Nephrology
SPECIALTY
Nephrology
Restore your kidney health with advanced diagnostics, personalized therapy and kidney transplant. Our nephrology specialists expert in diagnosing and managing kidney disease and condition, including hypertension, kidney stones, and End-Stage Renal Disease (ESRD).
Expert Kidney Care and Nephrology in Malaysia
Kidneys are vital organs that responsible for filtering waste, regulating blood pressure, and balancing fuilds. The damage or failure or kidneys will cause symptoms such as nausea, fatigue, weaken bones, and difficulty to concentrate. Without proper treatment, these kidney disease can impact a person’s quality of life.
At Island Hospital, our team of the best nephrologists in Penang, Malaysia is dedicated in providing customize and effective treatment plan to cure all kidney-related condition, from early-stage kidney disease to chronic renal failure, including renal injuries, kidney infection, kidney stones, and kidney cysts.
For patients experiencing kidney failure, we also offer kidney transplant surgery to help restore kidney function. Using the latest diagnostic tools and advanced technologies, our nephrologists in Malaysia strive to preserve kidney health and enhance the life quality of our patients.
Make An Inquiry if you have any more questions.
Conditions and Treatments
Procedures offered and conditions treated for nephrology at Island Hospital includes (but not limited to) the following:
- Kidney Stones
- Chronic Kidney Disease (CKD)
- End-Stage Renal Disease (ESRD)
- Kidney Infections
- Hypertension-related kidney disease
- Dialysis
- Kidney Transplant
- Surgical removal of kidney stones
- Antibiotics for kidney infections
- Immunosuppressive therapy
Kidney Transplant
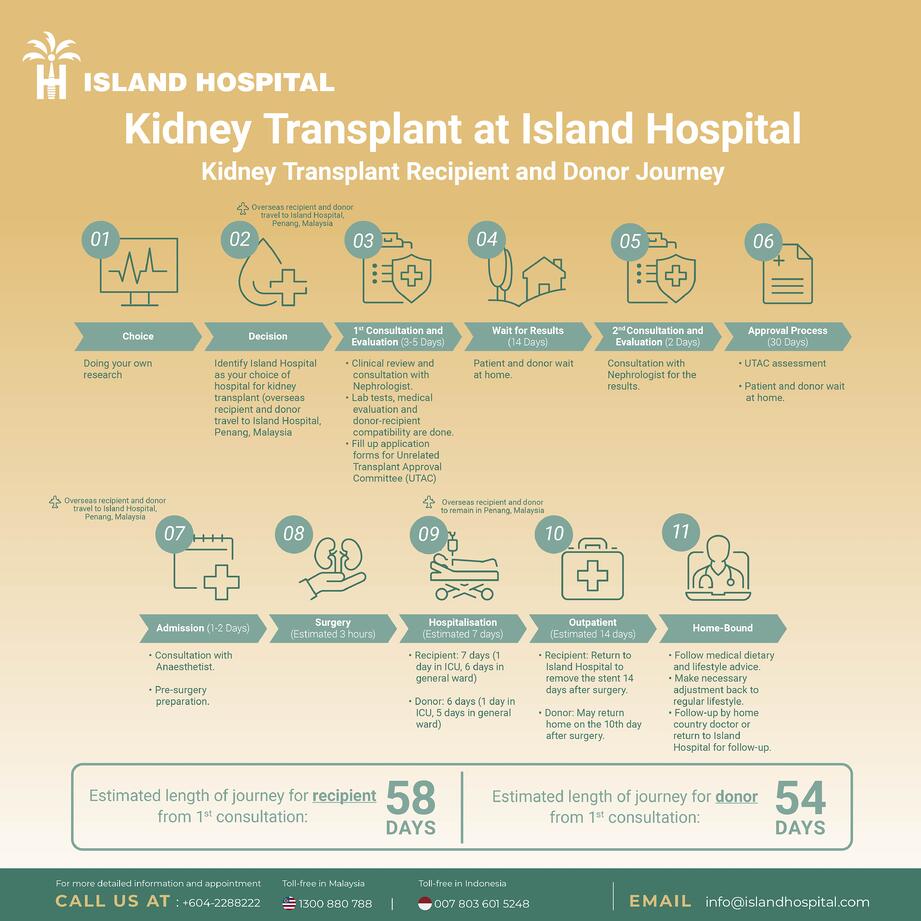
1) Choice
Doing your own research.
2) Decision
Identify Island Hospital as your choice of hospital for kidney transplant (overseas recipient and donor travel to Island Hospital Penang, Malaysia).
3) 1st Consultation and Evaluation (3-5 Days)
- Clinical review and consultation with nephrologist.
- Lab tests, medical evaluation and donor-recipient compatibility are done.
- Fill up application forms for Unrelated Transplant Approval Committee (UTAC)
4) Wait for Results (14 Days)
Patient and donor wait at home.
5) 2nd Consultation and Evaluation (2 Days)
Consultation with Nephrologist for the results.
6) Approval Process (30 Days)
- UTAC assessment
- Patient and donor wait at home
7) Admission (1-2 Days)
Overseas recipient and donor travel to Island Hospital, Penang, Malaysia.
- Consultation with Anaesthetist
- Pre-surgery preparation
8) Surgery (Estimated 3 hours)
9) Hospitalisation (Estimated 7 days)
Overseas recipient and donor to remain in Penang, Malaysia.
- Recipient : 7 days (1 day in ICU, 6 days in general ward)
- Donor : 6 days (1 day in ICU, 5 days in general ward)
10) Outpatient (Estimated 14 days)
- Recipient : Return to Island Hospital to remove the stent 14 days after surgery.
- Donor : May return home on the 10th day after surgery.
11) Home-Bound
- Follow medical dietary and lifestyle advice.
- Make necessary adjustment back to regular lifestyle.
- Follow-up by home country doctor or return to Island Hospital for follow-up.
