09 Jan Top 5 PCOS Treatments Your Gynecologist Recommends (Diet & Drugs)
Top 5 PCOS Treatments Your Gynecologist Recommends (Diet & Drugs)
By Island Hospital | Jan 9, 2026 12:00:00 PM
If you’ve been grappling with irregular periods, sudden acne, or unexplained difficulty conceiving, you might be one of the millions of women worldwide—affected by Polycystic Ovary Syndrome (PCOS).
A new diagnosis or ongoing struggle can feel overwhelming and isolating. We see you, we understand the frustration, and we believe it’s time to move beyond managing symptoms to truly thriving with this condition.
Island Hospital’s in-depth guide will walk you through understanding the condition, receiving an accurate diagnosis, and exploring all available treatment paths tailored to your specific health goals—whether it is managing symptoms, achieving pregnancy, or preventing long-term complications.
What is Polycystic Ovary Syndrome (PCOS)?
PCOS is a complex endocrine and metabolic disorder characterised primarily by a persistent hormonal imbalance. While the name suggests a problem with the ovaries, the underlying causes are systemic, involving multiple body systems.
The Core Issues of PCOS
PCOS is typically defined by a combination of three key factors:
-
Irregular Periods and Hormonal Imbalance
A fundamental feature of PCOS is an imbalance of reproductive hormones. Specifically, women with PCOS often have higher-than-normal levels of androgens (often called “male hormones,” such as testosterone).
This excess androgen disrupts the normal menstrual cycle, preventing the ovary from releasing an egg (ovulation) each month. It will lead to irregular, infrequent, or absent menstrual periods. The failure to ovulate is the primary driver of both irregular cycles and fertility issues in PCOS.
-
Insulin Resistance
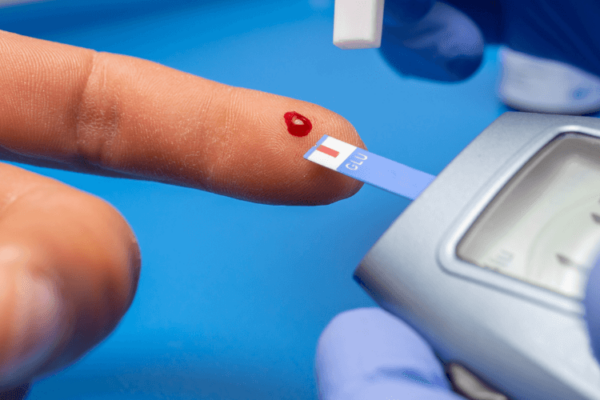
In most individuals with PCOS, the body’s cells do not respond effectively to the hormone insulin, which is responsible for regulating blood sugar. This condition is known as insulin resistance.
In response, the pancreas produces even more insulin. High levels of insulin can, in turn, signal the ovaries to produce more androgens, further exacerbating the hormonal imbalance and PCOS symptoms.
-
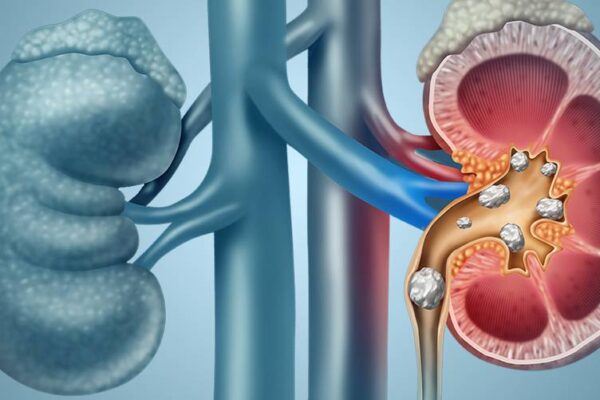
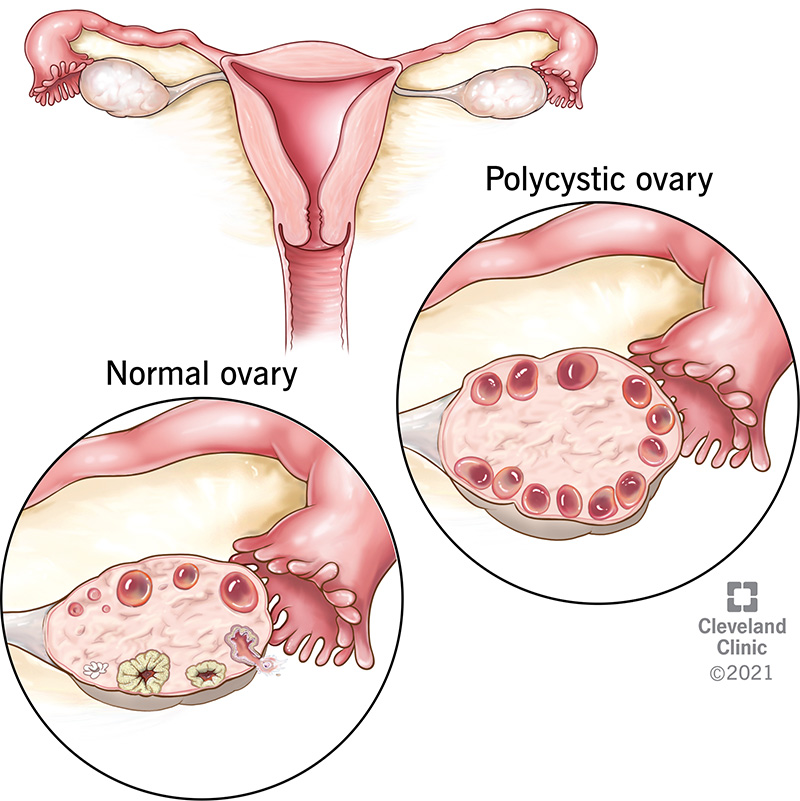
Cysts in the Ovaries: A Misleading Name
The term “polycystic” is often misunderstood. It does not mean you have large, painful cysts that need immediate removal.
In fact, the “cysts” are not true cysts but rather a large number of harmless, underdeveloped follicles (sacs containing eggs) that have stalled in their development due to the lack of proper ovulation.
