07 Jan How Weight Loss Helps Improve Type 2 Diabetes?
How Weight Loss Helps Improve Type 2 Diabetes?
By Island Hospital | Jan 7, 2026 12:00:00 PM
Living with diabetes can be intimidating, especially if you’ve been recently diagnosed with type 2 diabetes. Many people imagine a future filled with strict diets, endless rules, and a constant fear of their blood sugar spiralling out of control. But the truth is far more empowering.
Type 2 diabetes can be effectively managed and, in many cases, significantly improved with the right lifestyle choices. Among all the tools available, weight management stands out as one of the most powerful.
Weight loss is not just about appearance or feeling better — it can transform your health from the inside out. Even shedding a small amount of weight can create profound, positive changes in your body: improving the way you use insulin, boosting energy levels, and reducing the risk of long-term complications.
In this article, we’ll explore why weight loss matters for people living with type 2 diabetes, how it supports better blood sugar control, and the practical steps you can take to achieve it safely and sustainably.
What is Diabetes?
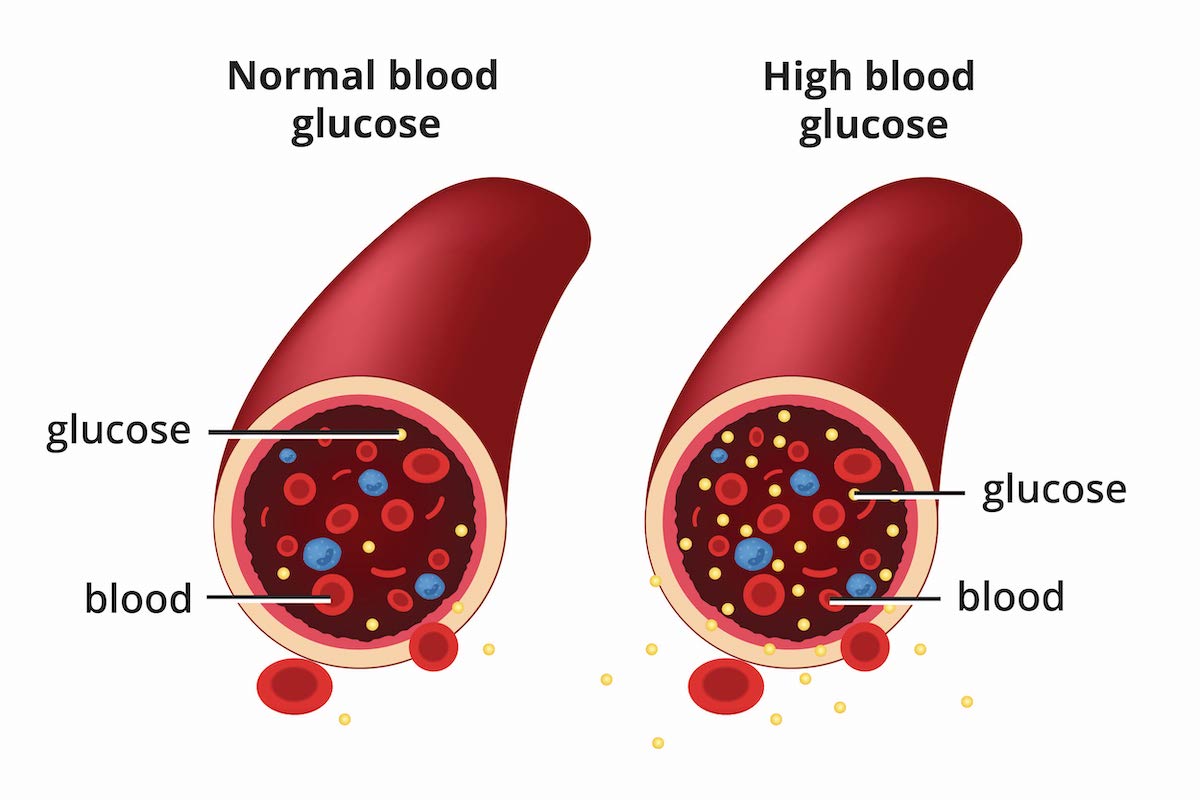
Diabetes is a chronic condition in which the body struggles to regulate blood sugar (glucose) due to problems with the hormone insulin. Insulin acts like a key that allows glucose from the bloodstream into our cells, where it’s used for energy.