Normal Kidney Functions
Most people are born with two kidneys on either side of the spine, behind the abdominal organs and below the rib cage. Kidneys are shaped like kidney beans. The kidneys perform several major functions to keep the body healthy and alive. Our kidneys:
- filter blood to get rid of waste products by passing it from the body as urine, while returning water and chemicals back to the body as needed
- regulate blood pressure by releasing several hormones
- stimulate the production of red blood cells by releasing the hormone erythropoietin.
When working well, it produces urine. Urine is then carried to the bladder through the ureter like pipes. It stays in the bladder until the body senses that it is full and thus releases the urine from the bladder through the urethra.
What is kidney failure?
When the kidneys stop working, waste products and metabolites start accumulating in the blood, leading to renal failure. If it persists (chronically), end-stage renal disease occurs and either dialysis or transplantation is required.
Common causes of end-stage renal disease
- Diabetes mellitus (Types 1 and 2)
- High blood pressure
- Glomerulonephritis (a group of diseases that injure the part of the kidney that filters blood (called glomeruli), marked especially by blood or protein in the urine and by edema)
- Polycystic kidney disease (genetic disorder that causes many fluid-filled cysts to grow in the kidneys)
- Severe anatomical problems in the urinary tract
Treatments for End-stage Renal Disease
The treatments for end-stage renal disease are:
- Hemodialysis – a mechanical process of cleaning the blood of waste products
- Peritoneal dialysis – waste products are removed by passing chemical solutions through the abdominal cavity
- Kidney transplantation.
While none of these treatments cure end-stage renal disease, a transplant may offer the closest thing to a normal life because the transplanted kidney can replace the failed kidneys. However, it also involves a life-long dependence on medicine (which may have severe side effects) to ensure the transplanted kidney works well.
In some cases, dialysis patients who also have severe medical problems such as cancer or active infections may not be suitable candidates for a kidney transplant.
Types of kidney transplant done in Island Hospital
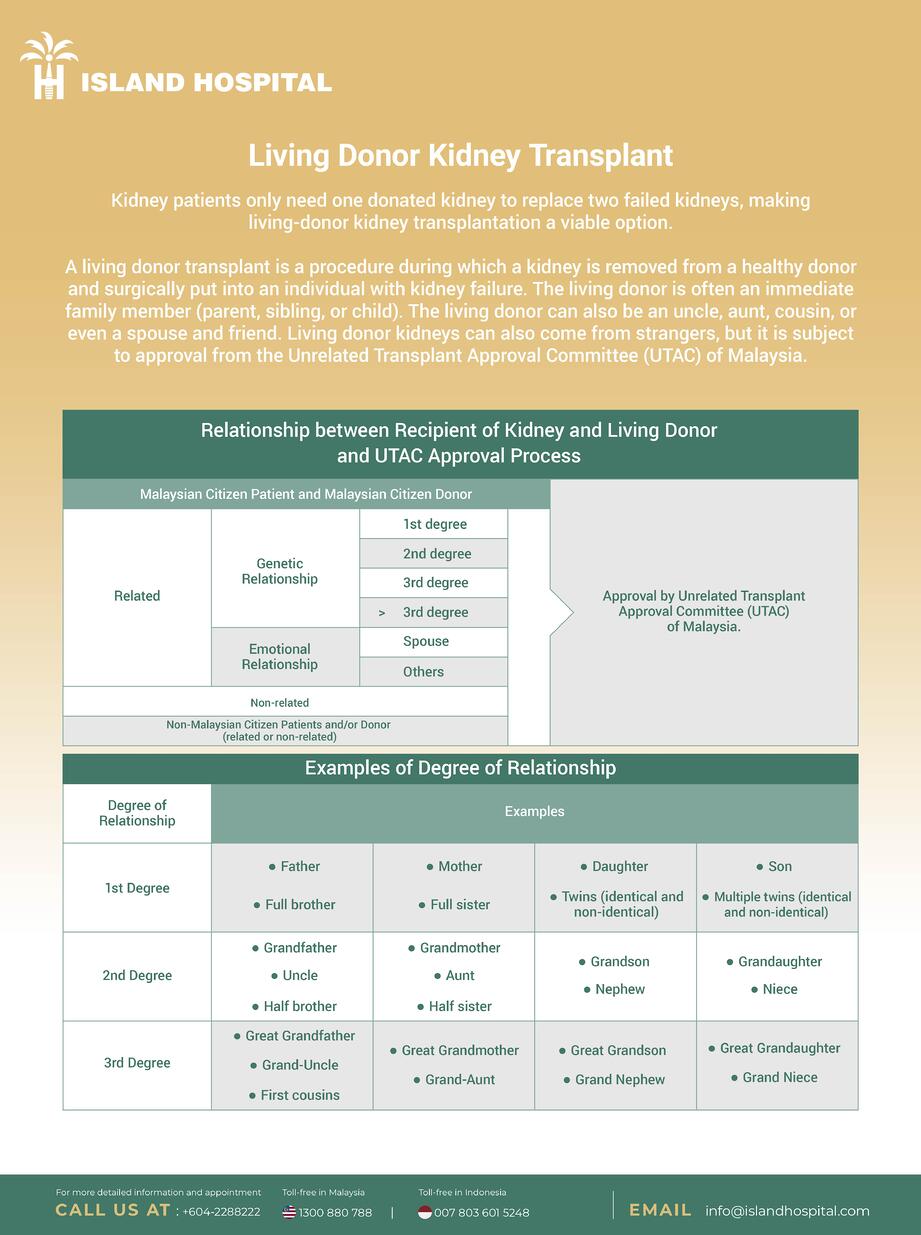
A kidney transplant is the transfer of a healthy kidney from one person into the body of a person who has little or no kidney function. Typically, kidney transplants can be done from a deceased donor or living donor. At Island Hospital, we perform only with living donors.
