
27 Dec
Liver Disease Warning Signs You Should Never Ignore
By Island Hospital | Dec 27, 2018 12:04:20 PM
The liver is a vital organ, roughly the size of a football, located beneath the rib cage on the right side of the abdomen. It plays a crucial role in digestion, metabolism, and detoxification—helping the body process nutrients, filter harmful substances, and maintain overall health.
Liver disease occurs when the liver becomes damaged or inflamed. It may be inherited (genetic) or develop due to factors such as viral infections, excessive alcohol consumption, obesity, or long-term metabolic conditions.
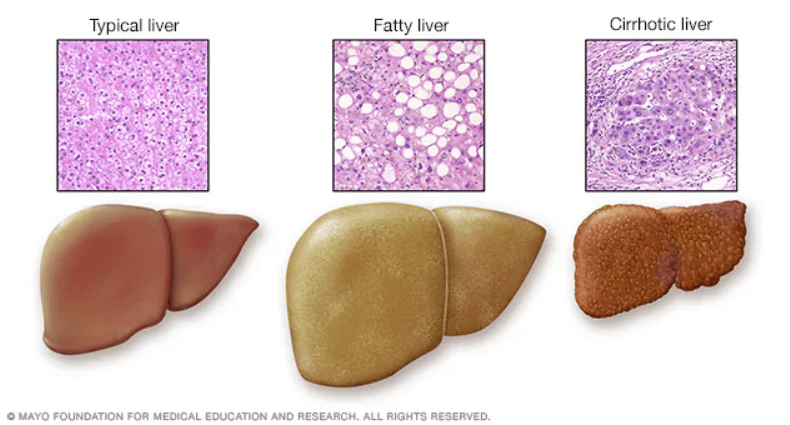
Over time, ongoing liver damage can lead to scarring known as cirrhosis. In advanced stages, this scarring interferes with normal liver function and may progress to liver failure, a serious and potentially life-threatening condition.
Symptoms and Signs
Liver disease may not cause noticeable symptoms in its early stages, which is why it often goes undetected.
As liver function becomes impaired, a range of symptoms and physical signs may begin to appear, indicating the need for medical evaluation.
Symptoms
- Chronic fatigue
- Nausea
- Vomiting
- Loss of appetite
- Tendency to bruise easily
Signs
- Skin and eyes that appear yellowish (Jaundice)
- Abdominal pain and swelling
- Swelling in the legs and ankles
- Itchy skin
- Dark urine colour
- Pale stool colour/ bloody or tar-coloured stool
Diagnosis
As liver disease may not cause obvious symptoms at first, diagnostic testing plays a key role in identifying the condition early.
To ensure an accurate diagnosis, your doctor will use a combination of clinical assessment and diagnostic tests to evaluate liver function and determine the underlying cause:
- Blood tests
A group of blood tests called liver function tests can be used to diagnose liver disease. Additional blood tests may be performed to identify specific liver conditions, infections, or inherited (genetic) disorders.
- Imaging tests
Imaging studies such as ultrasound, CT scans, and MRI scans allow doctors to evaluate the size, shape, and structure of the liver. These tests can help detect abnormalities, scarring, or tumours within the liver.
- Tissue analysis
Removing a tissue sample (biopsy) from your liver may help diagnose liver disease and look for signs of liver damage. A liver biopsy is most often done using a long needle inserted through the liver. It is then analysed in a laboratory.
______________________________________________________
Reduce your risk of liver cancer. Understand and adopt these simple steps for a healthy liver and better you.
______________________________________________________
Treatment
Treatment for liver disease is tailored to each individual, as different liver conditions require different approaches.
With appropriate medical care, many patients can manage their condition effectively through lifestyle changes, medications, procedures, or surgery, with the aim of slowing disease progression, relieving symptoms, and preventing further liver injury.
- Condition-specific care
Each type of liver disease has its own treatment approach. For example, hepatitis A is usually managed with supportive care while the body’s immune system clears the infection.
- Surgical treatment
Patients with gallstones or gallbladder-related complications may require surgery to remove the gallbladder.
- Management of cirrhosis and advanced liver disease
In patients with cirrhosis or end-stage liver disease, medications may be needed to treat complications such as fluid accumulation (ascites), bleeding, and hepatic encephalopathy.
- Dietary changes and medications
A low-sodium diet and water tablets (diuretics) are often prescribed to reduce fluid retention and swelling.
- Treatment of ascites
For patients with significant fluid buildup in the abdomen, a procedure called paracentesis may be performed to remove excess fluid using a needle under local anaesthetic. This procedure can also help detect infection in the ascitic fluid.
- Treatment of portal hypertension
Certain procedures or surgeries may be required to manage portal hypertension, along with medications to reduce the risk of internal bleeding.
- Liver transplantation
Liver transplantation may be considered for patients with advanced or terminal liver failure when other treatments are no longer effective.
