
24 Oct The Evidence-Based Guide You Need to Overcoming Depression
The Evidence-Based Guide You Need to Overcoming Depression
By Island Hospital | October 24, 2025 10:34:09 AM
Life is full of ups and downs, but sometimes the “downs” feel like they’ve set up permanent residence. When those feelings don’t go away, lingering for weeks, months, or even years, casting a shadow over everything you do, there’s a chance that you might have clinical depression.
According to the National Health and Morbidity Survey 2023, approximately one million Malaysians aged 15 and above suffer from depression, and the number has doubled since 2019. This means about 1 in 20 adults in Malaysia are currently living with depression.
Despite how common it is, the stigma around depression often makes it incredibly difficult to seek help, which is why we’ve created this compassionate space to offer clear, practical, and empathetic advice to help you on your journey toward healing and hope.
Understanding the Difference: Sadness vs. Depression
Sadness is a fundamental human emotion we all feel from time to time, like when you lose something important or experience a setback. It’s a natural, temporary response to a painful event.
Depression, however, is different. It’s a complex medical condition that goes far beyond a low mood. It’s a persistent, intense state of hopelessness and despair that can affect your body and mind.
Unlike sadness, depression is often accompanied by a range of physical and cognitive symptoms that impact every aspect of your daily life, including school, work, and relationships.
Common types of depression include:
- Postpartum depression, which occurs after childbirth. It is a serious mood disorder that can occur in new parents after childbirth, going beyond the temporary “baby blues” and involves more intense and long-lasting feelings of sadness, anxiety, and exhaustion that can interfere with a person’s ability to care for themselves or their baby.
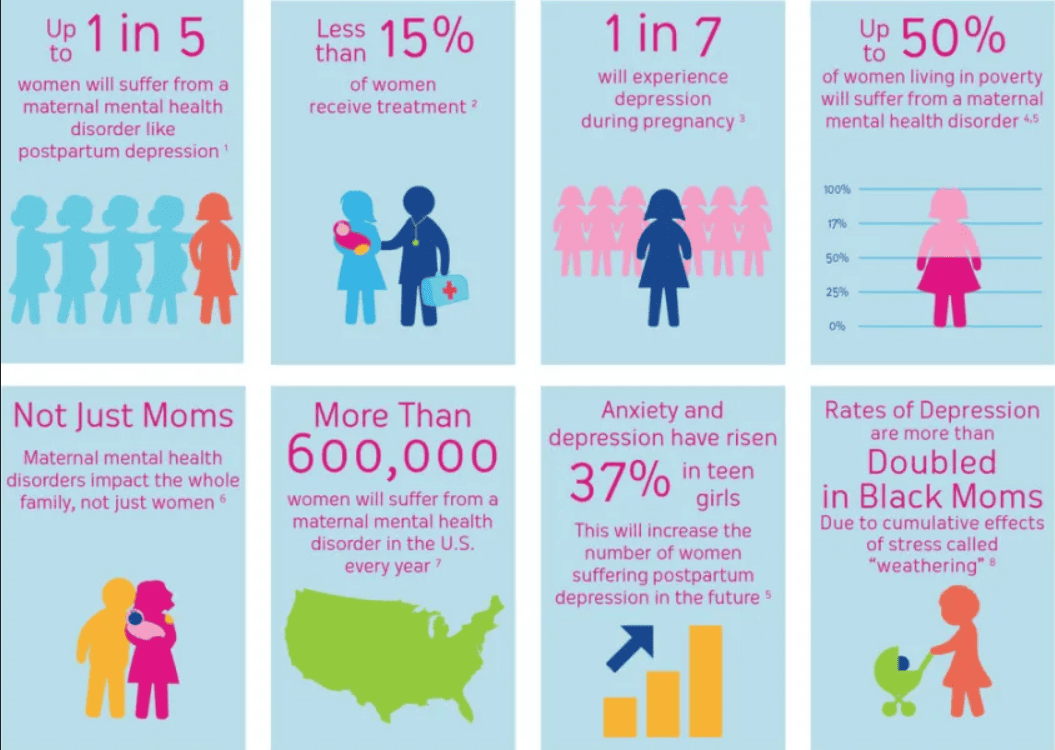
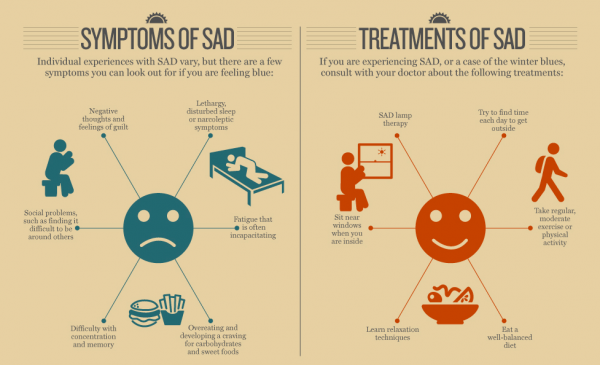
- Seasonal affective disorder (SAD) is a type of depression that has a seasonal pattern. It is most often triggered by the reduced sunlight in the shorter days of autumn and winter. People with SAD tend to experience a loss of energy, changes in appetite, and increased sleepiness during these months, with their symptoms improving as the seasons change to spring and summer.
What Causes Depression?
Depression is not a sign of weakness or a simple lack of willpower where you can simply “snap out of it”. It’s a complex condition with multiple potential causes.
The exact cause is unknown, but it is often a combination of biological, psychological, and environmental factors.
1. Biological Factors
Biological factors play a significant role. An imbalance in brain chemistry, particularly with neurotransmitters like serotonin and dopamine, can disrupt your mood, sleep, and appetite.