Living Donor Kidney Transplant
Living Donor Kidney Transplant vs. Deceased Donor Kidney Transplant
A living donor transplant has many advantages over a deceased donor, the most important being that it has a significantly higher success rate. Additional reasons may include:
| Living Donor Kidney Transplant | Deceased Donor Kidney Transplant |
| The transplanted kidney generally works immediately after the transplant. | The transplanted kidney could possibly take several days or weeks to function normally. |
| The transplant can be scheduled, giving the recipient and donor preparation time. | There is no way to know when a deceased donor kidney will be available, and surgery must be performed immediately after it is available. |
| A lower risk of rejection, especially if the kidney is donated by a blood relative. | A higher risk of rejection by the body. |
| Potentially reduces the waiting time to receive a kidney transplant. | The average wait time could be from three to five years or longer. |
Why are kidney transplants done?
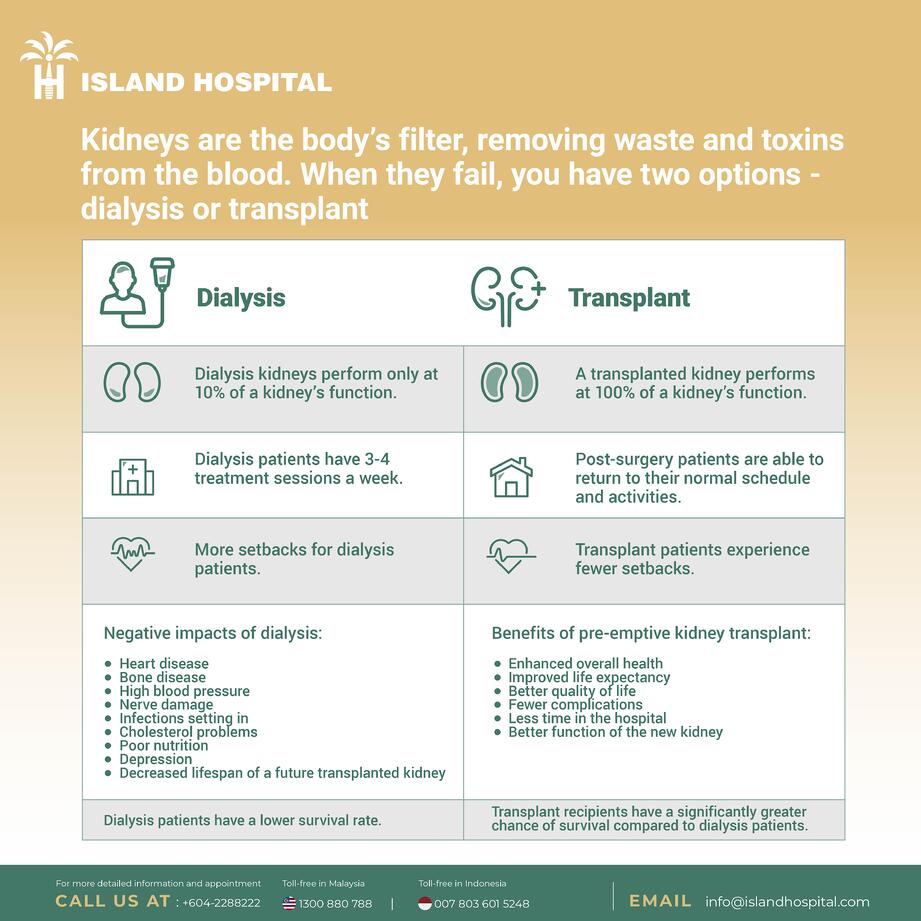
There are pros and cons to both dialysis and kidney transplants.
| Kidney Transplant | Dialysis (Hemodialysis) |
| Less time and effort required to meet with doctor | Takes a lot of time Frequent trips per week to a dialysis centre. |
| Reduced long-term cost of dialysis | Labour-intensive Requires medical professional assistance every visit |
| A more active and normalised life with fewer dietary restrictions | Frequent discomfort Requires patient to have needles inserted into them every visit. They have to sit there for hours and may feel tired after each visit. Strict dietary restrictions. |
| Lower risk of death | Higher risk of medical complications and death |
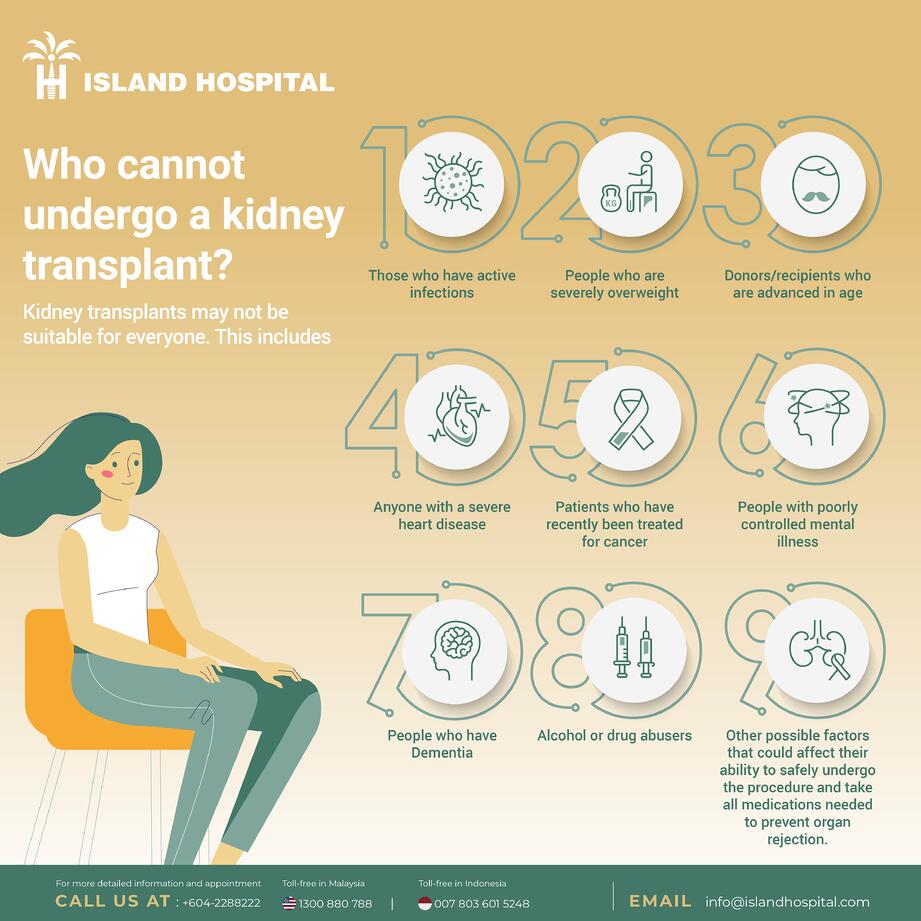
Although kidney transplant is the treatment of choice for End-Stage Renal Disease (ESRD), the procedure may not be suitable for everyone as there are a number of factors to consider. To ensure the safety and longevity of both the patient and the donor, the following conditions must be considered before the procedure can be carried out.
