
15 Jan How to Prevent Osteoporosis: Your Complete Guide to Stronger Bones
How to Prevent Osteoporosis: Your Complete Guide to Stronger Bones
By Island Hospital | Jan 15, 2026 12:00:00 PM
A fall might seem harmless—just a slip, a bruise, a moment of embarrassment. But for someone with osteoporosis, even a minor fall can lead to a broken bone and months of recovery. In Malaysia, this condition is far more common than many realise.
With 24.1% of the population estimated to be affected and the number of older adults living with osteoporosis expected to rise to 3.3 million by 2050, it has become one of Malaysia’s most silent yet widespread health threats. Men, once thought to be at lower risk, are now showing rising rates as well.
As alarming as these figures sound, osteoporosis is not only manageable—it is often preventable, especially when you start taking action early. Yet many Malaysians remain unaware of the risks, early warning signs, and lifestyle habits that can protect their bones for decades to come.
In this guide, we break down everything you need to know, from what causes osteoporosis to the practical steps you can take to prevent it.
What Is Osteoporosis?
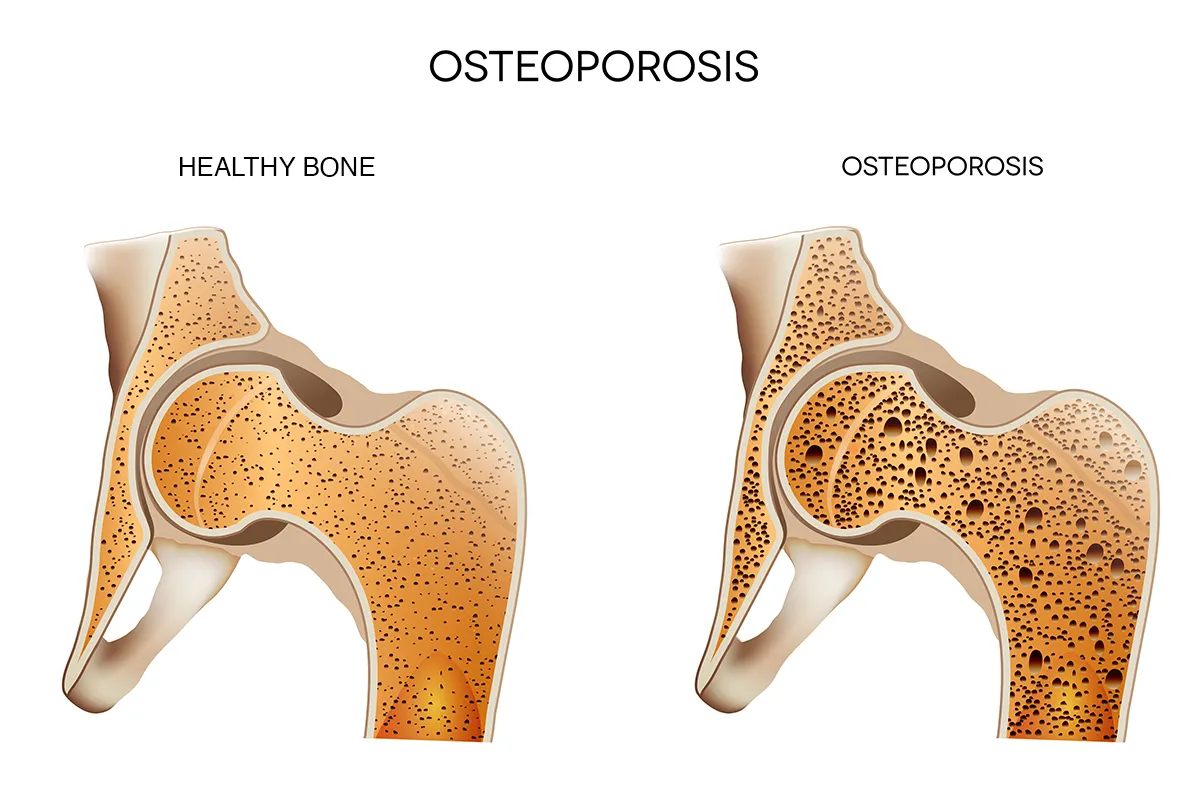
Osteoporosis—literally meaning “bones with holes” is a condition where bones gradually lose their strength, density, and structure. Most people don’t notice this happening because the process is slow and silent. You won’t feel your bones weakening, but over the years, they become more fragile, almost like chalk instead of solid, healthy bone.