Some research also points to a potential link between the gut and the brain, suggesting that gut health may influence mental well-being. This is why a healthy diet is often recommended as part of a holistic approach to managing depression.
2. Psychological and Environmental Factors
Certain personality traits, such as being highly self-critical or a perfectionist, can increase your risk of developing depression. These traits can lead to a cycle of negative self-talk and feelings of inadequacy.
Furthermore, stressful life events can act as a trigger. These include everything from long-term unemployment and difficult relationships to the loss of a loved one or prolonged social isolation.
Medical conditions, such as thyroid disease or autoimmune disorders, can also contribute to or mimic depressive symptoms. Additionally, substance use issues can both trigger and worsen depression, creating a vicious cycle that is difficult to break.
Are You Depressed? A Simple Self-Check
The first step in seeking help is recognising the signs. Doctors often use the mnemonic CIG-E-CAPS to help identify the classic symptoms of depression.
- Changes in sleep
- Interest (loss of interest in hobbies)
- Guilt
- Energy (lack of)
- Concentration (difficulty with)
- Appetite (changes in)
- Psychomotor changes (slowing down or agitation)
- Suicide (thoughts of)
While only a healthcare professional can diagnose depression, you can ask yourself two key questions to gauge if you may be struggling:
- In the past month, have you lost interest or pleasure in things you usually enjoy?
- Have you been feeling sad, down, or hopeless most of the time?
If you answered yes to either of these questions, it may be worth consulting a doctor to explore your feelings and experiences further.
Safety Disclaimer: If you are experiencing suicidal thoughts or are actively planning to harm yourself or others, this is a medical emergency. Immediately call our crisis hotline (+604 226 8527) or go to the nearest emergency room.
You are worth getting help.
Fuel your mind. Nourish your mood. Discover how healthy snacking can be both delicious and a powerful tool for your mental well-being in this article: Little Bites, Powerful Impact: Healthy Snacking for Your Optimal Health.
When to Seek Help

Seeking help for your mental health is a sign of strength, not weakness. Reaching out is appropriate whenever your symptoms persist for more than a couple of weeks, begin to interfere with your ability to function in your daily life, or if you feel like you’re struggling to complete even simple tasks.
Urgent Situations
It’s crucial to seek immediate help if you or someone you know is in crisis. This includes situations where there are thoughts of self-harm, an inability to care for oneself, or if symptoms are rapidly worsening.
