women: A Complete Guide to Contraception
What Are the Best Birth Control Methods for Women: A Complete Guide to Contraception
By Island Hospital | Jan 12, 2026 12:00:00 PM
Choosing the right birth control is not always straightforward — and for many women, it can feel overwhelming. With so many conversations warning about potential side effects, it’s understandable that many women feel anxious or unsure about where to begin.
Even with more than 15 modern contraceptive options available in Malaysia, awareness and access remain limited. Studies show that one in three pregnancies in Malaysia is unplanned, while only 34.5% of women use modern contraception.
This suggests that many women may not be receiving the guidance, clarity, or reassurance they need to make informed choices about their reproductive health.
This article is here to change that. We’ll walk you through the best birth control methods for women, how each one works, and how to choose a method that fits your lifestyle and comfort level, helping you understand your options with clarity and confidence.
What is Birth Control?

Birth control, also known as contraception, refers to any method used to prevent pregnancy. While most people associate it with “the pill,” birth control actually comes in many forms, including hormonal methods, non-hormonal options, physical barriers, long-acting devices, and even natural tracking techniques.
Different methods work in different ways, such as by:
- Stopping ovulation (preventing the release of an egg)
- Thickening cervical mucus so sperm can’t reach the egg
- Preventing fertilisation
- Preventing implantation
- Acting as a physical barrier between the sperm and the egg
- Tracking fertile windows to avoid intercourse during peak fertility
Why Choosing the Right Birth Control Method Matters
Choosing a birth control method isn’t just about preventing pregnancy — it’s about protecting your overall well-being. Every woman’s body responds differently to hormones, devices, and lifestyle factors, which is why choosing the right method can make a significant difference to both your comfort and confidence.
Here’s why making the right choice matters:
-
Hormonal sensitivity varies from woman to woman
Some women feel absolutely fine on hormonal contraception, while others may experience mood changes, headaches, or irregular bleeding. Understanding your body’s hormonal responses can help you avoid unnecessary discomfort and choose a method that supports your well-being.
-
It can improve your period or make it worse
Certain methods can make periods lighter, shorter, or even stop them completely. Others may cause heavier or more irregular bleeding. Selecting the right method can help manage:
- heavy periods
- painful cramps
- PMS symptoms
- period-related migraines
-
It affects your fertility timeline
If you plan to conceive soon, you may prefer a method with a quick return to fertility. If you’re planning to delay pregnancy for years, long-acting methods might be more suitable. Understanding this timing helps prevent both unplanned pregnancy and unnecessary delays.
-
Your medical history matters
Some contraceptives are not recommended if you have certain conditions, such as:
- migraine with aura
- high blood pressure
- clotting disorders
- breastfeeding
- PCOS
- depression/anxiety
Choosing the wrong method may worsen symptoms, but the right one can actually improve them.
-
Different lifestyles need different levels of commitment
If you’re someone who forgets daily pills, a long-acting method may offer better protection. If you want something, you can stop anytime; a daily or monthly method may be ideal.
-
Safety, side effects & long-term health
Every method has risks and benefits. Choosing well can reduce unwanted side effects and help you avoid methods that don’t match your physical or emotional needs.
Want to stay ahead of your reproductive health? Learn the 14 early signs of pregnancy to help you understand your body better.
Birth Control Options for Women in Malaysia
Understanding the available birth control options is the first step in choosing a method that feels right for your body and lifestyle. Birth control methods generally fall into two categories — hormonal and non-hormonal. Here’s a clear, detailed breakdown to help you compare your choices with confidence.
Hormonal Birth Control
Hormonal contraception works by using synthetic hormones, either a combination of oestrogen and progestin, or progestin only, to prevent pregnancy. These hormones stop ovulation, thicken cervical mucus, and thin the uterine lining to reduce the chances of fertilisation.
In Malaysia, hormonal methods are widely used and readily available across both private and government healthcare facilities.
