
07 Jul Oesophagectomy Surgery: Patient’s Guide to Before, During & After
Oesophagectomy Surgery: Patient’s Guide to Before, During & After
By Island Hospital | July 07, 2025 10:30:00 AM
An oesophagectomy is a major surgical procedure to remove all or parts of your oesophagus, which is the tube that connects your throat to your stomach.
In this article, you’ll find information to help you through the entire process: how to prepare for your surgery, what happens during the procedure, and what to expect during recovery.
We hope this guide eases any anxiety you’re feeling and answers questions you’ve been having. As every experience is different, get in touch with our specialists for more details.
Overview of Your Oesophagectomy Surgery
An oesophagectomy is usually done to treat or relieve symptoms of oesophageal cancer. It’s also done to treat conditions that increase your cancer risk and benign (noncancerous) conditions which cause your oesophagus to not work as it should.
During the procedure, your surgeon will remove the damaged and diseased parts of your oesophagus. Then, they’ll pull up your stomach or small intestine and reattach it to your remaining oesophagus. We’ll cover more on this in the next section.
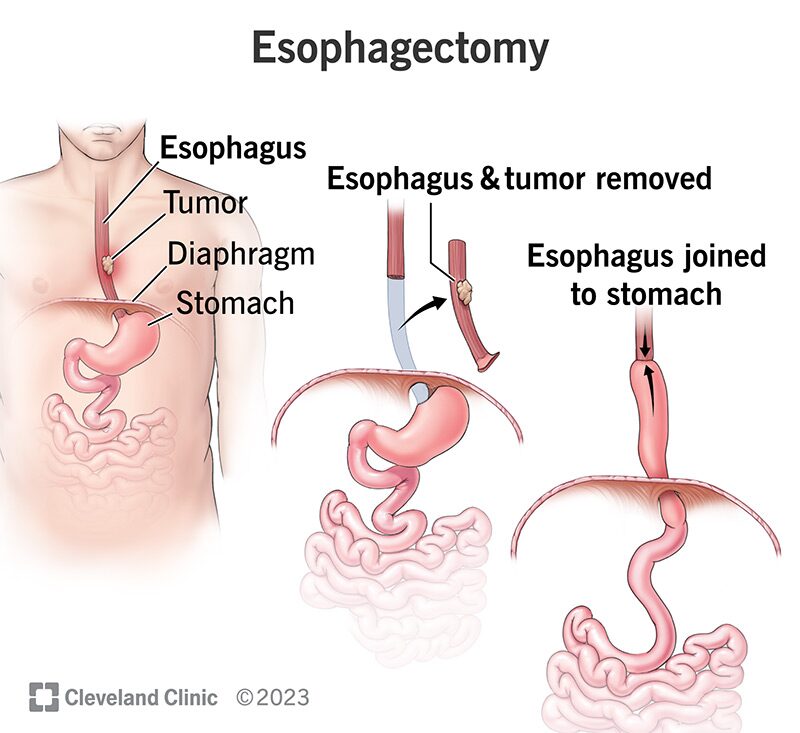
Source: Cleveland Clinic
Before Surgery: The Weeks Leading Up
Diagnostic Tests and Pre Admission Visits
Before your surgery, your doctor may run the following tests:
- Blood tests
- A swab test
- An ECG
- Breathing tests
- An echocardiogram
- A chest x-ray
- A cardiopulmonary exercise test
You’ll also have a pre-admission visit to prepare for your stay. During this appointment, we’ll:
- Review your general health and medical history
- Go over your current medications
- Explain our hospital’s recovery programme and what to expect
Diet, Lifestyle, and Medication
Your care team may recommend specific dietary changes and lifestyle modifications in the weeks before surgery.
This might include eating smaller, more frequent meals to help your body adjust, avoiding certain foods that may cause discomfort, and ensuring you’re getting proper nutrition to support healing.
You may also need to stop certain medications or supplements as directed by your doctor. If you smoke, quitting before surgery is strongly recommended as it significantly improves healing and reduces complications.
Gentle exercise, as approved by your medical team, can help strengthen your body for the recovery ahead.
What Should I Bring For My Hospital Stay?
Your care team will recommend the following items:
-
- Your medicines
- Personal hygiene items (e.g., brush, toothbrush, toothpaste, soap, towel)
- Eyeglasses, contact lenses, solution
- Loose fitting, comfortable clothes
- Smartphone and tablet with their chargers
- Comfort items (e.g., books, headphones, playing cards)
- A copy of your advanced medical directive
- A copy of your most recent clinic letter (if you have one)
Who Will Be on My Care Team?
Here’s who will be on your care team:
- The surgeon will perform your operation and oversee your surgical care.