On an ultrasound, these appear as small, pearl-like formations. It is critical to understand that not all women with PCOS will have polycystic ovaries visible on an ultrasound, and conversely, not all women with polycystic ovaries will have PCOS. Diagnosis requires meeting specific criteria beyond just this single finding.
Struggling with irregular, infrequent, or absent menstrual periods? Learn more about the causes of late periods in our article: Why is My Period Late?
Who is at Risk of Developing PCOS?
While the exact cause of PCOS remains unclear, a combination of genetic and environmental factors is believed to play a role. You may be at an increased risk if:
- You have a family history
If your mother or sister has PCOS, your risk is significantly higher, suggesting a strong genetic component. Far from being a guaranteed fate, this family link is a powerful call to action.
For those with a known history, proactive genetic risk assessment and targeted screening offer the chance to turn a potential diagnosis into an opportunity for early intervention. This means you can begin essential lifestyle management strategies now, effectively mitigating the condition’s severity.
- You have insulin resistance or Type 2 Diabetes
As insulin resistance is a central feature of PCOS, conditions that contribute to it (such as obesity and diabetes) increase this risk. - You have chronic low-grade inflammation
Research suggests that women with PCOS often have higher levels of inflammation, which can stimulate the ovaries to produce androgens.
Recognising PCOS Symptoms
The symptoms of PCOS vary greatly from woman to woman. No two cases are exactly alike, but they typically become noticeable in the late teens or early twenties.
| Symptom Category | Manifestation |
|---|---|
| Menstrual Irregularities | Infrequent periods (fewer than eight per year), very light periods, or periods that stop completely. |
| Excess Androgen Signs |
|
| Metabolic Changes | Weight gain or difficulty losing weight, particularly around the abdominal area, and the development of Acanthosis Nigricans (darkening and thickening of the skin, often in the armpits or neck). |
PCOS Without Classic Symptoms (Lean PCOS)
It is a common misconception that PCOS only affects women who are overweight or experience visible hair growth. This is not true.
A growing number of women are diagnosed with Lean PCOS, meaning they are at a healthy weight and may not show the classic signs of hirsutism or severe acne.
In these cases, the primary symptoms are often menstrual irregularity and fertility difficulties. This highlights the need for thorough diagnostic testing, as the condition is not always visually apparent.
PCOS Diagnosis
Diagnosing PCOS requires a careful and holistic evaluation by a specialist, such as an OB&GYN consultant. There is no single test for PCOS. Instead, doctors rely on clinical assessment, medical history, and specific diagnostic tests to meet internationally recognised criteria.