Type 2 Diabetes
- The body still produces insulin, but cells become resistant, or the pancreas doesn’t make enough.
- It develops gradually and is strongly linked to excess weight, inactivity, and genetics.
- Treatment includes lifestyle changes, weight loss, medications, and sometimes insulin.
- Weight loss is especially effective because it reduces insulin resistance and improves blood sugar control.
Why Weight Loss Helps in Type 2 Diabetes?
In Type 2 diabetes, carrying excess body fat (particularly around the abdomen) worsens insulin resistance. When the body becomes more efficient at using insulin, blood sugar levels improve. Simply put:
- Losing weight reduces fat buildup in the liver and muscles, helping insulin work more efficiently.
- Improved insulin sensitivity allows glucose to enter cells more effectively, lowering high blood sugar levels.
- Even modest weight loss (around 5% of body weight) can significantly improve blood sugar control and may reduce the need for medication.
- While weight loss isn’t a cure, it is one of the most powerful tools for managing and improving Type 2 diabetes outcomes.
Worried about how diabetes might affect your vision? This article on diabetic retinopathy treatment explains what you need to know — causes, symptoms, and the care options available to protect your eyesight.
What Are the Benefits of Weight Loss for Type 2 Diabetes?

Weight loss is one of the most effective ways to improve diabetes control — and the benefits begin even with modest changes. Research shows that losing just 5% of your starting weight can lead to measurable improvements in blood sugar, heart health, and overall well-being.
Here’s how weight loss makes a meaningful difference for people living with type 2 diabetes:
1. Decreases Insulin Resistance
Excess body fat, especially around the abdomen, makes it harder for the body to use insulin properly — a condition known as insulin resistance.
When you lose weight, your body becomes more sensitive to insulin, allowing glucose to enter cells more efficiently. This helps stabilise blood sugar levels throughout the day.
2. Helps Improve Blood Sugar Levels
As insulin sensitivity improves, your blood sugar naturally becomes easier to manage. Some individuals may even experience a return to near-normal blood sugar levels with consistent lifestyle changes, sometimes reducing the need for multiple medications.
3. Boosts Energy Levels
High blood sugar often leaves people feeling sluggish or fatigued. Weight loss helps your body use glucose more effectively, leading to better energy levels, improved focus, and a general sense of vitality.
4. Supports Better Sleep
Many people with type 2 diabetes also struggle with sleep issues such as sleep apnoea. Losing weight can reduce airway pressure, helping you breathe more easily at night, resulting in deeper, more restorative sleep.
5. Improves Mobility
Even a few kilograms of weight loss can reduce pressure on your joints, making it easier to walk, climb stairs, and stay physically active. Improved mobility also makes exercise more enjoyable and sustainable.
6. Promotes a Healthier Heart
Type 2 diabetes is closely linked to heart disease, but weight loss can reduce several key risk factors, including:
- Total cholesterol
- Triglycerides
- LDL (“bad”) cholesterol
- Blood pressure
These improvements collectively lower your risk of heart attacks, stroke, and other cardiovascular complications.
7. May Reduce the Need for Diabetes Medications
As blood sugar stabilises and insulin sensitivity improves, many individuals can reduce, and sometimes discontinue, certain diabetes medications under medical supervision. Modern weight-friendly diabetes medications can further support this progress.
What Is a Healthy Weight?
When it comes to managing Type 2 diabetes, the goal isn’t to reach a “perfect” weight — it’s to achieve a healthier weight that improves your blood sugar, energy levels, and overall health.
A healthy weight looks different for everyone. It depends on factors such as age, body composition, genetics, and where you store fat. Instead of focusing on an ideal number on the scale, healthcare professionals look at trends and overall metabolic health.