Kidney transplants may not be suitable for everyone. This includes people who have/are:
- active infections,
- severely overweight,
- advanced in age,
- severe heart disease,
- recently treated for cancer,
- poorly controlled mental illness,
- dementia,
- alcohol or drug abuse, and
- any other factor that could affect their ability to safely undergo the procedure and take the medications needed to prevent organ rejection
Risks and complications of kidney transplant
Kidney transplant surgery carries the risk of significant complications, including:
- Bleeding
- Blood clots
- Cancer that can be transmitted with the donated kidney
- Death
- Failure of the donated kidney
- Heart attack
- Infection
- Infection from the donor
- Leaking from or blockage of the tube (ureter) that links the kidney to the bladder
- Rejection of the donated kidney (although rare)
- Stroke
- Urological complications
- Vascular complications (vein and artery clotting or narrowing)
Also, kidney transplant is a major surgery. Therefore, it may have the surgical risks of:
- Allergic reaction to general anesthesia
- Bleeding during operation
- Blockage of the ureter
- Blood clots
- Failure of the donated kidney
- Heart attack
- Infection
- Leakage from the ureter
- Lymphoceles (a collection of lymphatic fluid within the body leading to potential renal failure)
- Rejection of the donated kidney
- Stroke
Anti-rejection medication side effects
After a kidney transplant, patients need to take medications to help prevent their body from rejecting the donor kidney. However, these immunosuppressant drugs can lead to some unpleasant side effects such as:
- Acne
- Bone thinning (osteoporosis)
- Bone damage (osteonecrosis)
- Diabetes
- Excessive hair growth or loss
- High blood pressure
- High cholesterol level
- Higher infection risk
- Higher risk of developing certain skin cancers and non-Hodgkin’s lymphoma
- Puffiness (edema)
- Weight gain
It is best to discuss with your doctors these risks and complications which are generally low in a well-optimised patient.