1. The Gold Standard: The Rotterdam Criteria
Most gynaecologists, including our Obstetrics and Gynaecology specialists at Island Hospital, rely on the Rotterdam Consensus Criteria for diagnosis. To be diagnosed with PCOS, a woman must exhibit at least two out of the following three criteria:
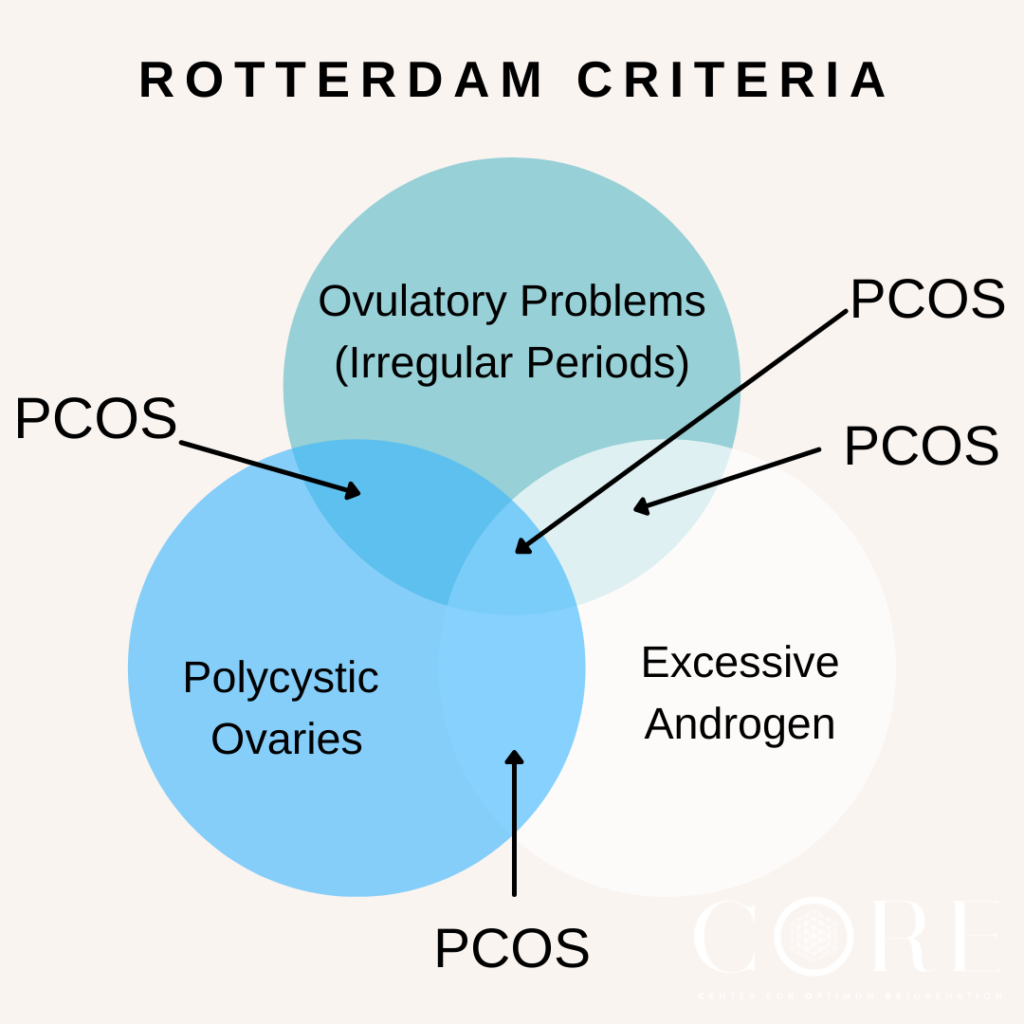
- Irregular or Absent Periods (Oligo- or Anovulation)
Indicating that ovulation occurs infrequently or not at all. - Signs of High Androgen Levels (Hyperandrogenism)
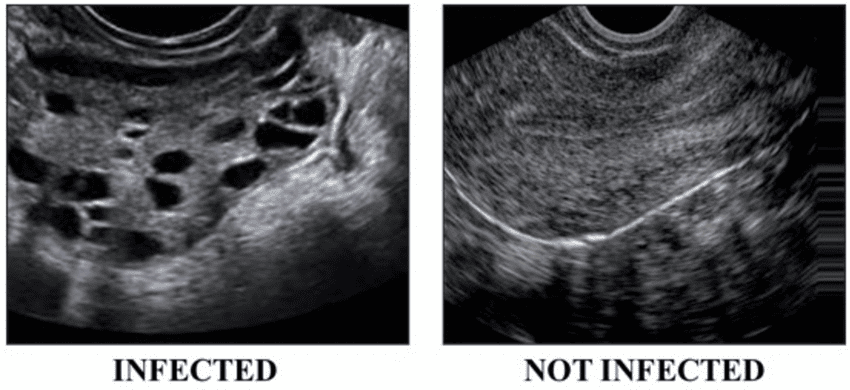
This can be evident through clinical signs (hirsutism, acne, male-pattern baldness) or confirmed via blood tests. - Polycystic Ovaries on Ultrasound
Showing 12 or more small follicles (2–9 mm in diameter) in one or both ovaries, and/or an increased ovarian volume.