At this stage, even simple movements such as bending, lifting, coughing, or a minor fall can cause a fracture. The most common fracture sites are the hip, wrist, and spine. Spinal fractures are especially dangerous because they can occur without a noticeable injury, leading to back pain, loss of height, or a stooped posture.
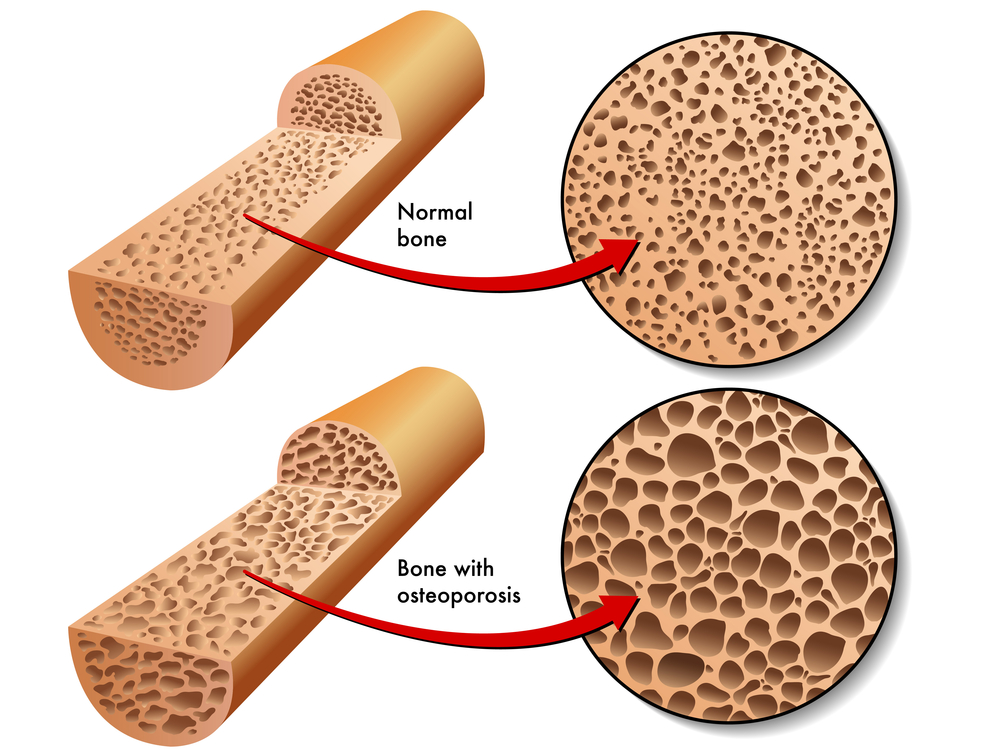
Inside, a healthy bone looks like a tight honeycomb. In osteoporosis, the “walls” of this honeycomb become thinner and weaker, while the spaces between them grow larger. The outer shell of the bone also becomes thinner, making the entire structure more vulnerable.
Bones may look solid, but they are actually living tissue that constantly breaks down and rebuilds. This process happens throughout life:
- In childhood and teenage years – bone is built rapidly
- In your 20s – your body continues strengthening bone
- By your late 20s to early 30s – you reach peak bone mass
- After your 30s – bone breakdown begins to happen faster than bone formation
- After menopause – women experience accelerated bone loss due to hormonal changes
When too much old bone is broken down, and not enough new bone is rebuilt, the bones become porous, brittle, and prone to fracture—this is osteoporosis.
Is hip replacement the answer? Learn what to expect, when it’s recommended, and how to prepare for life after surgery.
Causes of Osteoporosis
Osteoporosis does not develop overnight. It is the result of several long-term factors that gradually weaken bone structure. While some causes are natural, many are closely linked to lifestyle, diet, environment, and hormonal changes.
1. Hormonal Changes
Hormones play a major role in how quickly bones break down.