In such urgent situations, you should go to the nearest emergency department or contact a crisis hotline for immediate support.
What to Expect When You See a Doctor
When you decide to see a doctor about your mental health, it’s a big, positive step. Your doctor is there to help, and their goal is to understand what you’re experiencing so they can recommend the best course of action. Generally, they will focus on three main areas during your visit:
1. Ruling Out Other Causes
The first thing your doctor will do is a thorough check to ensure your symptoms aren’t caused by something else. They may ask about your medical history or recommend blood tests to rule out other medical conditions, like a thyroid problem or a vitamin deficiency, that could be mimicking the symptoms of depression. They will also inquire about external factors, such as substance abuse, which can significantly impact your mental state.
2. Identifying Triggers and Patterns
Your doctor will want to understand the timeline of your symptoms. They’ll ask about any recent stressful events in your life, such as a major life change, grief, or a difficult breakup, to identify potential triggers.
They’ll also explore whether your symptoms follow a specific pattern, for example, if they only appear during certain times of the year, which could indicate something like Seasonal Affective Disorder (SAD).
3. Evaluating Severity and Risk
This is a critical part of the assessment. Your doctor will ask questions to gauge how severely your depression is affecting you and if there are any immediate risks. They will especially focus on assessing any thoughts of self-harm, as your safety is their top priority. It’s important to be honest in this conversation so they can provide the right level of support.
Questions to Ask Your Doctor
To help you feel more prepared and in control of your appointment, consider writing down some questions in advance. Here are a few you might find helpful:
- What kind of depression do I have?
- Should my treatment plan include medication, psychotherapy, or both?
- What are the potential side effects of the medication you’re recommending, and what should I expect?
- Are there any lifestyle changes I can make—like changes to my diet, exercise, or sleep habits—that could help with my symptoms?
Who Should You Consult?
When dealing with symptoms of depression, the first step is to talk to a general practitioner (GP) or a family doctor. They can provide an initial assessment, rule out any other medical conditions that might be causing your symptoms, and refer you to a mental health professional if needed.
For a formal diagnosis and treatment plan, a psychiatrist is the specialist you should consult. A psychiatrist is a medical doctor who specialises in the diagnosis, treatment, and prevention of mental, emotional, and behavioral disorders.
Unlike psychologists or counselors, they can prescribe medication and other medical treatments, as they are medically trained to understand the complex relationship between your physical health and mental state.
