19 Apr Testicular Cancer: Rare but also common
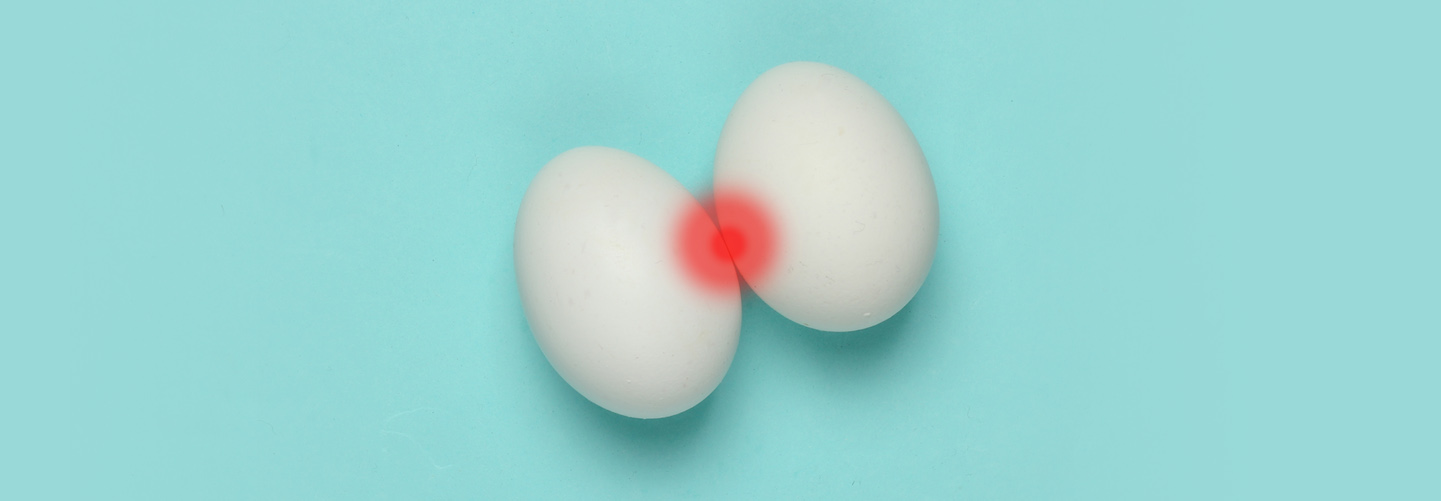
Testicular Cancer: Rare but also common
By Island Hospital | Aug 8, 2025 5:00:08 PM
The most common type of testicular cancer is a germ cell tumour.
Germ cell tumours are divided into two types:
- Seminomas
Slow-growing tumours are the most common type of germ cell tumour in men with testicular cancer.
Seminomas are further split into two types, one being classical seminoma and the other being spermatocytic seminoma.
The first type occurs in men of all ages, while the second type is more likely to occur in older people, and it also does not spread as much as other tumours.
- Nonseminomas
Uncommon but also much more aggressive tumours that spread quickly and are usually made up of more than one type of cancer cell.
Nonseminomas tend to develop in younger men or children, although they are rarer than seminomas.
Men’s health is crucial to look out for, and there are 4 top common diseases affecting them. Here’s what you need to know.
When the healthy cells in the testicle begin to mutate and divide uncontrollably, testicular cancer begins to form.
Even with current technology and research, the exact cause of the mutation of the cells and testicular cancer is still unknown.
Some known risk factors that may raise the likelihood of testicular cancer are:
- An undescended testicle (cryptorchidism)
As a baby, the testicles will form and then move into its proper position below the penis (into the scrotum) before birth.
Some men are born with one undescended testicle (or, in rare cases, both are undescended), and this condition occurs more often in boys who are born prematurely.
The development of the testicles might be affected in men with undescended testicles, and as a result, their risk of testicular cancer is higher.
- Klinefelter syndrome
Females are born with two X chromosomes (XX) while males are born with an X and Y chromosome (XY).
When a boy is born with an extra X chromosome (XXY), it results in a genetic disorder known as Klinefelter syndrome.
Klinefelter syndrome can affect the growth of the testicles and production of testosterone, which in turn may increase the risk of testicular cancer in a man.