If your doctor recommends that a kidney transplant be done, you will need to be referred to a licensed kidney transplant hospital, like Island Hospital. You can also find out if your insurance covers the transplant costs (pre-operation, operation and post-operation) and has a panel of hospitals to offer.
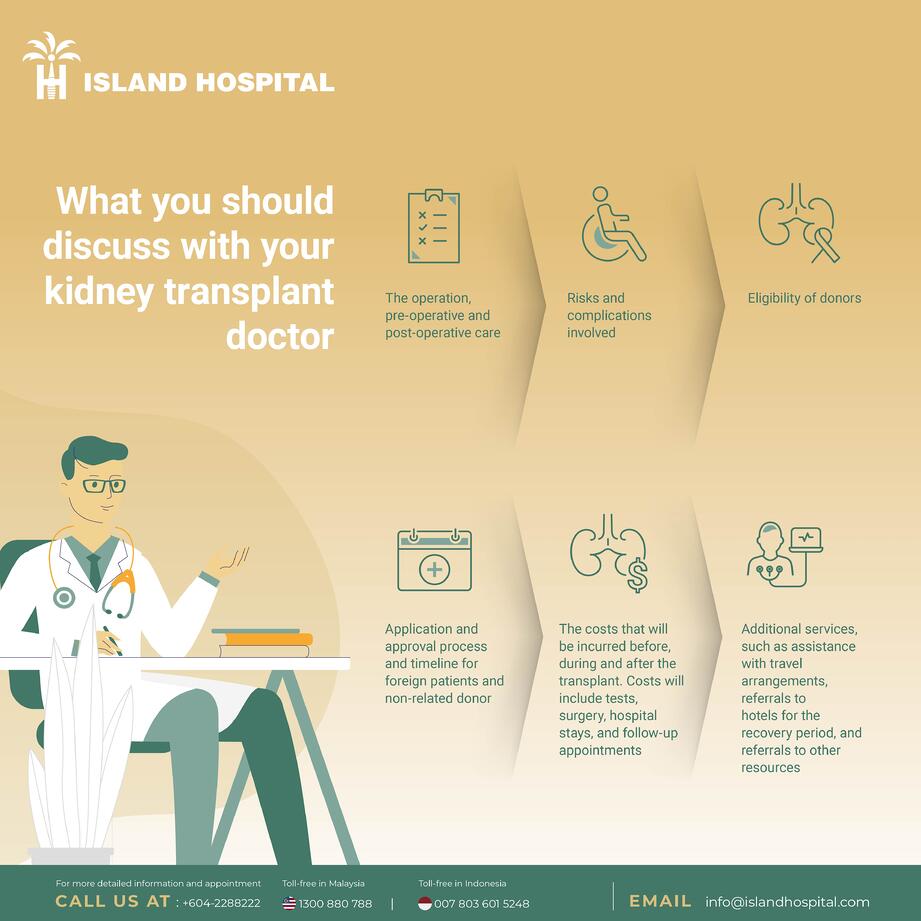
When you consult with our nephrologists at Island Hospital, we can share in-depth information on:
- The operation (pre-operative and post-operative care)
- Risks and complications involved
- Eligibility of donors
- Application and approval process and timeline for foreign patients and non-related donors
- Costs incurred before, during and after the transplant. This includes tests, surgery, hospital stay, and follow-up appointments
- Additional services such as assistance with travel arrangements, referrals to hotels during the recovery period, and referrals to other resources
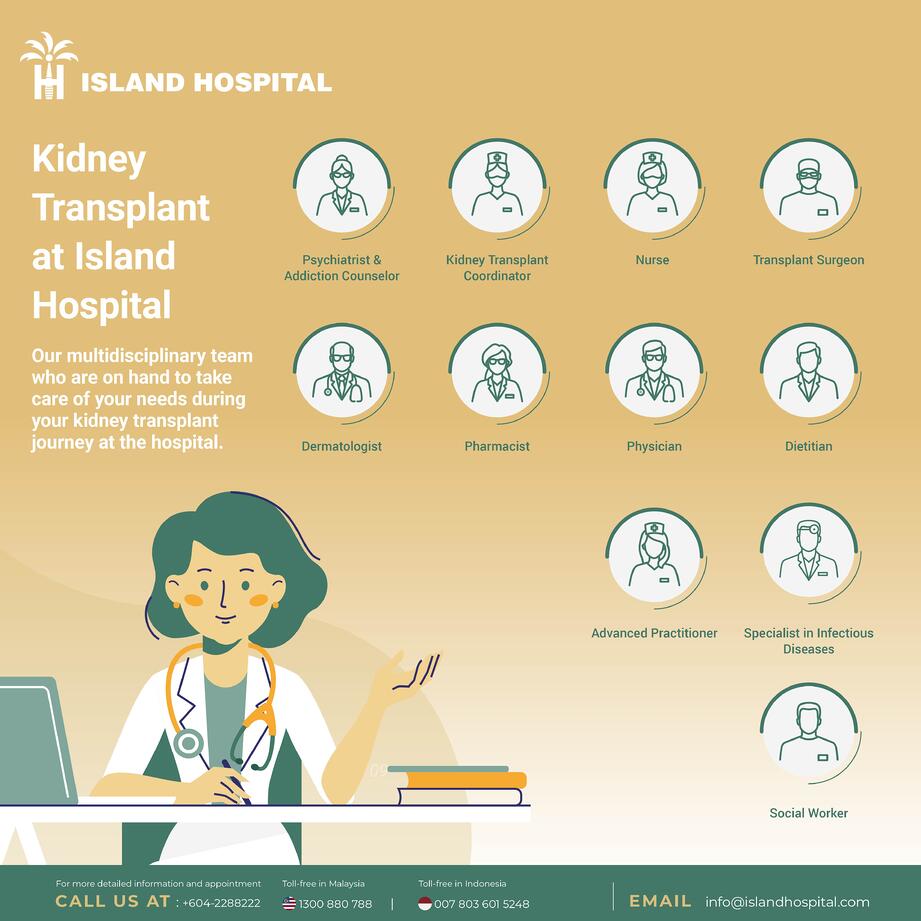
- Island Hospital’s Team Approach in Kidney Transplant
At Island Hospital, our facility, an integrated team of doctors trained in kidney diseases (nephrologists), renal transplant surgery (urologist), infectious disease management, and other specialties is focused on the needs of the patient and his family. Nephrologists, surgeons, doctors, transplant nurses, pharmacists, and others work together to manage every aspect of the patient’s kidney transplant, from planning through to post-surgical care.
Having all of this sub-specialised expertise solely focused on you means that you are getting care from the entire team and not just getting one opinion. At the same time, patient care is discussed among the team, test results are made available quickly, and appointments are scheduled in coordination so that the whole team can work together to determine what is best for the you.
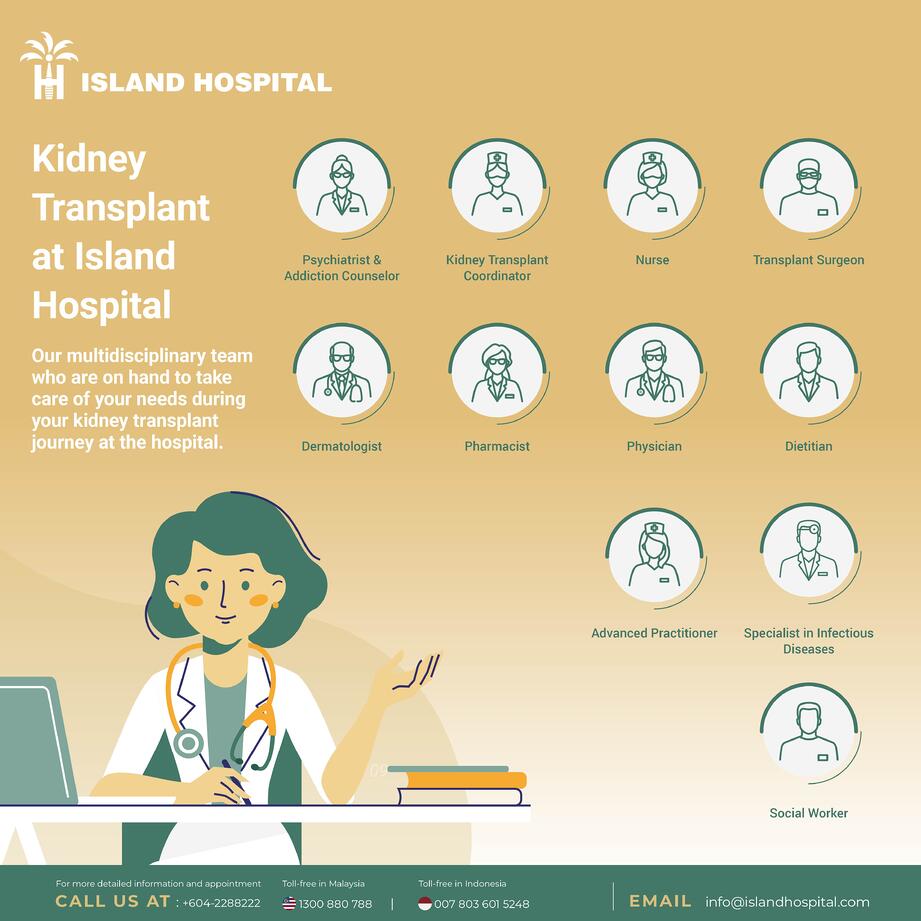
Transplant Surgeon:
Nephrologists:
Other medical professionals include:
- Specialist in infectious diseases
- Internists
- Anaesthetists
- Psychiatrist
- Dietitians
- Nurses
- Medical coordinators
- Pharmacists
Facilities at Island Hospital
- Fully licensed and experienced Kidney Transplant Unit that provides transplant patients with comprehensive and specialised care.