Evidence-Based Treatment Options
Recovering from depression is a journey, and most people find the best results by combining different strategies. This often includes psychotherapy, lifestyle changes, and, in some cases, medication.
1. Psychotherapy
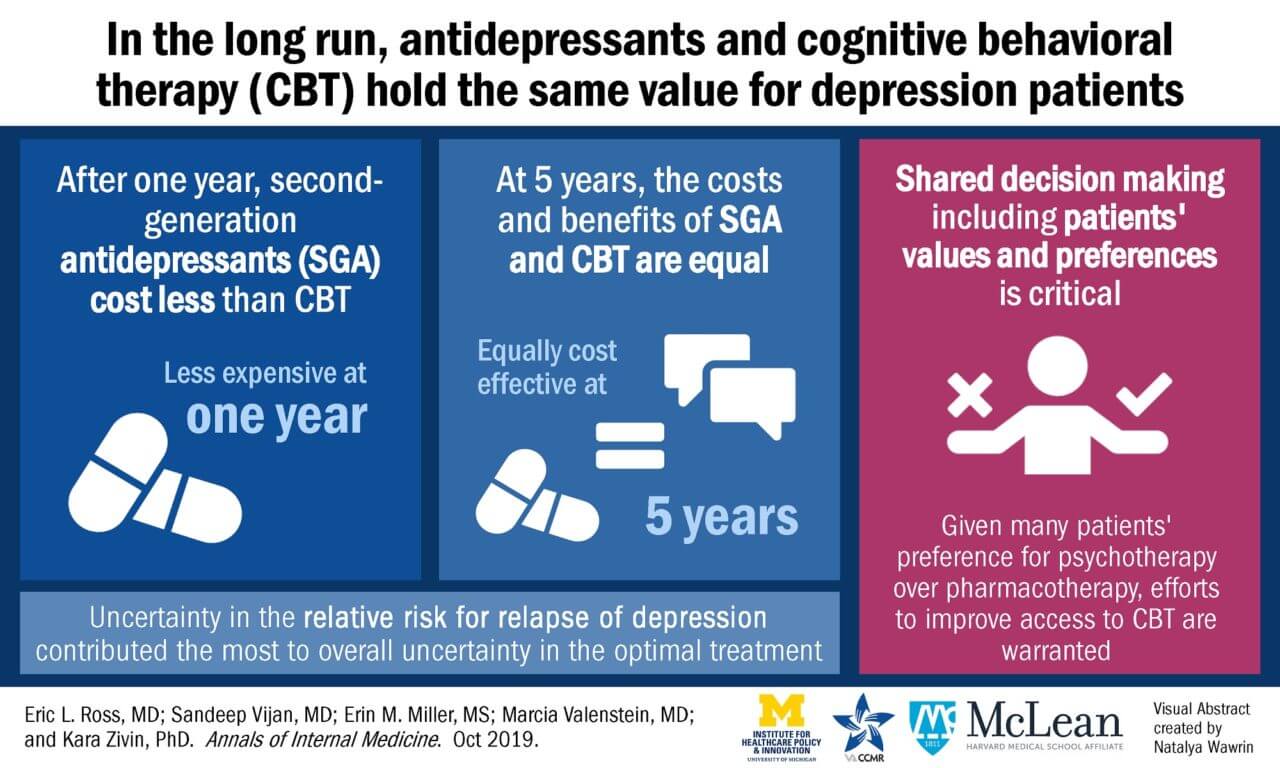
The most effective and widely studied form of talk therapy for depression is Cognitive Behavioral Therapy (CBT). The core principle of CBT is that depression is often maintained by negative and inaccurate thought patterns about yourself and the world. Through CBT, you learn to identify, question, and ultimately reframe these thoughts.
For example, imagine you are trying to eat healthy but you slip up and eat a scoop of ice cream. Your immediate, negative thought might be, “I’m a failure and I can’t stick to anything.” This thought can trigger a downward spiral, causing you to give up on your diet entirely.
In CBT, you learn to pause and challenge that thought, reframing it as, “It was just one scoop; I’m being too hard on myself. I can get back on track with my next meal.”
This process helps you break the cycle of negative thinking and build healthier, more realistic thought patterns. Research shows that CBT can be as effective as medication alone, and combining the two often leads to the best outcomes.
2. Lifestyle Modifications (The NESTS Framework)
While not a cure on their own, lifestyle changes can significantly improve your mood and support your recovery. The NESTS framework is a simple, evidence-based guide to these changes:
- Nutrition: A balanced diet, such as the Mediterranean diet, can positively impact your mood and brain health. Foods rich in omega-3 fatty acids and antioxidants have been linked to better mental well-being.
- Exercise: Numerous studies have shown that regular physical activity can be as effective as some antidepressant medications for treating mild to moderate depression. Aim for at least 30 minutes of moderate exercise, like a brisk walk, three times a week.
- Sleep: Depression can severely disrupt your sleep patterns. Establishing a consistent bedtime routine—like avoiding screens an hour before bed and creating a comfortable sleep environment—can help improve the quality of your rest, which is essential for mental and physical health.
- Time for yourself: Make time for hobbies and activities you enjoy. Whether it’s reading a book, listening to music, or spending time in nature, these moments of self-care can help you recharge and reduce stress.
- Support: Social connection is a powerful antidote to the isolation often associated with depression. Actively connecting with friends, family, or a support group can help you feel understood and less alone.
3. Medication
Antidepressants aren’t a “magic pill,” but they are a powerful tool that can help speed up the recovery process, especially for moderate to severe depression. It’s important to understand that they take time to work. You may begin to notice an initial impact in three to four weeks, but the full effect can take up to three or four months to become apparent.
