18 Jul How to Prevent Liver Cancer: Simple Steps for a Healthy Liver
How to Prevent Liver Cancer: Simple Steps for a Healthy Liver
By Island Hospital | July 17, 2024 12:00:00 PM
Medical Reviewer: Dr. Tang Weng Heng , Clinical Oncologist
The liver is a vital organ responsible for filtering toxins from your blood, producing proteins, and aiding digestion.
Unfortunately, this sixth most common cancer remains a significant public health concern.
While certain risk factors cannot be controlled, a growing body of research suggests that proactive measures can be taken to promote liver health and potentially reduce the risk of developing this disease.
In this article, we’ll explore key strategies for liver cancer prevention, discuss modifiable risk factors, outline evidence-based lifestyle choices, and emphasise the importance of regular check-ups for early detection.
What is Liver Cancer?
Liver cancer develops from abnormal cell growth within the liver. These cancerous cells can vary in type, leading to different subtypes of the disease.
Some may be benign (harmless) while malignant (cancerous) ones and can spread throughout the body.
The most common form, Hepatocellular Carcinoma (HCC), makes up roughly 90% of all liver cancers. It originates specifically in hepatocytes, the liver’s primary functional cells.
The cause and treatment for these tumours vary depending on the specific type. Therefore, it is crucial to understand the type of tumour in determining a patient’s prognosis.
Risk Factors for Liver Cancer
Risk factors represent any identifiable characteristic that increases an individual’s likelihood of developing a specific disease, such as cancer.
However, the specific risk factors associated with different cancers can vary significantly.
Major Risk Factors for Liver Cancer
- Chronic infection with hepatitis B virus (HBV)
Transmitted through blood, semen, and other fluids, HBV can spread from mother to child, via sex, or sharing needles.
It inflames the liver and can lead to cancer. Routine childhood vaccination is reducing HBV infections, but in some areas, chronic HBV remains a top cause of liver cancer.
- Hepatitis C virus (HCV)
Spread mainly through shared needles and less commonly through sex, Hepatitis C (HCV) can cause cirrhosis and lead to liver cancer. But modern blood screening minimises transfusion risk.
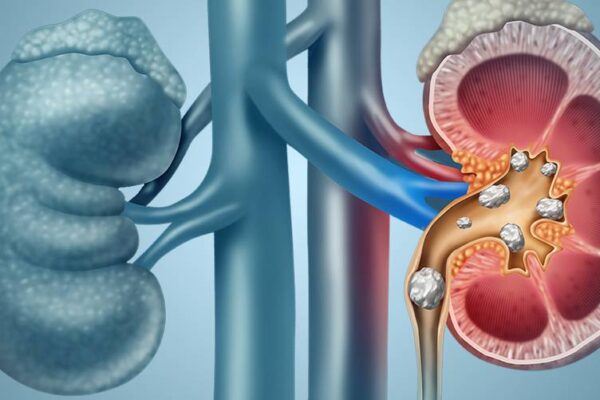
- Cirrhosis
Cirrhosis (scarred liver) sharply raises liver cancer risk. This scarring, often caused by chronic alcohol or HCV infection, disrupts function and blood flow. Importantly, HCV-related cirrhosis carries a higher cancer risk than those from HBV or alcohol.
- Heavy alcohol consumption
Heavy drinking can trigger cirrhosis, a strong risk factor for liver cancer, but also directly cause it even without cirrhosis.
Studies show a tenfold increase in liver cancer risk for heavy drinkers with cirrhosis compared to those without.
Did you know individuals with liver disease have a higher risk of cancer? Learn how to identify the signs and symptoms of liver disease in our complete guide.