1. Birth Control Pills (Combined Pill & Progestin-Only Pill)

Birth control pills come in two forms:
-
Combined oral contraceptives (COCs)
Contain both oestrogen and progestin, and prevent pregnancy by blocking ovulation, thickening cervical mucus, and thinning the uterine lining.
-
Progestin-only pills (the mini pill)
Mainly work by thickening cervical mucus and are a suitable option for women who are breastfeeding or need to avoid oestrogen.
When taken correctly, the pill is up to 99% effective, though typical daily use places effectiveness at around 91%. This method is best for women who want predictable cycles, lighter periods, or a contraceptive that is affordable, easily reversible, and gives them a sense of day-to-day control.
| Pros | Cons / Possible Side Effects |
|---|---|
| Regulates menstrual cycles | Must be taken daily at the same time |
| Reduces cramps and heavy bleeding | Nausea, breast tenderness, mild headaches |
| Helps improve acne (especially pills with drospirenone like Yaz) | Breakthrough spotting in the first few months |
| Can help with PCOS-related symptoms | Not suitable for women with migraine with aura |
| Quick return to fertility after stopping | Not suitable for those with a history of blood clots |
| Not recommended for smokers over age 35 |
|
| Not suitable for women with uncontrolled hypertension |
2. Hormonal IUD
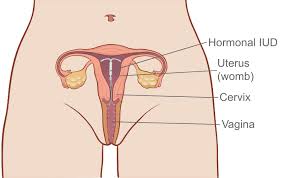
A hormonal IUD is a small T-shaped device placed inside the uterus, where it releases a low dose of progestin that thickens cervical mucus, thins the uterine lining, and may suppress ovulation in some women.
It is over 99% effective and offers long-term protection for 3 to 5 years, depending on the brand. This method is ideal for women who want long-lasting, low-maintenance contraception and those who prefer lighter or more manageable periods.
| Pros | Cons / Possible Side Effects |
|---|---|
| Over 99% effective | Irregular spotting for the first 3–6 months |
| Long-lasting (3–5 years) | Cramping or discomfort during/after insertion |
| Significantly reduces menstrual bleeding | Requires a doctor for insertion/removal |
| Some women stop having periods entirely | Does not protect against STIs |
| Low hormone exposure (acts mostly locally) | Rare risk of expulsion (IUD may shift or come out) |
| Immediate return to fertility once removed | Not suitable for women with certain uterine conditions |
3. Vaginal Ring
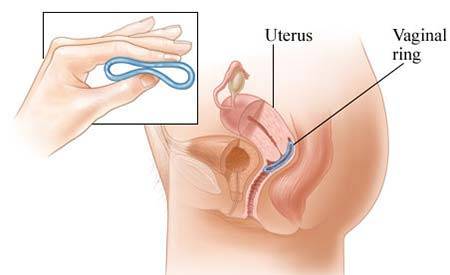
The vaginal ring is a small, flexible device inserted into the vagina, where it releases oestrogen and progestin to prevent ovulation while also thickening cervical mucus. When used correctly, it is 91% effective with typical use and up to 99% effective with perfect use.
This method is best for women who want a low-maintenance, once-a-month hormonal option without needing to take a daily pill.