Medication is typically used for about one year after a first episode of depression to help prevent a relapse. If one type of medication doesn’t seem to be working, don’t get discouraged. There are many different classes and types of antidepressants available, and your doctor can work with you to find the one that is most effective for you.
Don’t just live with sleepless nights. Find out how this Malaysian Sleep Study can help you unlock better, more energized days.
Coping Tools and Daily Practices
Incorporating small, manageable actions into your daily routine can make a significant difference in managing your symptoms.
- Daily mood tracking: Keeping a mood diary can help you identify triggers and see what activities, people, or places affect your feelings most. This awareness is the first step toward making positive changes.
- Weekly “small wins” checklist: When low motivation makes big tasks feel impossible, break them down into tiny, achievable steps. For example, instead of “clean the room,” your goal could be “put one item away.” Celebrating these small wins builds momentum and a sense of accomplishment.
- Simple routines: Establishing a consistent daily routine—such as waking up at the same time each day, eating regular meals, and having a bedtime ritual—can provide a sense of stability and control when you’re feeling overwhelmed.
- Find a creative outlet: Engaging in creative activities like drawing, painting, dancing, or writing can be a powerful way to process difficult emotions and reduce stress without having to use words.
Overcoming Barriers
Stigma, low motivation, and the cost of treatment are significant barriers to recovery, but they can be overcome.
- Acknowledge the stigma: Many people feel a sense of shame, but remember that depression is a medical condition, not a personal failing. Seeking help is a sign of courage and strength.
- Break tasks into micro-steps: On days when it’s hard to even get out of bed, focus on one tiny task, like drinking a glass of water or standing up and stretching for 30 seconds.
- Seek out affordable resources: Don’t let cost be a barrier. Many organisations and government agencies offer low-cost or free mental health services. Online platforms and support groups can also provide valuable, accessible resources to help you get started.
Your Journey to Healing Starts Now
Depression is a treatable illness, and you don’t have to navigate it alone. We can work together to normalise mental illness by talking openly about it, ensuring everyone has access to the information and support they deserve.
If you’re ready to seek help, remember that reaching out is an act of courage, not weakness. Island Hospital’s Psychiatry Department will be your guide in understanding your options and taking that crucial first step can begin your journey toward a life filled with hope, healing, and well-being.
FAQs
1. How do I know if I’m depressed or just going through a rough patch?
It’s common to have periods of sadness, but depression is different. If you’ve been feeling sad, hopeless, or have lost interest in things you usually enjoy for more than two weeks, and these feelings are interfering with your daily life, it’s a good idea to seek a professional opinion. A doctor or a mental health professional can provide a proper diagnosis and guidance.
2. Will I need to take medication forever?
For a first episode of depression, a doctor will typically recommend taking medication for about a year after your symptoms have significantly improved. This helps to prevent a relapse. For those who have had multiple episodes or have more severe symptoms, longer-term treatment might be recommended as a preventative measure. Remember, the goal is always to find the most effective and sustainable treatment for you.
3. Can depression come back after I recover?
Yes, depression can return. However, this doesn’t mean your recovery was a failure. By continuing to practice healthy lifestyle habits, like regular exercise and a balanced diet, and staying in touch with your care team, you can build resilience and significantly reduce your risk of a relapse. Think of it as managing a chronic health condition—consistent care and healthy habits are key.
4. How can I support a friend or family member with depression?
The best way to support someone is to listen without judgment. Avoid offering quick fixes or saying things like “just cheer up.” Instead, offer your presence and empathy. You can encourage them to seek professional help and offer practical assistance with small, daily tasks that may feel overwhelming to them, such as making a meal or running an errand.
5. How long does depression usually last?
With proper treatment, many people see significant improvement within a few months, but everyone’s journey is different. Recovery is a gradual process that requires patience and consistency. The key is to stick with your treatment plan, even on days when it feels difficult, and trust that with time and care, you can begin to feel better.