- Intensive Care Unit (ICU) facilities to ensure seamless post-operative care and monitoring
- Well-trained specialised ICU nurses who support patients through the whole process
Evaluation process and finding a match
After you have selected Island Hospital as the transplant centre of choice and your donor, you will be evaluated medically to determine whether you and your donor meet the eligibility requirements for a kidney transplant, which may take several days.
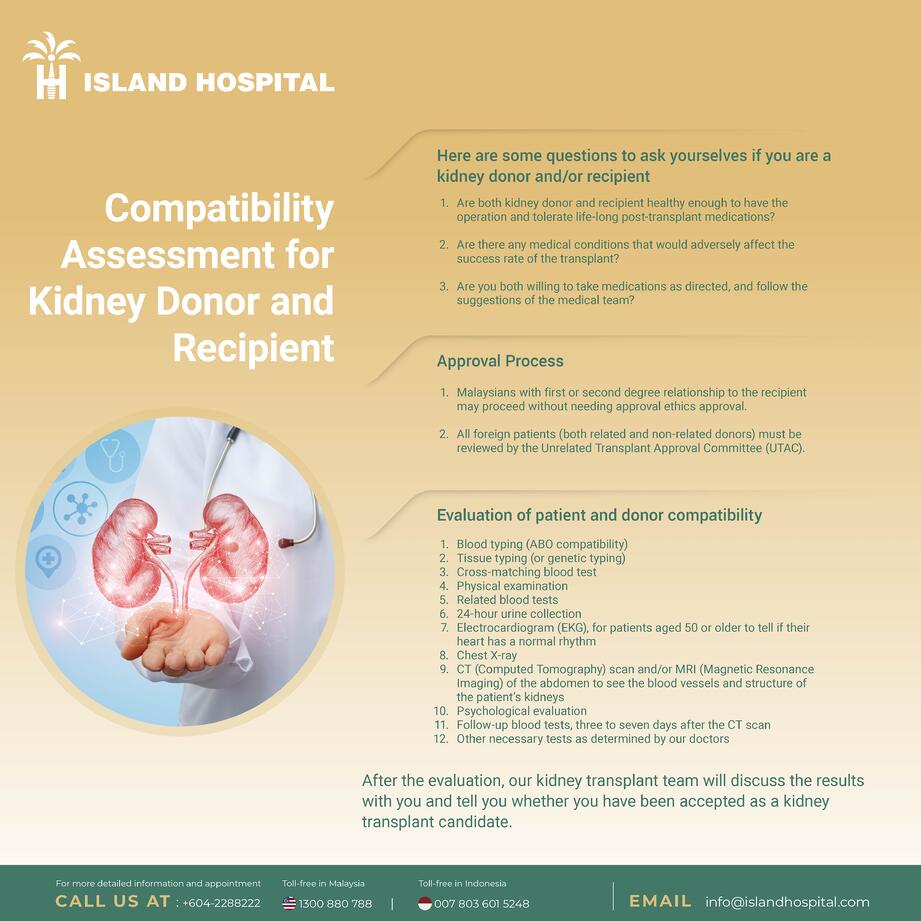
The team will assess whether you and your donor:
- Are healthy enough to have the operation and tolerate life-long post-transplant medications
- Have any medical conditions that would affect adversely the transplant success
- Are willing and able to take medications as directed and follow the suggestions of the medical team
Medically speaking, a kidney donor can be alive, deceased, related, or unrelated to the patient. However, transplant laws may differ as certain countries may have different criteria on who can be a lawful donor. Our transplant team will consider several factors when evaluating whether a kidney donor will be a good match for you before submitting all test reports to the Unrelated Transplant Approval Committee (UTAC) of Malaysia for approval.
- For local Malaysian patients with first or second degree relationship to the recipient, transplants can proceed without needing additional ethics approval (more details below)
- All foreign patients (both related and non-related donors) must be reviewed by the Unrelated Transplant Approval Committee (UTAC)
After your medical examination confirms that you are a suitable candidate for kidney transplant, the next step is to evaluate both you and your donor for compatibility.
It all begins with a blood test which will determine your donor’s blood type and whether it is compatible with yours. If it is compatible, two more blood tests will be done (tissue typing and cross-matching).
1. Blood Typing (ABO Compatibility)
A match is good if the donor and recipient have compatible blood types. This increases the chances of the recipient’s body accepting the new kidney.
Blood typing is the first blood test to check the blood type compatibility between the patient and donor.
If their blood type(s) does not match, the donor may not be able to donate his kidney to the patient.
A simple blood test is able to determine the blood type. The four basic blood types are A, B, AB and O. (Type O is the most common blood type and anyone of any blood type can accept type O.)
| Donor’s blood type | Blood types which can accept donor’s kidney |
| O | O, A, B, AB |
| A | A or AB |
| B | B or AB |
| AB | AB |
2. Tissue typing (or genetic typing)
Tissue typing (human leukocyte antigen (HLA) typing) is a blood test that matches the number of antigens that you and your recipient share. These antigens can recognise differences between their body tissues. This test also compares genetic markers which can tell how likely the transplanted kidney will last.