2. Essential Diagnostic Tests You May Undergo
To confirm a diagnosis and rule out other conditions that mimic PCOS (such as thyroid dysfunction or adrenal issues), your specialist may recommend a combination of tests:
- Blood Tests
- Hormone Levels: Measure androgens (e.g., total and free testosterone), luteinising hormone (LH), and follicle-stimulating hormone (FSH) to assess reproductive function. A high LH-to-FSH ratio is often observed, although not universally.
- Glucose Tolerance Test (GTT)
This is crucial to assess for insulin resistance or the presence of pre-diabetes or Type 2 diabetes, which commonly co-exist with PCOS. - Pelvic Ultrasound
An imaging test to visually examine the ovaries. As mentioned, many cases show a characteristic “string of pearls” appearance—the hallmark of many small, underdeveloped follicles .
Explore how PCOS affects fertility, treatment options, and the practical steps you can take to improve your chances of conception in this article: Can PCOS Cause Infertility? What You Need to Know.
Treatment Your Gynecologist May Recommend
Effective PCOS treatment is always individualised. It is essential to remember that treatment should meet you where you are, addressing your most bothersome symptoms and primary health goals.
The majority of patients tend to fall into three main groups, and treatment plans are crafted accordingly:
- Patients trying to conceive.
- Patients with bothersome symptoms (e.g., severe acne, hirsutism, irregular periods).
- Patients who are asymptomatic but newly diagnosed (focused on preventing long-term risks).
1. Foundational Treatment: Lifestyle Changes
For women with PCOS, lifestyle changes are the first-line and most effective treatment. These steps address the underlying factor of insulin resistance and often lead to significant improvements in hormonal balance and symptom severity.
- Dietary Adjustments: Focus on a low-glycaemic index (GI) diet to manage insulin levels. This includes consuming complex carbohydrates (whole grains), healthy fats, and lean proteins, while minimising processed sugars and highly refined foods.
- Regular Exercise: Consistent physical activity significantly improves insulin sensitivity, making your body more effective at regulating blood sugar. Even a 30-minute brisk walk most days of the week can be beneficial.
- Weight Management: Losing even a small percentage of body weight (5-10%) can often be enough to restore regular ovulation and ease symptoms like excess hair growth and acne.
2. Medication for Symptom Management
Medication is typically used to manage the specific symptoms that lifestyle changes cannot control alone.
- Oral Contraceptive Pills (OCPs) / Hormonal Birth Control: OCPs are the most commonly prescribed medication for PCOS when pregnancy is not desired. They provide a regular dose of hormones (oestrogen and progestin) that:
- Regulate the Menstrual Cycle
Ensuring regular, predictable periods, which helps to prevent the build-up of the uterine lining (endometrium), reducing the risk of endometrial cancer. - Decrease Androgen Levels
By raising levels of a protein called Sex Hormone Binding Globulin (SHBG), OCPs help bind up excess free testosterone, leading to an improvement in acne and hirsutism over time.
- Regulate the Menstrual Cycle
| Addressing the Concern on Long-Term Use: Some patients worry about the safety of long-term hormonal birth control use. Our specialists advise that for many women with PCOS, this medication is medically necessarynot just for contraception or symptom relief, but to protect the endometrium. By ensuring a monthly "withdrawal bleed," OCPs mitigate the serious long-term risk of endometrial hyperplasia and cancer associated with chronic, unopposed oestrogen stimulation due to lack of ovulation. The risks and benefits are always carefully weighed by your gynecologist. (For more information on contraceptive methods, please refer to our Obstetrics and Gynaecology specialists). |
- Insulin Sensitisers (e.g., Metformin)
These medications are commonly used to treat Type 2 diabetes but are highly effective in managing PCOS-related insulin resistance. By helping the body use insulin more effectively, they can lower blood sugar, reduce androgen production, and, for some women, help restore ovulation. - Anti-Androgen Medications
Drugs like spironolactone can block the effects of androgens on the skin and hair follicles, providing relief for severe hirsutism and acne. These are often used in conjunction with OCPs.