BMI as a General Guide
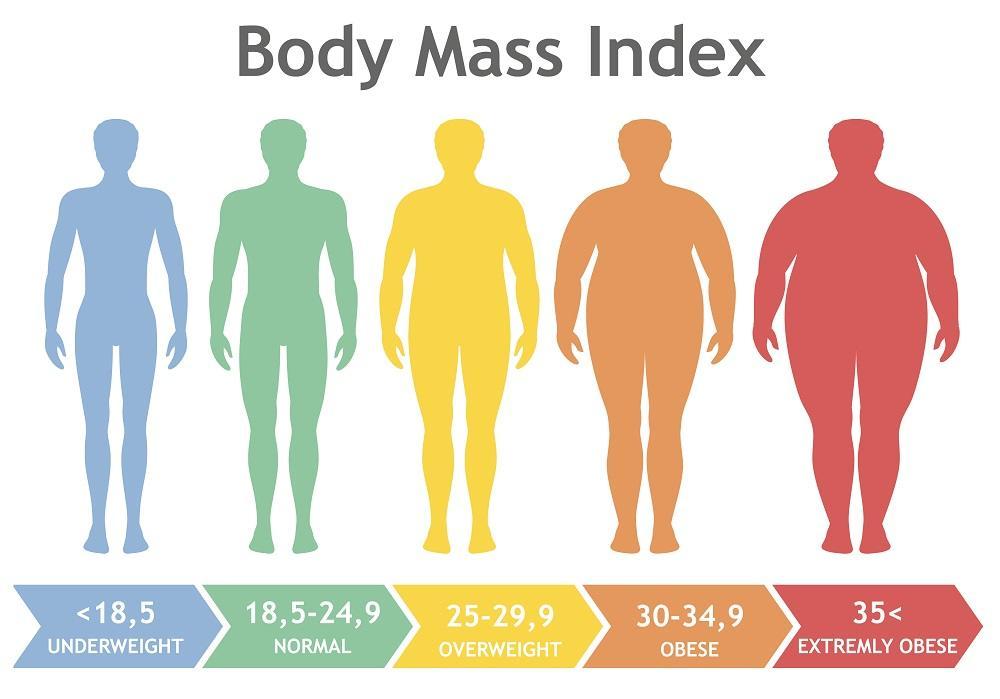
Body Mass Index (BMI) is commonly used to estimate a healthy weight range:
- Under 18.5: Underweight
- 18.5–24.9: Healthy weight
- 25–29.9: Overweight
- 30+: Obesity
BMI isn’t perfect, but it offers a starting point for understanding where your weight sits in relation to health risk.
What Should You Aim For?
For people with Type 2 diabetes, research consistently shows that losing even 5% of your current body weight can:
- Improve blood sugar control
- Reduce insulin resistance
- Lower blood pressure and cholesterol
- Reduce the need for some medications
Aiming for 5–10% weight loss is realistic, safe, and backed by substantial evidence. For example, if you weigh 90 kg, aim to lose 4.5-9 kg.
This percentage-based approach is far more achievable and far more beneficial than trying to reach a specific “ideal” weight all at once.
How to Lose Weight Safely with Type 2 Diabetes

While weight loss can make a big difference in diabetes management, it doesn’t mean going on extreme diets, skipping meals, or pushing your body through exhausting workouts. These habits usually do more harm than good, triggering blood sugar fluctuations and leaving you drained.
A healthier approach is to focus on balanced meals, regular movement, and small, sustainable habits that support long-term success.
1. Build a Diabetes-Friendly Eating Plan

A healthy eating plan for diabetes focuses on foods that stabilise blood sugar, support steady energy, and help reduce overall calorie intake.
Choose nutrient-rich, high-fibre foods
Fibre-rich, nutrient-dense foods help slow digestion, preventing sharp spikes in blood sugar, and keep you full for longer, making it easier to manage your appetite and reduce calories.
They’re also packed with essential vitamins, minerals, and antioxidants without adding excess calories — the perfect combination for healthy, sustainable weight loss.
Aim for at least half your plate to be vegetables, especially non-starchy varieties. Great options include:
- Vegetables (especially non-starchy varieties: leafy greens, broccoli, cucumber)
- Whole fruits (berries, apples, citrus)
- Whole grains (brown rice, wholemeal bread, quinoa)
- Legumes (beans, chickpeas, lentils)
- Nuts and seeds
Focus on lean protein
Lean protein helps keep you full and satisfied, reducing cravings and preventing overeating. Protein also has little impact on blood sugar, making it a key part of balanced, diabetes-friendly meals. Aim for ¼ of your plate to be lean protein, such as:
- Fish
- Skinless poultry
- Tofu
- Eggs
Choose healthy fats
Healthy fats support better insulin sensitivity and promote heart health—an important benefit for people with diabetes. They also add richness to meals, helping you feel satisfied with smaller portions. Good sources include:
- Olive oil
- Avocado
- Nuts
- Seeds
Choose Smart Carbohydrates
Carbohydrates affect blood sugar the most, so choosing the right types and the right portions is key. Aim for ¼ of your plate to come from whole grains or healthy starchy vegetables, which provide fibre and more stable energy than refined carbs.