- The clinical nurse specialist (CNS) will coordinate your care and provide specialised support throughout your journey.
- The dietitian will help you manage your diet and nutrition needs before and after surgery.
- The anaesthetist will manage your anesthesia during surgery and pain control afterward.
- Nurse or health care assistant will provide daily care and monitor your progress.
- The physiotherapist will help you regain strength and mobility during recovery.
Building Your Support System
Having a strong support network is essential for your recovery. Consider asking family members or close friends to help you during your hospital stay and recovery at home.
This might include someone to stay with you, help with daily tasks, attend appointments, or simply provide emotional support. Many patients find it helpful to designate one person as a primary contact who can communicate updates to other family and friends.
Don’t hesitate to reach out to support groups or counseling services if you need additional emotional support during this time.
During Surgery: The Day of Your Procedure
An esophagectomy usually takes around 3 to 6 hours. Before surgery, you’ll be given anaesthesia which will put you to sleep so you don’t experience any pain.
- Depending on the type of oesophagectomy, your surgeon will make small cuts into your neck, chest, abdomen, or a combination to access your oesophagus.
- Then, your surgeon will remove the diseased or damaged part of your oesophagus.
- Your surgeon will pull up your stomach or small intestine up into your chest or neck area and reconnect it to the remaining oesophagus.
- In some cases, the stomach may be reshaped into a tube to help with digestion.
- A feeding tube (jejunostomy tube) may be placed into your small intestine to provide nutrition while you recover.
- The incisions will be closed with stitches or staples and covered with dressings.
- You’ll be moved to the recovery room, where your vital signs will be closely monitored as you wake up from anaesthesia.
After Surgery: The Road to Recovery
Recovery from an esophagectomy is a gradual process that requires patience and commitment. Initially, you’ll spend time in the intensive care unit where your medical team will closely monitor your vital signs and ensure you’re healing properly.
As you progress, you’ll move to a regular hospital room where you’ll begin the process of relearning how to eat and drink. Your care team will guide you through each step, from taking small sips of water to eventually eating solid foods again.
How long is the recovery after an oesophagectomy?
It may take 1 or 2 years to adjust to life after the surgery. However, everyone is different. Your condition prior to the surgery affects this recovery period.
Potential Complications
When to Seek Help
Call your care team if you experience:
- Worsening pain or fevers
- Warmth or redness around the incisions
- Weakness
- Shortness of breath
- Heart racing
- Diarrhea or black stools
- Burning in your throat
- Persistent cough
- Jaundice
- Trouble swallowing
- Uncontrollable weight loss
Get immediate medical attention if you:
- Have trouble swallowing or breathing
- Vomit blood
- Have severe pain (including chest pain)
Book an Appointment With Island Hospital Today
At Island Hospital, our oncologists, experienced nurses, and dedicated paramedical support are ready to guide you throughout your esophagectomy surgery.
From precise diagnostic testing to advanced treatments to compassionate support services, our Clinical Oncology and Haemato-Oncology Centre is fully-equipped to help you fight back against cancer.
Moreover, our Gastroenterology Centre provides comprehensive high-end care for a wide range of gastrointestinal disorders. We aim to provide the best treatment and care for your digestive system.
Schedule an appointment with our specialists today. Should you have any enquiries on the treatment, services, or facilities at Island Hospital, feel free to contact us.
FAQ
What is the bowel prep before esophagectomy?
Bowel preparation before esophagectomy usually involves dietary restrictions and the use of laxatives to clear the intestines. This reduces the risk of infection and complications if part of the colon is used to reconstruct the esophagus.
What is the most common cause of death after esophagectomy?
The most common cause of death after esophagectomy is respiratory complications, such as pneumonia or acute respiratory distress syndrome (ARDS). These issues often result from surgical stress, anesthesia, or pre-existing lung conditions.
What is a preoperative esophagectomy risk score?
A preoperative esophagectomy risk score is a clinical tool used to estimate a patient’s risk of complications or mortality after surgery. It considers factors like age, nutrition, lung function, and comorbidities to guide surgical planning and patient counseling.
What is the quality of life after esophagectomy?
Quality of life after esophagectomy often improves over time but may be affected by changes in eating habits, digestive issues, and fatigue. Most patients adapt well, especially with support from dietitians and rehabilitation programs.
However, it’s important to note that everyone’s experiences are different. Talk to your doctor about any concerns and questions.
What are the digestive problems after esophagectomy?
Common digestive problems after esophagectomy include difficulty swallowing, acid reflux, dumping syndrome, and early satiety. These issues arise due to changes in anatomy and can often be managed with diet modifications and medication.