| Pros | Cons / Possible Side Effects |
|---|---|
| Over 99% effective | Irregular spotting for the first 3–6 months |
| Long-lasting (3–5 years) | Cramping or discomfort during/after insertion |
| Significantly reduces menstrual bleeding | Requires a doctor for insertion/removal |
| Some women stop having periods entirely | Does not protect against STIs |
| Low hormone exposure (acts mostly locally) | Rare risk of expulsion (IUD may shift or come out) |
| Immediate return to fertility once removed | Not suitable for women with certain uterine conditions |
4. Contraceptive Implant (Nexplanon/Implanon)
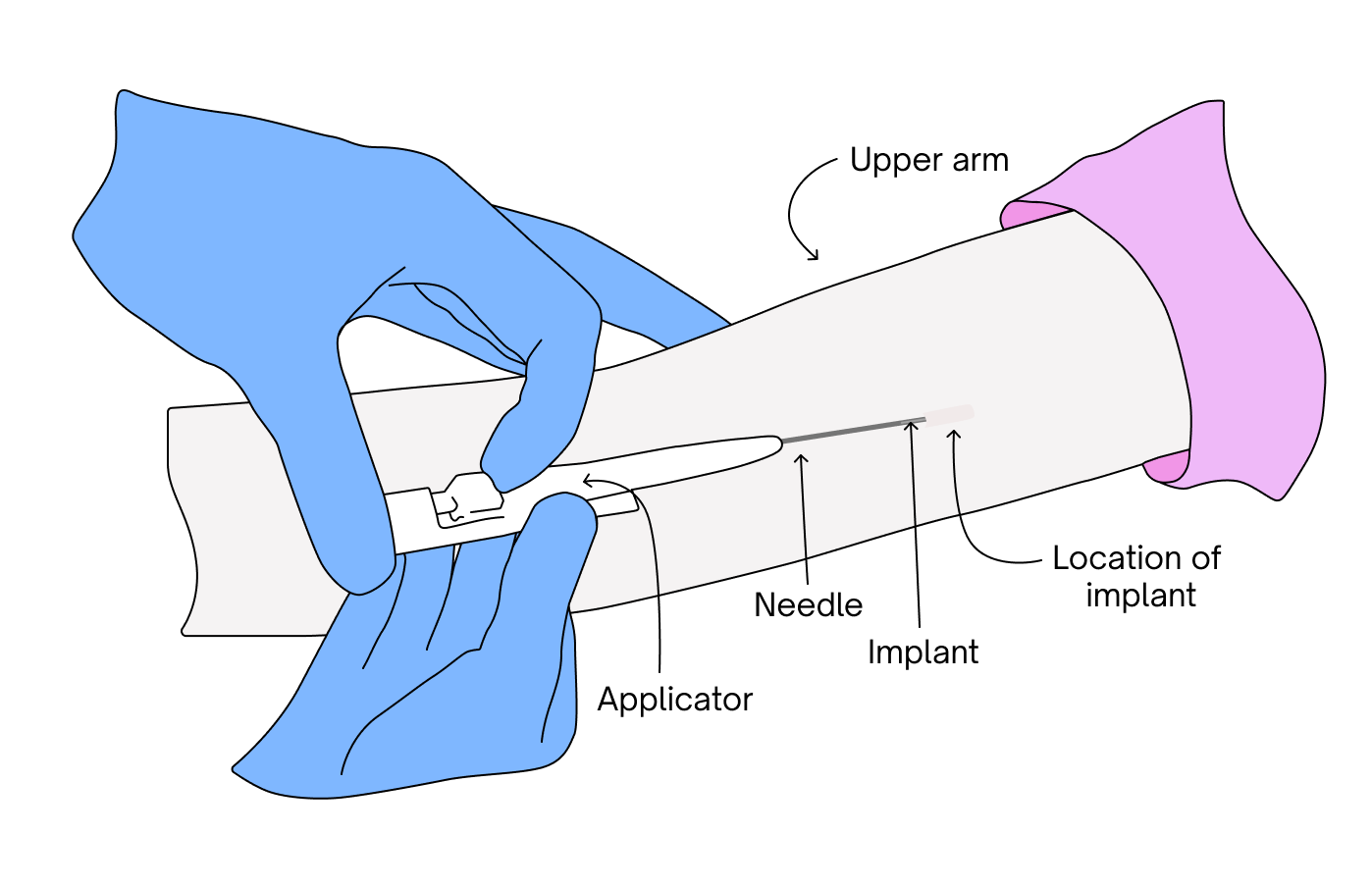
The contraceptive implant is a small rod inserted under the skin of the upper arm that releases progestin to prevent ovulation and thicken cervical mucus. It is over 99% effective and provides long-term protection for up to 3 years.