- Family history
If a man has first-degree relatives (parents or siblings) who have testicular cancer, he is also at a higher risk of developing testicular cancer.
- Age
Approximately 50% of testicular cancer cases occur in teenagers and young men, usually affecting those between the ages of 15 and 35.
However, it can also develop at any age and is known to affect men in their 60s.
- HIV
A person with HIV is at a higher risk of developing germ cell tumours, especially testicular cancer.
The good news is that testicular cancer is highly treatable regardless of whether the cancer is contained within the testicle or if it has spread beyond the testicle.
Treatment for testicular cancer may be one of or a combination of the following:
- Surgery
The primary treatment for testicular cancer (regardless of stage) is the removal of the testicle via surgery, known as a radical inguinal orchiectomy.
The surgeon will make an incision in your groin and then extract the testicle from the opening. If needed, a prosthetic testicle can be inserted to replace the removed testicle.
In some cases, the surrounding lymph nodes may also need to be removed via surgery to reduce the risk of cancer recurrence, especially if the cancer is advanced or has spread beyond the testes.
- Radiation therapy
Radiation therapy (or radiotherapy) uses high-powered energy beams to kill cancer cells.
It is an option of treatment for men who have developed seminoma type of testicular cancer, and may also be used to kill any remaining cancer cells after a testicle removal surgery.
The radiation exposure may reduce the sperm count or even affect the fertility in some men; make sure you talk to your doctor if you want to preserve your sperm before radiotherapy.
- Chemotherapy
Chemotherapy is a form of treatment where drugs are used to kill cancer cells. The drugs will travel throughout the body to attack cancer cells that have spread beyond the original tumour.
Germ cell tumours (seminoma and nonseminoma) are especially sensitive to chemotherapy, and as such, testicular cancer is highly treatable with chemotherapy.
In rare cases where the cancer has already travelled beyond the testicle during diagnosis, chemotherapy may be used to kill or reduce the size of the cancer cells before surgery to remove the testicle is carried out.
A type of germ cell called teratoma does not respond well to chemotherapy and requires surgery to be removed.
Because nonseminomas often present multiple different types of cancer cells, a person whose cancer contains teratoma will require both surgery and chemotherapy for successful treatment of testicular cancer.
While we can’t pinpoint the exact cause of testicular cancer, and therefore cannot make specific recommendations, early detection can help reduce the risk of it getting severe.
The easiest way to detect early changes in your testicles is by carrying out a testicular self-examination (TSE).
- TSE is best performed after a shower, when the muscles in your body and the scrotum are relaxed.
- Stand in front of a mirror and visually inspect your scrotum. Look for any noticeable changes in the size of the testicles, and check for any signs of swelling or changes in the skin.
- It is normal if one of your testicles is slightly larger or hangs lower than the other one.
- Then, examine both testicles with your hands. Use one hand for each testicle; use the thumb and fingers to feel for any lumps or swelling.
As you regularly perform TSE, you will eventually feel more comfortable and familiar with the structure of your testicles.
This will help you detect lumps or abnormalities more effectively than before. Ideally, you should carry out a TSE once or twice a month after a shower and do it while standing in front of a mirror.
Some men do not discover testicular cancer until they visit the doctor for a physical examination, while others find it during TSE.
A lump in the testicle does not necessarily confirm testicular cancer, so your doctor may use the following methods for a diagnosis:
- An ultrasound test
- Blood tests to check for cancer or tumour markers in the blood
- Computerised Tomography (CT) scan
- MRI (Magnetic resonance imaging)
A majority of cancers have positive outcomes when detected and treated early. In fact, testicular cancer is one of the most treatable forms of cancer.

We’re offering our comprehensive Plus Package for Men at only RM2,499 – giving you a complete head-to-toe health assessment for peace of mind.
Our package features vital health screenings, including Cardiovascular Assessment, Cancer Markers, Radiological Screening, Stool Assessment, Kidney Function Test, and much more.
What’s Included in Your Screening Experience:
✔ Physical examination
✔ Complete medical report
✔ Consultation by Health Screening Physician
✔ Light refreshments
✔ Exclusive Island Hospital woven bag