- Menopause: A sharp drop in estrogen causes rapid bone loss. This is why women over 50 are at the highest risk.
- PCOS (Polycystic Ovary Syndrome): Hormonal imbalance and insulin resistance may affect bone metabolism.
- Thyroid Disorders: Hyperthyroidism, which occurs in many Malaysians, speeds up bone breakdown.
- Low Testosterone in Men: Often underdiagnosed, low testosterone can lead to decreased bone density.
2. Low Calcium Intake
Several studies show that Malaysians generally do not meet the recommended daily calcium intake.
Common reasons include:
- Low consumption of dairy or fortified foods
- Limited intake of leafy greens
- Popularity of processed or low-nutrient meals
- Skipping meals or dieting trends among young adults
Low calcium over long periods significantly weakens bone structure.
3. Vitamin D Deficiency
Despite having year-round sunlight, Malaysia has surprisingly high rates of vitamin D deficiency.
Why this happens:
- Indoor office-based jobs
- Extensive use of sunscreen
- Cultural habits of avoiding sun exposure
- Air-conditioned environments
- Haze season reducing UV penetration
Vitamin D is essential for absorbing calcium. Without it, even if you eat enough calcium, your body cannot use it effectively.
4. Sedentary Lifestyle
Many Malaysians spend long hours sitting, especially in office jobs, during long commutes, or while using phones and screens.
A lack of physical activity reduces:
- Bone-building stimulation
- Muscle strength (which supports bone health)
- Balance (increasing risk of falls)
5. Smoking and Alcohol Consumption
Smoking weakens the cells responsible for forming new bone and reduces the body’s ability to absorb calcium effectively. Excessive alcohol intake further disrupts hormone balance and slows down the bone rebuilding process, making bones more fragile over time.
6. Long-Term Medication Use
Certain medicines increase the risk of osteoporosis, including:
- Steroids (for asthma, arthritis, autoimmune diseases)
- Some thyroid medications
- Certain hormonal treatments
These medications may speed up bone loss if used for long periods.
7. Poor Gut Health
Poor gut health can significantly affect the body’s ability to absorb essential nutrients. Conditions such as:
- Long-term gastric problems
- IBS or inflammatory bowel disease
- Frequent antibiotic use
- Poor diet, high in sugar and processed foods
can impair the digestive system’s ability to properly absorb nutrients. Over time, this contributes to weaker bones and an increased risk of osteoporosis.
8. Being Underweight or Having Low Muscle Mass
Being underweight increases the risk of osteoporosis as the body has less bone mass and fewer nutrient reserves to support healthy bone development. Low muscle mass adds to this risk, as muscles help stimulate bone growth and maintain bone strength.
9. Family History
A family history of osteoporosis or fractures from minor falls can increase your likelihood of developing the condition. This genetic tendency means your bones may naturally be more prone to thinning as you age.
While having a family history doesn’t guarantee osteoporosis, it does make early prevention through diet, exercise, and regular screening even more important.
Wondering what comes next after limb reconstruction? Learn about the key milestones, physical therapy tips, and long-term outcomes.
How to Prevent Osteoporosis
Prevention is the most powerful way to protect your bones—no matter your age. By combining the right nutrients, movement, lifestyle habits, and early detection, you can significantly lower your risk of osteoporosis.
1. Improve Bone-Strengthening Nutrition

Improving your nutrition is one of the simplest and most effective ways to strengthen your bones. The right foods help build bone mass, support bone structure, and improve your body’s ability to maintain healthy bones as you age.
By making sure you get enough calcium, vitamin D, protein, and other essential nutrients, you can significantly reduce your risk of osteoporosis and protect your bones in the long run.
| Nutrient | Why It Matters | Food Sources | Especially Important For |
|---|---|---|---|
| Calcium | Supports bone formation and density | Anchovies, tofu, sardines, leafy greens | Women nearing menopause, older adults |
| Vitamin D | Helps the body absorb calcium | Sunlight, eggs, sardines | Indoor workers, older adults |
| Protein | Builds muscle to support bones | Chicken, fish, tempeh, eggs | Underweight individuals, seniors |
| Magnesium | Helps regulate calcium absorption | Nuts, seeds, whole grains | Those with digestive issues |
| Vitamin K2 | Directs calcium to bones | Tempeh, natto, eggs | Older adults |
| Collagen | Supports bone matrix strength | Bone broth, fish skin | People with low protein intake |
2. Exercise and Movement
Although exercise cannot reverse established osteoporosis, staying active is essential for maintaining bone health. Regular movement helps stimulate bone growth and maintain muscle strength, both of which improve balance and lower the risk of fractures.