This method is ideal for women seeking a highly effective, low-maintenance option that does not involve oestrogen.
| Pros | Cons / Possible Side Effects |
|---|---|
| Extremely effective (over 99%) | Irregular bleeding is common |
| Long-lasting (up to 3 years) | Possible weight or mood changes |
| Safe for breastfeeding | Requires a minor procedure to insert/remove |
| No oestrogen | Temporary bruising or soreness at the insertion site |
| Quick return to fertility after removal | Does not protect against STIs |
5. Contraceptive Injection (Depo-Provera)

The contraceptive injection contains progestin and is given once every 12 weeks, preventing ovulation and thickening cervical mucus. It is 94% effective with typical use and up to 99% effective with perfect timing.
This method suits women who prefer a hormone-only option without oestrogen and want contraception that requires attention only a few times a year.
| Pros | Cons / Possible Side Effects |
|---|---|
| Only needed every 12 weeks | Irregular or prolonged bleeding |
| No oestrogen | Possible weight gain |
| Reduces menstrual cramps | Mood changes in some women |
| May stop periods over time | Delayed return to fertility (6–12 months) |
| Very effective | Cannot be reversed once the shot is given |
| Suitable for breastfeeding | Does not protect against STIs |
Non-Hormonal Birth Control
Non-hormonal birth control methods do not use synthetic hormones to prevent pregnancy. Instead, they work through physical barriers, natural cycle tracking, or the use of copper to stop fertilisation.
These options are ideal for women who prefer to avoid hormones, have medical conditions that limit hormonal use, or want a more natural approach to contraception.
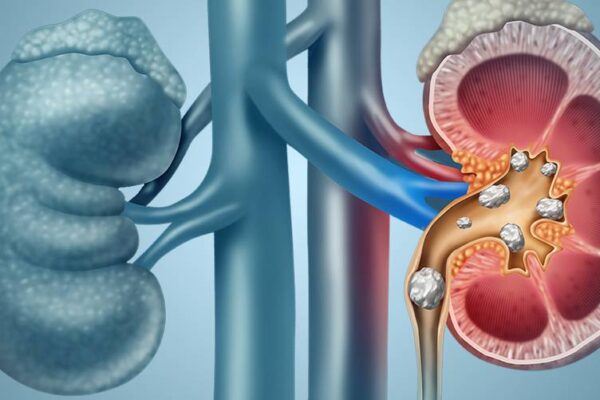
6. Copper IUD