Other Risk Factors for Liver Cancer
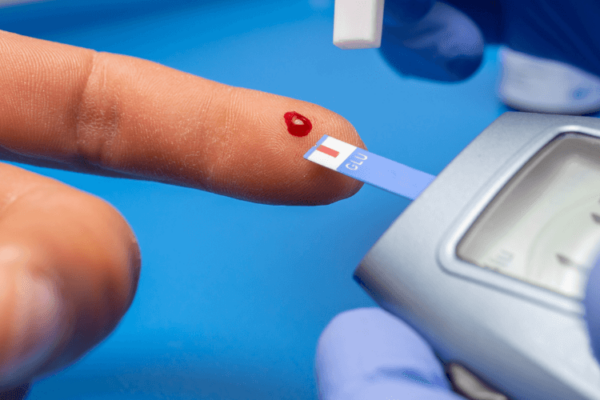
- Diabetes
Individuals with diabetes face a heightened risk of developing liver cancer compared to those without the condition.
- Gender
While HCC strikes men far more frequently than women, this is likely due to behavioural influences on some risk factors mentioned earlier. Interestingly, the fibrolamellar subtype of HCC shows a higher prevalence in women.
- Obesity
Excess weight (obesity) is a known risk factor for liver cancer, possibly due to its association with fatty liver disease and cirrhosis.
- Tobacco use
Smoking elevates your risk of developing liver cancer. While quitting lowers the risk compared to current smokers, both groups remain at higher risk compared to those who never smoked.
- Certain diseases
Some of these diseases also increase the risk of liver cancer:
(i) Tyrosinemia
(ii) Alpha1-antitrypsin deficiency
(iii) Porphyria cutanea tarda
(iv) Glycogen storage diseases
(v) Wilson disease
However, the identification of a risk factor, or even several, does not establish a definitive diagnosis of the disease as some patients diagnosed with the disease may present minimal or undetectable known risk factors.
This is why regular health screenings and consultations with your doctor are crucial for early detection and personalised advice
Symptoms of Liver Cancer?
Liver cancer in its early stages is often undetectable because it may not cause any noticeable symptoms. However, as the disease progresses, some common signs can emerge, including:
- Abdominal pain or swelling
- Darkened urine
- Loss of appetite
- Nausea and vomiting
- Pale stools
- Unexplained weight loss
- Weakness and fatigue
- Yellowed of the skins and eyes (Jaundice)
It’s crucial to seek medical attention immediately if you experience any of these symptoms. Early detection is essential for effective treatment of liver cancer.
How Can I Prevent Liver Cancer?
While liver cancer can be a serious concern, the good news is that there are steps you can take to potentially lower your risk.
By adopting a proactive approach to your health, you can empower yourself to reduce your risk factors and safeguard your liver health.
Reduce Your Risk of Viral Hepatitis
- Get Vaccinated Against Hepatitis B
The hepatitis B vaccine is highly effective in preventing infection. Vaccination is routinely recommended for infants and can be given to adults at risk.
- Get Tested for Hepatitis B and C
Early detection and treatment of hepatitis B and C infections can significantly reduce the risk of developing liver cancer. Discuss testing with your doctor.
- Practise Safe Sex
Hepatitis B can be transmitted through sexual contact. Using condoms consistently can help reduce the risk of infection.
Maintain a Healthy Lifestyle
- Achieve and Maintain a Healthy Weight
Obesity is a risk factor for liver cancer. Maintaining a healthy weight through diet and exercise can help reduce your risk.
- Don’t Smoke
Smoking increases your risk of various cancers, including liver cancer. Quitting smoking or avoiding it altogether is crucial.
- Eat a Balanced Diet
Consume a healthy diet rich in fruits, vegetables, and whole grains while limiting processed foods, red meat, and saturated fats. Avoid foods with high cholesterols and decrease your sugar intake.
- Limit Alcohol Consumption
Heavy alcohol consumption is a major risk factor for liver damage and cancer. Aim for moderation or abstinence.
Other Preventive Measures
- Avoid Exposure to Aflatoxins
Aflatoxins are toxins produced by certain moulds that can contaminate grains and nuts. Avoid consuming mouldy or potentially contaminated foods.
- Discuss Risk Factors with Your Doctor
If you have a family history of liver cancer or other risk factors, talk to your doctor about additional preventive measures or monitoring strategies.