Each person has six basic tissue typing antigens (or markers) shared equally from their parents. A parent and child would have at least a 50 percent match while sibling can have a zero to 100 percent match.
The best tissue type for you, the recipient is to have a six out of six antigens match (a zero mismatch), something which is possible.
It is not necessary for all antigens to match in order to have a successful transplant. Sometimes, even one matched antigen could work.
3. Cross-matching
Cross-matching is a blood test carried out at least twice you and your donor and recipient to see if there is any reaction to your donor’s kidney.
It involves mixing a small sample of your blood with your in the lab. The test determines whether antibodies in your blood will react against specific antigens in your donor’s blood.
If there is no reaction, the result is a negative cross-match, paving the way for a transplant surgery.
But even if you have passed all other tests, yet you are found to have a positive cross-match (your body would attack the new kidney), the surgery cannot be done unless you go through additional treatment before and after the transplant to reduce the risk of your antibodies reacting to your donor’s kidneys.
Other tests
Other tests on you and your donor in the donor evaluation which may take several days include:
- a thorough physical examination
- blood tests
- 24-hour urine collection
- Electrocardiogram (EKG), for patients aged 50 or older to tell if their heart has a normal rhythm
- chest X-ray
- CT (computed tomography) and/ or MRI (magnetic resonance imaging) of the abdomen (to see the blood vessels and structure of your kidneys)
- Psychological evaluation
- follow-up blood test three to seven days after the CT scan
- Any other necessary testing as determined by our doctors
After the evaluation, our kidney transplant team will discuss the results with you, and advise if you have been accepted as a kidney transplant candidate.
Living kidney donation
Getting a willing living kidney donor is an option other than waiting for a compatible deceased-donor kidney to be available.
Family members are often the most likely to be compatible living kidney donors. But successful living-donor transplants are also common with kidneys donated from emotionally related non-family donors such as friends. This is subject to approval from the ethics committee in the Unrelated Transplant Approval Committee (UTAC) of Malaysia, which takes about 14 days.
Staying healthy
Staying healthy and active is vital whether you are waiting for a donated kidney or your transplant surgery is already planned. It may also help to speed up your recovery from surgery. Make effort to:
- Take your medications as instructed
- Stick to the guidelines of diet and activities
- Turn up at all appointments with your doctors
- Engage in healthy activities, including relaxing and spending time with family and friends
- Stay in touch with your doctors and let them know of any significant changes in your medical condition.
What to bring to the hospital
Here are some suggestions for your convenience during your hospital stay:
- A current list of your medicines, including the dosage and the times you take them.
- Your mobile phone charger.
- Personal care items such as towels, toothbrush, toothpaste, denture cleanser, skin care products, comb, deodorant, make-up and/or shaving kit.
- Storage containers for your glasses or contacts if you wear them. Label the containers with your name.
- A storage container and extra batteries for your hearing aids if you wear them. Label the containers with your name.
- Your own gown/robe if you do not wish to wear the hospital’s.
- Shorts or undergarments to wear underneath your hospital gown/robe.
- Warm clothing if you expect it to be cold.
- Clothing to wear home, including socks, shoes (supportive with nonslip soles), undergarments, shirt and loose pants or a sweat suit.
- Leave Valuables at home or with your family. You may want to bring a little money to buy newspapers or magazines.
What you may want to think about if you live alone
For your convenience, there are certain things you would want to manage before getting admitted:
- Have drinking water prepared at home.
- Find someone to do your gardening.
- Arrange to have your newspaper and mail delivered to your door rather than outside, as needed.
- Arrange transportation to get your groceries, and attend doctor and clinic appointments instead of driving.
- Find someone to help care for your pet, if needed.
- Prepare and freeze a few meals before your surgery.
What to do on the day before surgery
Tell your doctor if you have any changes in your physical condition (fever, cold, dental problems, sore throat, urinating problem) or skin condition (rash, cuts). Surgery may need to be postponed.
(See instructions on pre-surgical food and drink guidelines )
What to do on the evening before surgery (admission may be 1 day or more before the surgery)
- Do not eat a heavy meal before the surgery.
- Take all drugs the hospital gives.
- Take a shower or bath with a special soap. Washing your skin with this soap removes any bacteria on the skin. It also helps prevent infection around the incision. To clean your skin, do the following steps:
- Do not use the soap on your face.
- Wash your rectum and genital areas last.
- Rinse the soap with plain water.
- Dry yourself with clean towels.
- Do not put lotion on your skin after cleansing.
- Do not eat or drink any liquids – even water – after midnight. Your surgery can be delayed or canceled if you don’t follow this instruction.
What to do on the morning of surgery
- Take your morning medicine(s) as directed, with a small sip of water.
- Take a shower (or bath) with the special soap.
- Reach the hospital two hours before your surgery.
Directions on Food and Liquid Before Surgery
The following are based on your arrival time to the hospital, not your scheduled surgery time.
Smoking, Vaping or Chewing Tobacco: Do not smoke, vape, chew tobacco or use any other tobacco products up to 24 hours before your scheduled arrival time. This will reduce the risk of complications. If you do use tobacco products within 8 hours of your scheduled arrival time, your surgery may be delayed or canceled.
Alcohol: Do not drink alcohol up to 24 hours before your scheduled arrival time.
Solid Food: You may eat your regular meals up to 8 hours before your scheduled arrival time.
Solid Food: You may eat a light meal up to 6 hours before your scheduled arrival time.
A light meal is:
- 2 pieces of toast with a light topping
- 1 granola or protein bar
- 1 cup (250ml) oatmeal or other hot cereal — and one of these:
- 450ml of milk, coffee (with or without cream), juice (with or without pulp) or a sports drink.
Clear Liquids: Drink clear liquids up to 2 hours before your scheduled arrival time.