Helpful exercise recommendations include:
- Choose weight-bearing activities such as brisk walking, jogging, dancing, badminton, or climbing stairs. These activities encourage bone growth because you move your body against gravity.
- Add some higher-impact movements, like light jumping or skipping, if you are able. These movements further stimulate the bones, but they may not be suitable for people with joint issues or other conditions.
- Include resistance training using bodyweight exercises, resistance bands, dumbbells, or machines. Building muscle around your joints helps protect your bones and improves overall strength.
- Practise balance and flexibility exercises, such as yoga or tai chi, to reduce the risk of falls. Good balance becomes increasingly important as you grow older.
It’s always a good idea to consult your doctor before starting a new exercise routine, especially if you’ve been inactive for a long time, are above 75 years old, or have a medical condition.
3. Lifestyle Improvements
Small lifestyle changes can make a meaningful difference in maintaining strong bones. Managing your daily habits helps balance hormones, support nutrient absorption, and keep your bones and muscles healthy as you age.
Helpful habits include:
-
Take regular movement breaks
Sitting for long hours slows bone and muscle activity, so taking regular movement breaks, such as standing up, stretching, or walking every hour, helps keep your body active and prevents stiffness.
-
Practise good posture
Maintaining proper posture while sitting or standing reduces unnecessary strain on your spine and promotes healthier alignment.
-
Maintain a healthy weight
Being underweight reduces bone reserves, while muscle loss weakens the support around your bones. Eating balanced meals and engaging in strength-building exercises help maintain a healthy weight and muscle mass.
This habit is especially important for underweight individuals, older adults losing muscle, and people recovering from illness or injury.
-
Get enough sleep and manage stress
Poor sleep and chronic stress disrupt hormone levels that regulate bone formation, so prioritising rest and stress management can help your body rebuild bone more effectively.
This is especially important for women with PCOS or hormone imbalance, and individuals with busy or demanding work schedules.
-
Get regular sunlight exposure
A few minutes of morning sunlight boosts vitamin D levels, which supports calcium absorption and overall bone strength.
-
Stay hydrated throughout the day
Drinking enough water supports nutrient transport, joint lubrication, and overall body function, all of which indirectly contribute to healthier bones.
-
Avoid smoking and limit alcohol consumption
Smoking weakens bone-forming cells and reduces calcium absorption, while excessive alcohol disrupts hormone balance and slows bone rebuilding.
Reducing or avoiding these habits helps protect long-term bone health, especially for men who smoke regularly or individuals with existing hormonal issues.
-
Choose a balanced, minimally processed diet
A diet high in sugar, salt, and processed foods disrupts nutrient absorption and gut health, potentially weakening bones over time. Prioritising whole foods, lean protein, and vegetables supports healthier bones, especially for individuals with diets that rely heavily on processed foods.
4. Fall Prevention
Preventing falls is an integral part of protecting your bones, especially as you get older. Simple changes in your home and daily routine can greatly reduce the risk of slips, trips, and fractures.
-
Improve lighting in your home
Good lighting helps you see obstacles clearly and move safely around your home. This is especially important for older adults or anyone with vision difficulties.
-
Remove clutter and secure loose items
Clearing walkways, securing loose carpets, and keeping frequently used items within easy reach reduces the risk of tripping.
-
Use non-slip mats in bathrooms and kitchens
Wet surfaces are a common cause of falls, so using non-slip mats helps prevent slipping in high-risk areas.
-
Wear supportive, non-slip footwear
Proper footwear improves stability and reduces the chances of slipping on smooth or wet floors. This habit is especially important for seniors and individuals with weak leg muscles.
-
Add safety features like grab bars or handrails
Installing grab bars in bathrooms or handrails on stairs provides extra support and confidence during movement.
-
Keep floors dry and clean
Wiping spills immediately and ensuring floors are not slippery helps reduce fall risk in the home.