- Brown rice
- Wholemeal bread
- Quinoa
- Sweet potatoes
- Oats
Foods to limit
On the other hand, it’s best to limit foods that cause rapid blood sugar spikes, increase calorie intake, and make weight loss more difficult. These include:
- Sugary drinks
- Refined carbs such as white bread, pastries, and sugary cereals
- Deep-fried foods and items high in saturated or trans fats
2. Eat Regularly — Don’t Skip Meals
People with diabetes should avoid skipping meals because it can cause:
- Low blood sugar (hypoglycaemia)
- Intense hunger that leads to overeating later
- Sluggish energy and cravings
Aim for 3 balanced meals, around the same time each day. Some people benefit from 1–2 healthy snacks, especially if their medications can cause low blood sugar.
3. Start with Achievable Physical Activity
Exercise plays a powerful role in improving insulin sensitivity, burning calories, and supporting weight loss, but you don’t need to jump into intense workouts to see results.
Recommended (CDC):
- 150 minutes of moderate activity per week, such as brisk walking, cycling, light jogging, and swimming
- Strength training 2 or more days per week helps build muscle, which boosts metabolism and lowers blood sugar
- Break it up: three 10-minute walks are just as effective as one 30-minute session.
Easy ways to increase daily movement
- Take the stairs instead of the lift
- Park further away
- Walk after meals
- Do light housework or gardening
- Stretch or move during TV commercial breaks
4. Combine Diet + Exercise for the Best Results
Research shows that weight loss is most successful when healthy eating and physical activity are paired together. This combination:
- Burns more calories
- Increases muscle mass
- Reduces insulin resistance
- Helps stabilise blood sugar throughout the day
People who combine both are far more likely to lose weight and keep it off.
5. Take a Gradual, Sustainable Approach
Fad diets promise quick results, but they rarely work long-term. Slow, steady progress is safer and more effective for diabetes.
Aim to lose 0.5–1 kg per week, or about 5–10% of your total body weight over a few months — this alone can dramatically improve blood sugar control.
6. Monitor Progress and Adjust As You Go
Keeping track of your progress helps you understand what’s working well and what may need adjusting. Regular monitoring also keeps you motivated and allows you to make informed changes along the way.
Track:
- Blood sugar readings
- Weight and waist circumference
- Energy levels
- Eating patterns
7. Work with Healthcare Professionals
Professional support can make your weight-loss journey safer, more effective, and easier to navigate, especially when managing diabetes. At Island Hospital, endocrinologists, diabetes educators, and dietitians work together to create personalised plans tailored to your needs.
They can help with:
- Personalised meal plans
- Safe exercise programmes
- Medication adjustments
- Weight-loss strategies
- Ongoing education and blood sugar monitoring
Working closely with your healthcare team ensures that every step you take aligns with your health goals and supports long-term diabetes management.
Ready to take control of your diabetes with expert support? Reach out to Island Hospital today.
Want to understand what a healthy diet for diabetes really looks like? Explore this helpful guide packed with simple tips and smart food choices for better blood sugar control.
Diabetes Medications and Weight Loss
Some diabetes medications can support weight loss in addition to improving blood sugar control. These can be helpful when lifestyle changes alone aren’t enough or when insulin resistance is more severe.
Medications that may promote weight loss include:
1. Metformin
Helps reduce insulin resistance and may lead to modest weight loss.
2. GLP-1 receptor agonists (e.g., semaglutide, liraglutide)
Reduce appetite, slow digestion, and can lead to significant weight loss.
3. SGLT2 inhibitors (e.g., empagliflozin, dapagliflozin)
Help the body remove excess glucose through urine, which may support weight reduction.
4. Orlistat (Xenical®)
Blocks fat absorption from food, leading to modest weight loss.
Medications should always be prescribed and monitored by a healthcare professional, as they must be matched to your medical history, blood sugar levels, and weight-loss goals.
Tips to Lose Weight with Type 2 Diabetes

Losing weight when you have Type 2 diabetes doesn’t need to be complicated — it just needs to be focused, consistent, and tailored to your health situation. The following tips, drawn from trusted sources, will help you build sustainable habits.