Clear liquids are only these:
- water
- fruit juice without pulp
- sports drinks
- soda
- black coffee without cream or creamer
- tea without cream or creamer.
Drink 350ml – 600ml of electrolyte sports drink (Gatorade® or Powerade®) 2 hours before your scheduled arrival time.
Hard Candy and Gum:
- You may have hard candies (such as a lemon drop or throat lozenge) or chew gum up to 2 hours before your scheduled arrival time.
- You may use gums and lozenges for tobacco cravings up to 2 hours before your scheduled arrival time.
Medicines: Take your medicines as directed with a small sip of water.
During the procedure
Details of procedure
Kidney transplants are done with you and your donor under general anesthesia, so that you are unconscious during the procedure. The surgical team also monitors the heart rate, blood pressure and blood oxygen level throughout the procedure.
- The surgeon makes an incision and places the new kidney in your lower abdomen, just above one of your legs, and connects it to your blood vessels. Unless your own kidneys are causing complications such as high blood pressure, kidney stones, pain or infection, they are left intact. Usually, the left kidney of the donor will be taken due to easy access, unless the left kidney’s function is lower than that of the right.
- The final step is connecting the ureter from the donor kidney to the bladder.
- In most cases, the kidney will soon start producing urine.
After the procedure
After your kidney transplant, you can expect to:
1. Spend about a week in the hospital.
Our medical team will monitor your condition in the operation recovery area to monitor possible signs of complications. Your new kidney will produce urine just like how your own kidneys did when they were healthy and most often, it starts immediately. In other cases, it may take several days. You may expect aches or pain around the operation site while you’re healing.
Most kidney transplant patients can return to work and other normal activities within three to eight weeks after the procedure. Patients are not encouraged to lift objects weighing more than 5kg or do vigorous exercise other than walking until the wound has completely healed (usually about six weeks after surgery).
2. You need to go for frequent check-ups as you continue to recover.
Close monitoring is necessary for a few weeks. You may need blood tests several times a week and have your medications adjusted in the weeks after your transplant. If you live in another city or country, you may need to make arrangements to stay near the transplant centre.
3. Take medications the rest of your life.
You’ll need to take a number of medications after your kidney transplant. Drugs called immunosuppressants (anti-rejection medications) help keep your immune system from attacking and rejecting your new kidney. Additional drugs help reduce the risk of other complications, such as infection, after your transplant.
Results
After a successful kidney transplant, you will no longer need dialysis because the new kidney will filter your blood.
You’ll need medications to suppress your immune system to prevent your body from rejecting your donor kidney. Because these anti-rejection medications may make your body more vulnerable to infection, your doctor may also prescribe antibacterial, antiviral and antifungal medications.
After the transplant, skin check-ups with a dermatologist to screen for skin cancer are vital and it is recommended to keep your health screening (including cancer screening) up-to-date.
Depending on your health condition, ability to withstand surgery and expectations on the quality of life, there are several possible courses of actions for you if your new kidney fails:
- Consider a 2nd transplant
- Resume dialysis
- Stop all treatments
Managing Your Life After Kidney Transplant
It is important to plan ahead these things for your life after kidney transplant as you adapt to the new lifestyle:
- Join or set up your support group
Talking with others who have the same experience as you is important to help ease your stress. Having a group of positive friends and family to be there for you also helps to smooth things out. - Get connected on social media
Sharing and connecting with people online can be helpful in exchanging tips and positivity to help you get into your new life with greater ease without the burden of meeting up. - Getting rehabilitation services
Having rehabilitation support really helps when you are going back to the workforce after a kidney transplant. - Set realistic expectations and milestones for yourself
Life after transplant may not be the same. Don’t stress yourself by having expectations that are not realistic. Go with the flow and pace yourself accordingly. - Learn more about your condition
Find out as much as possible on things with regards to your conditions. Knowledge can empower you to be in better control of your health and it can also liberate you from illogical fears. - Maintaining a new nutrition and exercise plan
Regular exercise helps to increase energy levels and strength. It also helps you maintain a healthy weight, reduce stress and prevent complications such as high blood pressure and cholesterol levels. Your dietitian at Island Hospital will give you guidelines and help on healthy food options and ideas to use in your nutrition plan. It is important to take note of what he/she says to ensure that you stay healthy to prevent chronic diseases from complicating your situation.
It is important to understand as much as possible as you manage chronic kidney diseases and consider kidney transplant as an option. Speak to us as soon as possible to understand more and be better prepared.
Nephrology FAQs
A nephrologist is medical doctor who speciaize in diagnosing and managing kidney-related disease such as kidney stones, kidney infections, and hypertension related to kidney. They conduct diagnosis and guide patients throughout the entire treatment process.
Common symptoms of kidney disease include fatigue, swollen legs or ankles, changes in urination, urine with foam, and shortness of breath. These symptoms could be overlooked in the early stages. Therefore, it’s crucial to undergo routine medical check-ups.
Kidney disease can be caused by chronic health conditions such as high blood pressure, diabetes, infections, as well as the use of certain medications. Unhealthy habits like prolonged excessive salt intake and chronic dehydration can also result in kidney disease or kidney failure.
Chronic kidney disease cannot be cured. However, medical treatment and lifestyle changing can slow down its progression and improve the condition. In such cases, treatments are used to control and prevent further damage.
If you have kidney-related symptoms or concerns, book an appointmont to consult with our best nephrology doctor in Malaysia.
Practice a healthy diet and lifestyle to maintain blood pressure and blood sugar at healthy levels. Healthy habits include drinking more water, quitting smoking, exercising regularly, and avoiding overly salty foods. Regular health screenings are important to detect kidney-related issues early and receive proper treatment before the condition worsens.
Yes, high blood pressure could be the cause of result of kidney disease. Kidneys are crucial in regulating blood pressure. When kidneys are damaged, they will have problems regulating blood pressure properly. Therefore, managing blood pressure is important in maintaining kidney health.