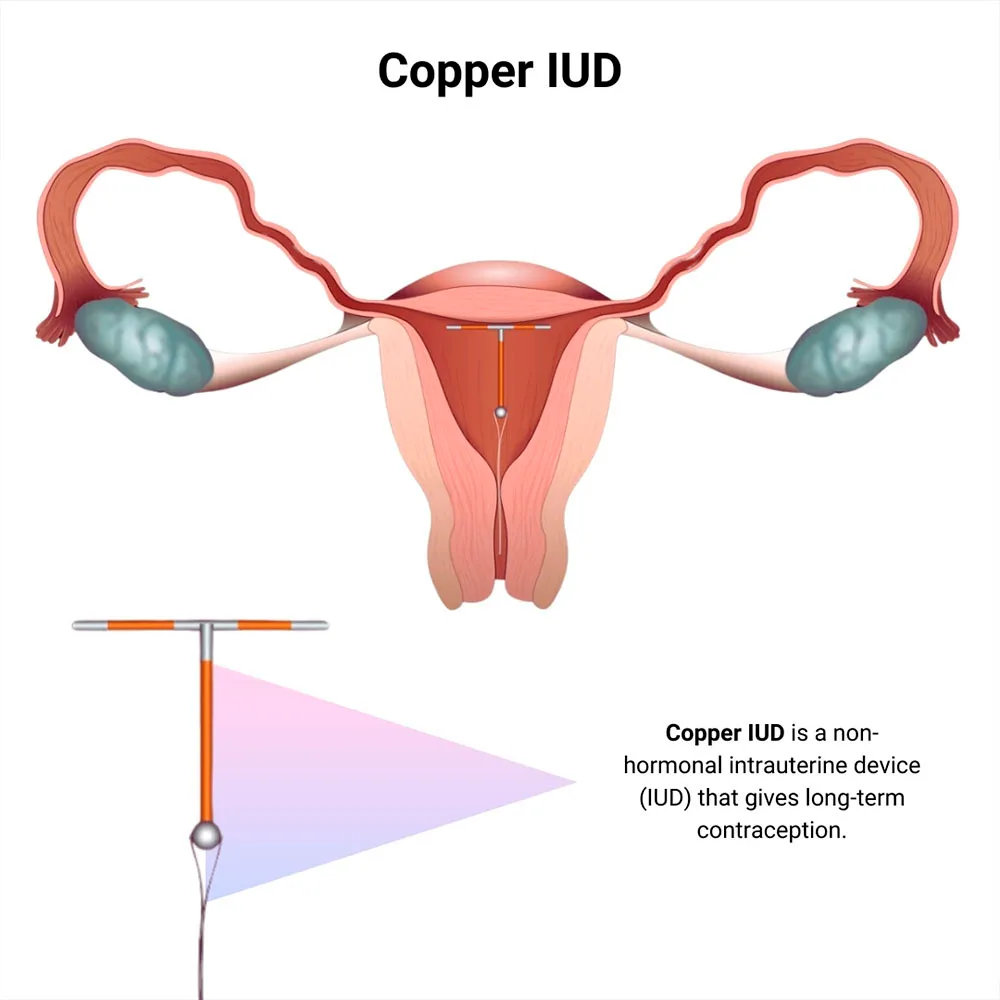
The copper IUD is a hormone-free device placed in the uterus, where copper ions create an environment toxic to sperm, preventing fertilisation. It is over 99% effective and lasts 5–10 years.
This method is best for women who want long-term contraception without hormones and prefer a highly reliable, maintenance-free option.
| Pros | Cons / Possible Side Effects |
|---|---|
| Long-lasting (5–10 years) | Heavier or more painful periods at first |
| Hormone-free | Cramping after insertion |
| Over 99% effective | Requires doctor insertion/removal |
| Immediate return to fertility | Does not protect against STIs |
| Suitable for those avoiding systemic hormones | Not ideal for women with heavy menstrual flow |
7. Condoms (Male and Female)

Condoms act as a physical barrier to prevent sperm from entering the uterus. They are 85% effective with typical use and up to 98% effective with perfect use.
Condoms are best for women or couples who want hormone-free, on-demand contraception and protection against sexually transmitted infections (STIs).
| Pros | Cons / Possible Side Effects |
|---|---|
| Protect against STIs | Lower effectiveness with incorrect use |
| Hormone-free | Can break or slip |
| Easily accessible and affordable | May reduce sensation for some |
| Can be used with other methods | Latex allergy possible |
| No prescription needed | Must be used every time |
8. Diaphragm / Cervical Cap
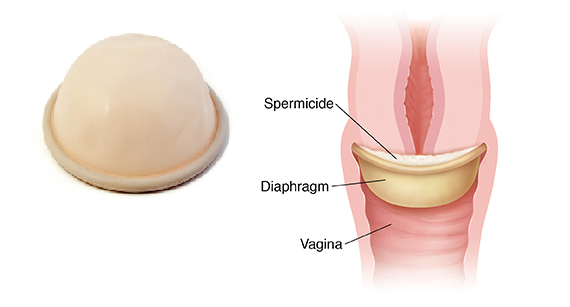
A diaphragm or cervical cap is a reusable device inserted into the vagina to cover the cervix and block sperm, typically used with spermicide. It is 71%–88% effective depending on correct use. This method suits women who prefer hormone-free contraception and are comfortable inserting a device before sex.