- Long-term disease management
Some liver conditions require ongoing medical care and regular monitoring to control symptoms and minimise long-term complications.
Prevention
Protecting your liver starts with everyday habits and informed health decisions. Check out these simple preventive measures that can help you reduce your risk of liver disease and support long-term liver function:
- Drink alcohol in moderation
For healthy adults, that means up to one unit a day for women and up to two drinks a day for men. Heavy or high-risk drinking is defined as more than eight drinks a week for women and more than fifteen drinks a week for men.
- Avoid risky behavior
Get help if you use illicit intravenous drugs, and don’t share needles used to inject drugs. Use a condom during sex. If you choose to have tattoos or body piercings, be picky about cleanliness and safety when selecting a shop.
- Get vaccinated
If you’re at increased risk of contracting hepatitis or if you’ve already been infected with any form of the hepatitis virus, talk to your doctor about getting the hepatitis A and hepatitis B vaccines.
- Use medications wisely
Take prescription and non-prescription drugs only when needed and only in recommended doses. Don’t mix medications and alcohol. Talk to your doctor before mixing herbal supplements or prescription or non-prescription drugs.
- Avoid contact with other people’s blood and body fluids
Hepatitis viruses can be spread by accidental needle sticks or improper cleanup of blood or body fluids. The risk of contracting hepatitis B and C can be decreased by minimising the risk of exposure to another person’s bodily fluids.
- Take care with aerosol sprays
Make sure the room is ventilated, and wear a mask when spraying insecticides, fungicides, paint and other toxic chemicals. Always follow the manufacturer’s instructions.
- Protect your skin
When using insecticides and other toxic chemicals, wear gloves, long sleeves, a hat and a mask.
- Maintain a healthy weight
Obesity can cause non-alcoholic fatty liver disease.
Risks If Left Untreated
Just as cracks in a building worsen if left unrepaired, small liver problems can escalate into serious disease without proper treatment.
Therefore, early care and attention can help prevent small issues from turning into serious, irreversible damage.
- Inflammation
This inflammation can cause damage to the liver, making the condition worse. In this beginning stage, unlike some conditions in advanced liver disease, the symptoms and inflammation is treatable to prevent the second step of the disease.
- Fatty Liver
When a fatty liver is left untreated, it develops into Steatohepatitis, (a condition where not only fat is accumulated in the liver) but there is inflammation (hepatitis) and liver cell death (necrosis) and scarring (fibrosis) occur.
- Liver Disease
Fibrosis of the liver can then progress to cirrhosis of the liver, which is the last stage of Liver Disease.
________________________________________________________________________
With tens of thousands of cases of Hepatitis B and C in Malaysia, early detection and vaccination are key. Learn how early screening, timely treatment, and vaccination can safeguard your liver in 3 Most Common Hepatitis.
______________________________________________________________________
Your Road to A Healthier Liver Starts Today
With the right guidance, your journey to a healthier liver starts today by managing your symptoms and maintaining a healthy habit quality of life.
Every patient’s liver health, lifestyle, and goals are unique. That’s why the most effective care comes from a personalised plan designed around you, guided by experienced liver specialists who understand both the science and the human side of this journey.
Here’s how you can take proactive steps today:
- Ask, learn, and share: Bring your test results, medical history, and any questions to your doctor.
- Explore your options: Liver disease management can involve lifestyle changes, medications, procedures, or surgery. Your specialist will help you find the right approach for your specific situation.
- Plan for the future: Talk with Island Hospital’s Gastroenterology experts about monitoring, diet, lifestyle adjustments, and support systems so you can stay on top of your liver health over the long term.
Book a consultation with a liver specialist today to start a personalised care plan tailored to you and your health goals.
FAQs
1. What’s the most likely cause of my symptoms?
It’s important to understand what may be contributing to your liver issues. Causes can range from viral infections and fatty liver to medication side effects or inherited conditions.
Therefore, asking this helps you and your doctor focus on the most relevant tests and treatments.
2. What kinds of tests do I need? Do these tests require any special preparation?
Liver problems are usually evaluated with blood tests, imaging studies, and sometimes a liver biopsy. Remember to ask your doctor about each test, how it is performed, whether fasting or other preparation is needed, and what the results can reveal.
3.Should I stop taking certain medications or supplements?
Some medications and herbal supplements can worsen liver problems or interact with treatments. Be sure to make a list of everything you take and discuss them with your doctor on whether any should be paused, adjusted, or replaced with safer alternatives.
4. Should I avoid alcohol?
Alcohol can damage the liver and worsen many liver conditions. Ask your doctor whether complete abstinence is necessary or if moderate use is safe in your specific case.
5. I have other health conditions. How can I best manage these conditions together?
Conditions such as diabetes, high blood pressure, or obesity can affect liver health. Discuss how to manage all your health issues together, including medications, diet, and lifestyle adjustments, to ensure your liver stays protected.