3. Fertility Treatment If Trying to Conceive
PCOS is one of the most common treatable causes of infertility. The good news is that many women with PCOS can achieve a successful pregnancy with guidance.
- Ovulation Induction
The goal is to stimulate the ovaries to release an egg. Common first-line treatments include oral medications like Clomiphene Citrate or Letrozole. These drugs are monitored by your specialist through ultrasound to time intercourse or intrauterine insemination (IUI). - In Vitro Fertilisation (IVF)
For patients who do not respond to ovulation induction or have other compounding fertility factors, IVF remains a highly effective option, allowing the specialist to carefully control the hormonal environment.
| You can learn more about advanced options here: IUI vs IVF: Which Fertility Treatment is Right for You?). |
4. Surgery
While lifestyle and medication cover the vast majority of cases, a surgical procedure known as Laparoscopic Ovarian Drilling (LOD) may be considered for a select group of women with PCOS who are resistant to standard oral fertility medications.
LOD involves using a fine electrical current or laser to puncture the surface of the ovary. This process can temporarily lower androgen levels and restore ovulation for a period, potentially allowing conception to occur naturally or with less intensive fertility drug support. LOD is a specialised, minimally invasive option and is not a first-line treatment.
Living with PCOS: Mental Health Management
Dealing with chronic symptoms like weight struggles, unwanted hair growth, acne, and the stress of fertility issues can significantly impact a woman’s mental well-being. At Island Hospital, we recognise the importance of treating the whole person.
- Depression and Anxiety
Studies have shown that women with PCOS have a higher prevalence of depression and anxiety compared to the general population. The fluctuations in hormone levels, combined with the visible, often embarrassing symptoms, contribute to lower self-esteem and body image issues. Open communication with your doctor about your emotional state is vital. - PCOS Affects Libido
Hormone imbalances, specifically the higher levels of androgens, can affect libido. Furthermore, the emotional distress and physical discomfort associated with PCOS can also lower sexual desire. Addressing the root hormonal and metabolic issues often leads to an improvement in quality of life, including sexual health.
Managing PCOS effectively involves a holistic team approach, often including mental health counselling alongside your gynaecological and dietary treatment.
Achieve Your Personal & Reproductive Goals with Island Hospital
The future with PCOS is defined by management, not limitation.
With the specialised care and cutting-edge resources available at Island Hospital, we empower you to effectively manage your symptoms, aggressively mitigate long-term health risks (including diabetes and endometrial cancer), and turn your reproductive aspirations into reality.
We are here to be your partner in health, providing the expert, compassionate care that so many patients have experienced: (Read our patient success stories here: Island Hospital Facebook Testimonials).
Stop surviving PCOS, and start thriving. Let us be your guide.
Contact us today to schedule your comprehensive consultation.
FAQ
How does a gynecologist diagnose PCOS?
A gynecologist diagnoses PCOS using the Rotterdam Criteria, requiring at least two out of three findings: irregular or absent periods, signs of high androgen levels (blood tests or clinical symptoms like hirsutism), and/or polycystic ovaries visible on a pelvic ultrasound.
This is an exclusionary diagnosis, meaning other conditions with similar symptoms (like thyroid issues or high prolactin) must first be ruled out.
How does PCOS affect fertility?
PCOS is a leading cause of female infertility because the hormonal imbalance (excess androgens and insulin) prevents the ovaries from releasing an egg—a process called anovulation. If an egg is not released, conception cannot occur.
Treatment focuses on restoring regular ovulation through lifestyle changes, insulin-sensitising medications, or specific ovulation-inducing drugs.
Does PCOS cause more serious issues like cancer?
While PCOS itself is not cancer, it is associated with an increased long-term risk of endometrial cancer (cancer of the uterine lining). This risk occurs because the lack of regular ovulation means the uterine lining builds up without being shed.
If the lining is not shed regularly (at least every three months), prolonged exposure to oestrogen can cause abnormal cell growth. This risk is managed effectively through medications like hormonal birth control or periodic progestin therapy to ensure the lining is shed. PCOS also increases the risk of metabolic conditions like Type 2 diabetes and heart disease.