Remember: While these steps can help reduce your risk of liver cancer, they don’t guarantee complete prevention. Regular checkups and screenings remain important for early detection.
Did you know that unhealthy eating habits pose a risk to liver cancer? Read this guide on Malaysian healthy plate to discover how to make your diet healthier.
Early Detection Saves Lives: Protect Your Liver
Early detection of liver cancer is crucial for successful treatment outcomes.
By taking proactive steps today, you can significantly contribute to safeguarding your liver health and potentially promoting a longer, healthier future.
At Island Hospital, our dedicated team of renowned oncologists and supportive staff are here for you, every step of the way. We offer a personalised and comprehensive approach to cancer care and a healthy lifestyle for you.
From advanced diagnostics to cutting-edge therapies and compassionate support, our dedicated centre provides the expertise and resources to empower you in your fight against bladder cancer.
Schedule a consultation with us today to learn more about our world-class treatment options and our unwavering commitment to your comfort throughout your journey. Your path to recovery begins here.
Take Charge of Your Health Today!

Introducing our Executive Health Screening Package for just RM760.
This comprehensive health check includes a physical examination, complete medical report, consultation with a health screening physician or specialist, light refreshments, and an exclusive Island Hospital woven bag.
Prevention is always better than cure, so take charge of your well-being by booking our Executive Health Screening Package today!
FAQ
1. How do I know if my liver is healthy?
It’s important to note that there isn’t a single definitive way to know for certain if your liver is completely healthy. However, there are several signs and tests that can indicate potential issues.
It’s important to consult with a doctor to determine which tests are right for you. They will consider your symptoms, risk factors, and medical history when making recommendations.
Early detection of liver problems is crucial, so don’t hesitate to discuss your concerns with a healthcare professional.
2. How to detect liver cancer early?
It is often difficult to detect liver cancer as signs and symptoms do not appear until its later stage.
Screening tests would be needed for people who have no symptoms or history of cancer but for people at higher risk, there several tests can be conducted.
Some tests commonly used to detect liver cancer includes:
- Blood tests
(i) Liver Function Tests (LFTs)
This standard panel measures the levels of various enzymes and proteins produced by the liver. Abnormal levels can indicate potential damage or dysfunction.
(ii) Alpha-Fetoprotein (AFP) Blood Test
This test measures a protein produced by the liver. Elevated AFP levels can be a sign of liver cancer, but it’s not definitive and other factors need to be considered.
(iii) Viral Hepatitis Tests
These blood tests specifically screen for infections like Hepatitis B and C, which can damage the liver.
- Imaging Tests (if needed):
(i) Ultrasound
(ii) CT Scan or MRI
3. Can fatty liver turn into cancer?
Yes, fatty liver disease, especially NASH (Nonalcoholic Steatohepatitis), can raise your risk of liver cancer. Fatty buildup in the liver (NAFLD) can sometimes progress to NASH, which involves inflammation and cell damage.
This ongoing damage increases the risk of liver cancer (HCC). While not everyone with fatty liver gets cancer, the risk is higher with NASH and other factors like obesity or diabetes.
Maintaining a healthy weight through diet and exercise can significantly reduce your risk. Talk to your doctor for personalised advice.
4. What foods are good for liver repair?
While there’s no magical cure or single food that can “repair” a damaged liver, a healthy diet plays a crucial role in supporting liver function and promoting overall health.
Here are some types of foods that can benefit your liver:
- Fruits and vegetables (e.g., berries, cruciferous vegetables)
- Healthy fats (e.g., fish, beans, lentils, tofu)
- Lean protein sources (e.g, avocados, nuts, seeds, olive oil)
- Whole grains (brown rice, quinoa, whole-wheat bread)
It’s important to consult with a doctor or registered dietitian for personalised dietary advice specific to your health condition and needs.
There’s no one-size-fits-all approach, and a well-rounded, balanced diet is essential for optimal liver health.