1. Set Realistic Goals
Begin with small, achievable targets. Aiming to lose around 5% of your current body weight is a great starting point and can already improve blood sugar levels. Breaking this down into weekly goals, such as 0.5–1 kg per week, keeps the process manageable and helps you stay motivated.
2. Eat consistently throughout the day
Skipping meals can cause blood sugar swings and overeating later on. Regular, balanced meals help stabilise your blood sugar and keep hunger in check.
3. Watch your portions
Even healthy foods can add up. Using smaller plates, measuring portions, and paying attention to hunger cues can help you naturally reduce calorie intake.
4. Stay hydrated
Drinking water regularly helps prevent mistaking thirst for hunger and supports overall metabolism.
5. Prioritise good sleep
Poor sleep affects appetite and cravings, making weight loss more difficult. Aim for 7–9 hours of rest each night.
6. Manage your stress
High stress can increase blood sugar and trigger emotional eating. Simple activities like deep breathing, stretching, or enjoyable hobbies can help.
7. Monitor your progress
Tracking your blood sugar, weight, and how you feel helps you notice patterns and adjust your routine when needed.
8. Seek Support
Share your goals with family or friends who can encourage you, join you for walks, or help you stay accountable. Support makes healthy changes feel less overwhelming.
9. Make Gradual Changes
You don’t have to overhaul your lifestyle overnight. Pick one or two changes at a time—like adding vegetables to meals or walking 10 minutes a day. Building habits slowly helps them stick.
10. Eat Slowly and Mindfully
Rushing through meals can lead to overeating. Slow down, pay attention to flavour and fullness, and give your body time to recognise when it’s satisfied.
Take Charge of Your Diabetes Today!
Living with Type 2 diabetes can be challenging, but with the right support, meaningful progress is within reach.
At Island Hospital, our Diabetes Centre provides comprehensive care for all types of diabetes, supported by an experienced team of endocrinologists. We offer personalised treatment plans, weight-management guidance, comprehensive assessments, and advanced diagnostic tools to help you take charge of your health with confidence.
Whether you’re newly diagnosed or looking to improve your blood sugar and weight, we’re here to help. Book an appointment with Island Hospital’s expert diabetes care team today!
FAQ
Can weight loss actually reverse Type 2 diabetes?
In some people, yes. Significant weight loss, especially around the abdomen, can greatly reduce insulin resistance and ease the demand on the pancreas. For some individuals, this leads to diabetes remission, where blood sugar levels return to a normal range without medication.
However, remission doesn’t happen for everyone, and it doesn’t mean the diabetes is “cured.” Ongoing healthy habits are still needed to maintain good control. Even if remission isn’t achieved, any amount of weight loss still improves blood sugar and reduces complications.
How quickly will I see improvements in my blood sugar after losing weight?
Some people notice changes within a few weeks, especially if they lose just a small amount (around 2–5% of their body weight). Your body becomes more sensitive to insulin quite early in the weight-loss process.
Bigger improvements like reduced medication needs or reaching target HbA1c levels usually become clearer after 3–6 months of consistent lifestyle changes.
Is belly fat more harmful for diabetes than other types of fat?
Yes. Belly fat (also called visceral fat) sits deep around your internal organs and has a strong link to insulin resistance. It releases hormones and inflammatory chemicals that make it harder for your body to use insulin effectively.
That’s why losing even a small amount of belly fat can lead to noticeable improvements in blood sugar control.
Does menopause or ageing make diabetes harder to control?
It can. As we age, we tend to lose muscle mass, gain fat more easily, and become less active — all of which worsen insulin resistance.
For women, menopause adds hormonal shifts that can cause weight gain (especially around the abdomen), higher blood sugar spikes, and fluctuating energy levels.
This doesn’t mean diabetes can’t be controlled — only that adjustments in diet, exercise, and medications may be needed over time.
How often should I check my blood sugar when trying to lose weight?
It depends on your treatment plan, but generally:
- If you’re on medication that can cause low blood sugar (like insulin or sulfonylureas), checking 1–3 times a day may be recommended.
- If you’re not at risk for hypoglycaemia, checking a few times per week or around key moments, such as before and after exercise or when changing your diet, can be enough.
Monitoring helps you understand how food, activity, and weight changes affect your blood sugar, and guides safe adjustments.