-
Strengthen your legs and practise balance exercises
Improving leg strength and balance through simple exercises reduces fall risk and improves stability. This is especially helpful for older adults and those who have experienced previous falls.
Early Screening and Detection in Malaysia
Early screening is one of the most effective ways to detect bone loss before it becomes severe. A bone density test (called a DXA scan) measures how strong your bones are and identifies your risk of fractures. This test is quick, painless, and widely available in many Malaysian hospitals and medical centres.
Detecting bone loss early gives you the chance to take action before it progresses. With the right guidance, you can strengthen your bones through lifestyle changes, targeted exercises, supplements, or appropriate medical treatment.
Screening is especially important for:
- Adults over 50
- Post-menopausal women
- Long-term steroid users
- Individuals with a family history of osteoporosis
- Anyone unsure of their bone health or who has multiple risk factors
Take Control of Your Bone Health with Early Screening!

Strong bones are essential for healthy aging, and early detection of bone loss is one of the most effective ways to prevent osteoporosis and future fractures.
At Island Hospital, the Executive Health Screening Package provides a thorough assessment of your overall health — helping to identify risk factors that may contribute to weak bones, hormonal imbalance, vitamin deficiencies, or early bone loss.
For RM760, you’ll receive expert care, advanced diagnostic tests, and a personalised consultation to help you understand where your bone health stands and what steps you can take to protect it.
What’s Included in Your Screening Experience:
- Comprehensive blood tests (to check calcium levels, vitamin D status, inflammation markers, and overall health)
- Chest X-ray
- Electrocardiogram (ECG)
- Ultrasound abdomen & pelvis
- Urine analysis
- Physical examination and detailed consultation
Taking a proactive approach to screening empowers you with early insights, so you can strengthen your bones, adjust your lifestyle, and reduce your long-term risk of osteoporosis.
Support Your Bones with Early Detection!
Living with weak bones or the fear of fractures can be overwhelming — but with the right guidance and early action, osteoporosis can be prevented and managed effectively. From improving your nutrition and staying active to making simple daily lifestyle changes, protecting your bones starts with understanding what your body needs.
At Island Hospital, our team of orthopaedic specialists is dedicated to supporting your bone health through comprehensive assessments, expert consultations, and personalised recommendations. With access to advanced screening tools and a holistic approach to prevention, we’re here to help you stay strong at every stage of life.
Let us support you on your journey to lifelong bone strength — Schedule an appointment today!
FAQ
Is osteoporosis reversible once diagnosed?
Osteoporosis cannot be fully reversed, but it can be managed and improved with the right treatment. Medications, lifestyle changes, adequate calcium and vitamin D, and weight-bearing exercises can help slow bone loss and, in some cases, improve bone density over time.
Can someone be “too active” and harm their bone health?
Yes, excessive or high-intensity exercise without proper nutrition can harm bone health. Overtraining may increase the risk of stress fractures, especially in people who are underweight or have low energy availability. Very intense endurance sports (like marathon running) can also reduce hormone levels if not balanced with proper rest and nutrition.
Can osteoporosis occur in younger adults?
Yes, osteoporosis can occur in younger adults, although it is less common. Factors like eating disorders, long-term steroid use, hormonal imbalances (PCOS, thyroid disorders), low vitamin D, gastrointestinal diseases, being underweight, or genetics can lead to early bone loss.
Are there early warning signs of bone weakness before a fracture?
Osteoporosis is often called a “silent disease” because most people have no symptoms until a fracture occurs. However, some early signs may include:
- Loss of height over time
- Back pain caused by vertebral compression
- A stooped or hunched posture
- Fragile nails
- Weak grip strength
These symptoms aren’t always obvious, so screening remains the best way to detect bone loss early.
How often should I get a bone density test?
Most healthy adults only need a bone density test every 2–5 years, depending on risk factors. However:
- Women over 65 and men over 70 should test at least once every 2 years.
- Adults 50+ with risk factors (steroid use, family history, early menopause, smoking) may need more frequent testing.
- Younger adults with medical conditions that affect bone health may be tested more often.
Your doctor will recommend the right frequency based on your individual risk profile.






