
05 Jan The Lifelong Impact of a Tongue Tie: Symptoms, Stages & Solutions
The Lifelong Impact of a Tongue Tie: Symptoms, Stages & Solutions
By Island Hospital | Jan 5, 2026 12:00:00 PM
Did you know that your tongue – aside from tasting food – holds the critical ability in helping you to eat, speak, breathe, and even maintain optimal posture. Truth is, the health and mobility of this single muscle have a significant, cascading effect on your overall well-being.
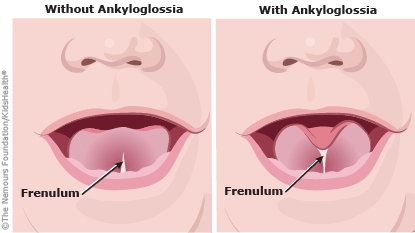
Sometimes, a subtle physical restriction called ankyloglossia or commonly known as a tongue tie, compromises this essential function.
For years, it was often dismissed unless it severely hampered an infant’s feeding. However, we now know that its effects are lifelong.
What starts as a struggle to breastfeed in infancy can quietly evolve into chronic jaw pain, sleep issues, or speech difficulties in adulthood.
Uncover the vital facts you need with this guide highlighting the crucial link between the tongue and overall health. Best of all, it lays out exactly how Island Hospital’s ENT team delivers tailored solutions designed just for you.
The Lifelong Impact: 7 Key Signs You Need an ENT Specialist
Tongue tie is unique because the symptoms change and evolve as a person ages, often leading to compensatory behaviours that mask the underlying problem.
Here are the seven key signs of a restrictive tongue tie, spanning from infancy through adulthood:
| Life Stage | Primary Issue | The 7 Key Signs |
|---|---|---|
| Infancy (0–1 Year) | Feeding & Growth |
|
| Childhood (1–12 Years) | Speech & Oral Function |
|
| Adolescence & Adulthood | Chronic Pain & Airway |
|
Breastfeeding mothers will also face several maternal symptoms if their infant shows signs of tongue tie such as:
- Painful Nipple Compression: Nipple damage, blistering, or bleeding due to the baby chewing instead of sucking.
- Mastitis/Blocked Ducts: Due to inefficient milk removal.
- Low Milk Supply: The body reduces supply when milk isn’t fully drained.
Did You Know? Tongue tie is a relatively common congenital condition, affecting approximately 4% to 10% of newborns globally. However, not all cases require intervention, only those that impact function.
When to Treat: Functional Assessment and Decision-Making
Unlike other medical conditions, the decision to treat a tongue tie is rarely based on appearance alone. It is based on functional limitation—that is, how much the restrictive tissue impacts the patient’s daily life.
1. Normal Tongue vs. Tongue-Tie: How to Tell the Difference
A normal, healthy tongue should be able to:
- Protrude beyond the lower gumline without a deep indentation.
- Elevate easily to the roof of the mouth (palate) and hold that position.
- Sweep the entire upper and lower gums laterally (side-to-side).
A tongue tie often results in a heart-shaped tongue tip when protruded and a clear inability to lift the tongue high enough to create a good seal for feeding or to correctly rest the tongue on the palate.
2. How Island Hospital Doctors Diagnose Tongue-Tie
If you suspect a tongue tie—at any stage of life—the first step is a proper assessment by an experienced specialist.
Diagnosis is a holistic process that goes beyond a quick look. Our ENT specialists use a combination of methods:
- Anatomical Assessment
Looking at the thickness, location, and length of the frenulum (e.g., using a classification scale). - Functional Assessment
This is the most crucial step. We use simple tools and observation to assess the tongue’s full range of motion, its ability to elevate, and its strength.At this stage, your doctor will assess the appearance and elasticity of the frenulum, and evaluating the tongue’s functional movement using standardised tools like the Tongue Tie Assessment Protocol (TTAP) or the Hazelbaker Assessment Tool for Lingual Frenulum Function (HATLFF).
- Symptom History
For adults and children, this involves a detailed discussion about chronic pain, speech clarity, and sleep patterns. For infants, we rely on parental feedback and collaboration with lactation consultants.
3. Monitor vs Treat Guide
| Monitor (Conservative Management) | Treat (Intervention Indicated) |
|---|---|
| Mild restriction with no functional symptoms (e.g., feeding is normal, no pain). | Significant functional symptoms (e.g., failure to thrive in infants, chronic jaw/neck pain in adults). |
| Symptoms are new or mild, and conservative therapies (like specific exercises or lactation support) are showing progress. | Symptoms are severe, chronic, and unresponsive to non-surgical intervention. |
| Waiting for the child to grow to see if natural changes occur. | Risk of long-term functional impairment (e.g., speech impediment, airway compromise). |
The Multidisciplinary Solution at Island Hospital
The treatment for a tongue tie can range from non-surgical therapy to a minor procedure. Critically, surgery alone is often not enough—it requires a team approach.
1. Conservative Management: Non-Surgical Therapies
Before considering a procedure, the Island Hospital team often recommends non-surgical paths, especially for older patients with poor muscle function:
- Lactation Consultancy (Infants): Optimising latch and feeding position can sometimes overcome mild restrictions.
- Myofunctional Therapy (MFT): Often described as physical therapy for the mouth, MFT involves specific exercises to retrain the tongue and facial muscles. This is crucial for adults and children who have spent years compensating for the restricted movement.