| Pros | Cons / Possible Side Effects |
|---|---|
| Hormone-free | Lower effectiveness |
| Reusable for up to 2 years | Must be inserted before sex |
| Can be used only when needed | Needs to stay in place 6 hours after sex |
| No systemic side effects | Increased risk of UTIs |
| Can be combined with condoms | Requires fitting in some cases |
9. Fertility Awareness Methods (FAM)
Fertility awareness methods involve tracking signs such as basal body temperature, cervical mucus changes, and menstrual cycle patterns to identify fertile days. These methods are up to 76% effective with typical use and up to 95–99% effective with perfect use.
They are best for women seeking hormone-free contraception, especially those with regular cycles and the discipline to track daily.
| Pros | Cons / Possible Side Effects |
|---|---|
| 100% hormone-free | Lower effectiveness with inconsistent use |
| Encourages deeper understanding of your cycle | Requires daily tracking |
| No medical procedures | Illness or stress can affect accuracy |
| Supports future pregnancy planning | Requires partner cooperation |
| Free or low-cost (depending on method/app) | Does not protect against STIs |
Struggling with irregular periods? Learn what might be behind it — from hormonal issues to lifestyle triggers.
How to Choose the Right Birth Control Method

Finding the right birth control can feel overwhelming, especially with so many options available. But the best choice is the one that fits your daily routine, period needs, future pregnancy plans, and comfort level. Here’s how to figure out what might work best for you:
Step 1: Your Health and Medical Conditions
Your menstrual preferences can significantly influence which birth control method is right for you. If you’re hoping for lighter, shorter, or even absent periods, hormonal methods are often the most helpful options.
These include:
- Hormonal IUD
- Contraceptive injection
- Combined oral contraceptive pills
These methods can reduce menstrual flow, ease cramping, and are especially beneficial for women with heavy periods, endometriosis, or anaemia.
On the other hand, if you prefer to maintain a natural monthly cycle without hormonal influence, or if you want to avoid changes to your period entirely, non-hormonal methods may be a better fit.
These include:
- Copper IUD
- Condoms
- Fertility awareness methods
These options allow your body to follow its natural menstrual rhythm while still providing reliable pregnancy prevention.
Step 2: Consider Your Lifestyle and Commitment Level
Some birth control methods require daily or monthly attention, while others are completely maintenance-free.
1. “Set it and forget it”
If you want long-term protection with almost no maintenance, long-acting reversible contraceptives (LARCs) are ideal. They stay effective for years and are great for busy women or those who tend to forget daily pills.
These include:
- Hormonal IUD (3–5 years)
- Copper IUD (10 years)
- Implant (3 years)
2. Methods you control daily or monthly
If you prefer a method you can start or stop easily, or want flexibility in case of side effects, short-term options may be a better fit. These require more routine but offer more control.
These include:
- Pill – daily
- Vaginal ring – monthly
- Condoms – use only when needed
3. Natural or hormone-free
If you prefer to avoid hormones, whether for personal, medical, or lifestyle reasons, non-hormonal methods provide effective pregnancy prevention while allowing your natural menstrual cycle to continue.
These include:
- Copper IUD
- Barrier methods (condoms, diaphragm)
- Fertility awareness methods
Step 3: Think About Side-Effect Sensitivity
Every woman’s body responds differently to hormones. Understanding how your body typically reacts can help you avoid unwanted side effects and choose a method that feels comfortable and safe for you.
1. If you want to avoid hormones altogether
Some women prefer to stay completely hormone-free due to past side effects, medical reasons, or personal preference. These methods prevent pregnancy without affecting your natural hormones.
These include:
- Copper IUD
- Condoms
- Fertility awareness methods
2. If you need to avoid oestrogen
Certain medical conditions mean that oestrogen-containing methods are not recommended. Women with migraines with aura, a history of blood clots, uncontrolled hypertension, or those who smoke and are over 35 should avoid combined hormonal contraception.
Safe alternatives include:
- Progestin-only pill (mini pill)
- Hormonal IUD
- Implant
- Contraceptive injection
- Non-hormonal methods
3. If you are sensitive to mood changes or hormonal shifts
Some women notice mood changes, anxiety, or headaches when using certain hormonal methods. If this sounds familiar, choosing lower-hormone or non-hormonal options may lead to better comfort and stability.
Potentially better options include:
- Copper IUD
- Barrier methods
- Fertility awareness methods
- Low-dose progestin options (in some cases)
Step 4: Take Your Medical Conditions Into Account
Your health history and existing medical conditions can influence which birth control method is safest and most suitable.
1. If you have heavy or painful periods
Women who struggle with heavy bleeding, severe cramps, anaemia, or endometriosis often benefit from hormonal methods that lighten or suppress periods. These can significantly reduce discomfort and monthly blood loss.
These include:
- Hormonal IUD
- Combined pill (COCs)
- Contraceptive injection
2. If you have PCOS or hormone-related symptoms
PCOS can cause irregular periods, acne, or excess hair growth. Hormonal methods, especially those containing oestrogen, can help regulate the menstrual cycle and improve these symptoms.
Common options include:
- Combined pills
- Certain pills with anti-androgenic effects (e.g., drospirenone-based pills like Yaz)
3. If you have conditions that make oestrogen unsafe
Some medical conditions make oestrogen-containing contraception too risky. Women with migraine with aura, a history of blood clots, uncontrolled high blood pressure, or smokers above age 35 should avoid combined hormonal methods.
Safer alternatives include:
- Progestin-only pill (mini pill)
- Hormonal IUD
- Implan
- Contraceptive injection
- Non-hormonal methods (e.g., copper IUD, condoms)
Step 5: Align Your Choice With Your Fertility Goals
Your future pregnancy plans can also influence which method works best for you. Some contraceptives allow your fertility to return almost immediately once you stop using them, while others may delay ovulation for several months.
1. If you want a quick return to fertility
Most short-term methods and IUDs allow ovulation to resume shortly after discontinuation. These are suitable if you want to conceive within the next year or simply want flexibility.
2. If you want long-term pregnancy prevention
Long-acting reversible contraceptives (like IUDs or implants) are ideal if you’re not planning a pregnancy anytime soon. They provide durable protection without requiring frequent attention.
3. If you want to avoid delayed ovulation
The contraceptive injection may prolong the return of fertility, sometimes taking 6–12 months for cycles to regulate again. This method may not be suitable if you’re hoping to conceive in the near future.
Step 6: Consider the Cost and Budget Fit
Cost can also influence which birth control method feels right for you. Short-term methods like condoms and pills are usually more affordable upfront, making them suitable if you’re still exploring your preferences or prefer lower initial costs.
On the other hand, long-term methods such as IUDs or implants require a higher upfront cost but tend to be more cost-effective over the years. If you want long-term convenience, reliability, and fewer ongoing expenses, these options often provide the best value.