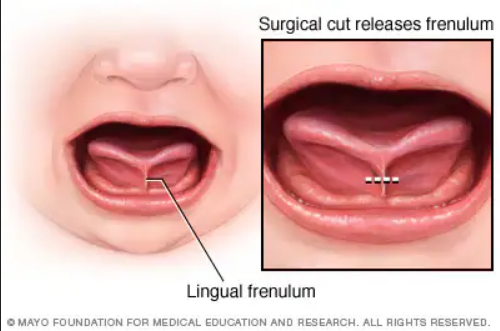
2. Surgical Interventions: Frenotomy and Frenuloplasty
If conservative measures fail or the functional restriction is severe, a procedure may be recommended:
- Frenotomy (The “Snip”)
A simple, quick procedure typically used for infants. The ENT specialist uses surgical scissors or a laser to release the frenulum. Recovery is swift, often allowing feeding to resume immediately. - Frenuloplasty (Surgical Revision)
Reserved for older children and adults, this procedure is more complex and often involves sutures to address a thicker, more fibrous frenulum.
3. Life After Treatment: The Importance of Rehabilitation
The surgery is only the first step. To ensure lasting success and prevent the wound from re-attaching, post-operative care is vital:
- Stretching/Exercises
Healing after a frenotomy requires focused attention to prevent the formation of a new, restrictive scar. Your specialist will provide a specific regimen of post-operative stretches, often called “wound care” or “active wound management.”- Goal: The primary goal is to encourage the open wound to heal “by secondary intention,” meaning it heals with a large, supple diamond shape rather than contracting into a tight, linear scar.
- Procedure: These stretches involve gently lifting and sweeping the tongue to specific locations, typically performed multiple times a day for several weeks.
- Duration: Consistency is key. These brief, frequent exercises are essential for several weeks post-procedure, though the exact duration will be tailored to the patient (infant or adult) and the extent of the initial tie.
- Speech and Myofunctional Therapy
For older children and adults, simply releasing the tissue is usually insufficient. The brain and the muscles have spent years compensating for the restriction, developing ingrained patterns of movement and posture that must be corrected.This is where Myofunctional Therapy (MFT) and, in some cases, Speech Therapy, become non-negotiable for lasting success.
MFT is essentially physical therapy for the tongue and facial muscles. It involves a series of tailored exercises designed to:
- Establish Proper Resting Posture: The correct tongue posture is resting gently against the roof of the mouth (the palate) when the lips are closed. This is vital for promoting nasal breathing, correct swallowing, and healthy facial bone development.
- Improve Swallowing Pattern: Retrain the tongue from a compensatory “thrust” pattern to a healthy, wave-like swallow (where the tongue moves upward and backward). An incorrect swallow can put constant pressure on the teeth and contribute to digestive issues.
- Strengthen and Coordinate the Tongue: Exercises target the newly released muscle fibers, building strength and coordination so the tongue can perform its full range of motion effortlessly.
Did You Know? A tongue tie can affect the shape of the face. When the tongue is restricted and cannot properly rest on the roof of the mouth, it fails to promote the outward and forward growth of the upper jaw (maxilla). Over time, this often leads to a narrower palate and a need for extensive orthodontics or a maxillofacial surgery.
A Path to Better Breathing and Well-being
The lifelong impact of an untreated ankyloglossia can seem daunting, but the good news is that effective, modern solutions are available. Recognising the signs—whether it’s poor latching in an infant, persistent speech delay in a child, or chronic jaw pain in an adult—is the first, most powerful step.
Don’t let a small band of tissue hold you or your loved one back from optimal health.
Contact Island Hospital today to schedule a comprehensive consultation with one of our specialised ENT specialists for full tongue relief.
FAQ
Can tongue tie fix itself as a child grows?
While some mild cases may show improvement as the frenulum stretches naturally with age, a true functional restriction often persists or leads to compensatory muscle habits. It will not “fix itself” if the symptoms are causing significant difficulty (like feeding or speech issues).
Is the procedure safe for newborns?
Yes, frenotomy is a common, minimally invasive procedure for infants. When performed by a qualified specialist, the risks are very low, and the benefits often include immediate improvements in breastfeeding.
What should I expect the surgical site to look like while it heals?
The released area will form a healing patch, often described as a “wet scab” or “diamond” shape.
- Day 1: The wound is typically pink or red.
- Day 2 onwards: The area turns white, yellow, or grey. This is not a sign of infection but is the natural healing tissue (fibrin and collagen) that acts as a bandage in the mouth.
- The healing patch will gradually shrink over the next few weeks until the site is completely healed.
What are some post-operative exercises and after-care treatment I should do after a tongue tie release?
Post-operative stretches are crucial to prevent re-attachment. Your Island Hospital specialist will prescribe a specific protocol, often involving quick, gentle lifts and sweeps under the tongue several times a day for a few weeks. For older patients, myofunctional therapy is recommended to teach the tongue its new, correct resting posture.
Why are post-operative exercises (stretches) so important after a tongue tie release?
Post-operative stretches are crucial because the mouth heals very quickly. The exercises prevent the raw tissue edges from sticking back together (known as reattachment) and forming a new, restrictive band of scar tissue. Consistent movement ensures the wound heals with the maximum possible flexibility and range of motion.