The Ultimate Birth Control Comparison Table
| Method | Duration | Hormonal? | Best For | Common Side Effects |
|---|---|---|---|---|
| Combined Pill (COC) | Daily | Yes | Women wanting cycle control, lighter periods, acne support | Nausea, breast tenderness, mild headaches, spotting |
| Mini Pill (POP) | Daily | Yes (Progestin-only) | Breastfeeding mothers, those who must avoid oestrogen | Irregular bleeding |
| Hormonal IUD | 3–5 years | Yes | Women wanting long-term, low-maintenance contraception and lighter periods | Irregular spotting in first months |
| Copper IUD | Up to 10 years | No | Women wanting hormone-free, long-term contraception | Heavier periods or stronger cramps (initially) |
| Implant | 3 years | Yes | Women who prefer “set-and-forget” reliability | Irregular bleeding |
| Injection (Depo-Provera) | Every 3 months | Yes | Women avoiding oestrogen or wanting fewer periods | Weight changes, mood changes, delayed fertility return |
| Vaginal Ring | Monthly | Yes | Women who prefer a once-a-month routine | Breast tenderness, nausea, spotting |
| Condoms (Male/Female) | Per use | No | Hormone-free option, STI protection | Possible irritation or breakage |
| Fertility Awareness Methods | Daily tracking | No | Women preferring natural methods & cycle awareness | Requires strict monitoring; irregular cycles may complicate tracking |
Find Your Best Birth Control Method Today!
Choosing the right birth control isn’t just about preventing pregnancy — it’s about protecting your wellbeing, understanding your body, and feeling confident in every decision you make. Whether you’re exploring your options for the first time or looking to switch to a method that suits you better, having trusted medical guidance makes all the difference.
At Island Hospital, our experienced team of Obstetrics & Gynaecology specialists provides personalised contraceptive counselling, comprehensive assessments, and safe access to a full range of birth control options — from pills to long-acting methods like IUDs and implants.
FAQ
Is an IUD painful to insert?
Most women describe IUD insertion as uncomfortable rather than extremely painful. You may feel cramping or pressure for a few seconds during placement. The experience varies from person to person — women who have given birth may find it less painful, while those who haven’t may feel stronger cramps.
Mild cramping for a few hours after the procedure is normal and usually settles with rest or over-the-counter pain relief.
What happens if I want to switch or stop birth control?
Switching or stopping birth control can cause short-term changes such as spotting, delayed periods, or hormonal shifts. These usually settle within a few weeks to months.
If switching methods, your doctor may recommend starting the new method before stopping the old one to avoid any gap in protection. Backup contraception (like condoms) may be needed for about 7 days, depending on the methods involved.
Is continuous contraception safe?
Yes. Taking birth control continuously, such as skipping the pill-free week to avoid monthly periods, is considered safe for most women.
You may experience some breakthrough bleeding in the first few months, which usually improves over time. Your doctor may recommend periodic checks to ensure the method remains suitable for you.
How soon can I get pregnant after stopping birth control?
Fertility can return very quickly after stopping most methods — often within a few weeks. The only exception is the contraceptive injection (Depo-Provera), where ovulation may take several months to return.
If you’re planning a pregnancy, an O&G specialist can help you transition safely and prepare for conception.
Can I use birth control if I have PCOS, endometriosis, or fibroids?
Yes — and in many cases, birth control can actually help manage symptoms.
- Combined pills help regulate cycles and reduce PCOS-related acne.
- Hormonal IUDs help reduce heavy bleeding from fibroids or endometriosis.
Always check with an O&G specialist for personalised advice.
At what age should I stop using hormonal birth control?
Many women can safely use hormonal birth control until age 50–55, depending on their health, risk factors, and whether they still need contraception. Your doctor will assess the safest options for perimenopause.
Does birth control affect libido?
Some women notice changes in sex drive, while others don’t experience any difference. Every body reacts differently. If libido changes persist, switching to another method often helps.
Take Charge of Your Reproductive Health Today – With Expert Care You Can Trust

Choosing the right birth control is a deeply personal decision, and understanding your overall health is the first step toward making the best choice for your body.
To help you stay informed and empowered, we’re offering our Comprehensive Plus Package (Female) at only RM2,799 — a complete, head-to-toe health assessment designed to give you clarity and peace of mind.
What’s Included in Your Screening Experience:
- Full physical examination
- Gynaecological assessment
- Radiological screening
- Cardiovascular assessment
- Urine assessments
- Complete medical report
- Consultation with a Health Screening Physician / Specialist
Note: If you are pregnant or think you might be, please inform our staff during registration.