
15 Aug Ask Our Parkinson’s Specialists: Addressing Your Concerns About a New Parkinson’s Diagnosis
Ask Our Parkinson’s Specialists: Addressing Your Concerns About a New Parkinson’s Diagnosis
By Island Hospital | August 15, 2025 10:34:09 AM
A Parkinson’s diagnosis can indeed feel like a moment that changes everything.
Beyond the initial shock, you might find yourself navigating a complex landscape of emotions—overwhelm, fear, confusion, and even a profound sense of grief for what feels lost.
These feelings of anxiety about what comes next, frustration with mobilities, or even sheer embarrassment due to the experienced symptoms is what most patients with Parkinson’s face.
Here at Island Hospital, we’ve had the privilege of supporting many individuals and families walking the journey with Parkinson’s. Because of this, we truly understand the weight of this experience and all the questions that come with it—even the ones you might feel worried or embarrassed to ask.
Designed with you in mind, this guide aims to answer your urgent, perhaps unvoiced, questions and debunk common myths, ensuring you’re fully prepared for your next doctor’s visit.
What is Parkinson’s Disease?
Parkinson’s disease is an age-related degenerative brain condition, where certain parts of your brain gradually deteriorate over time.
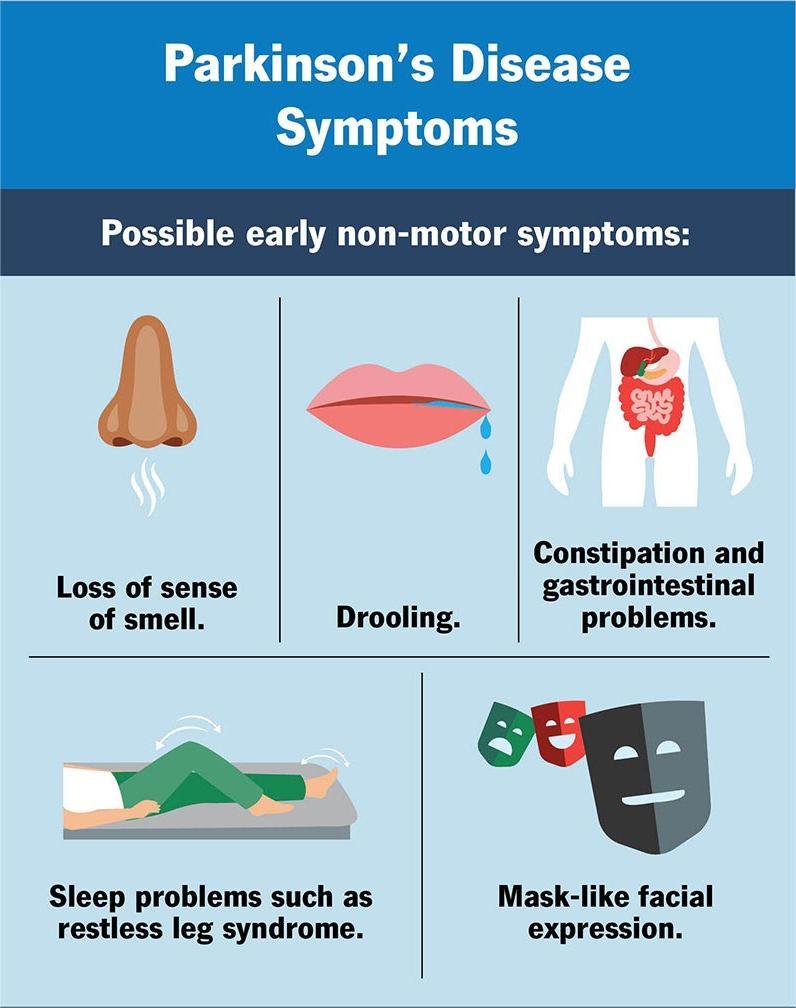
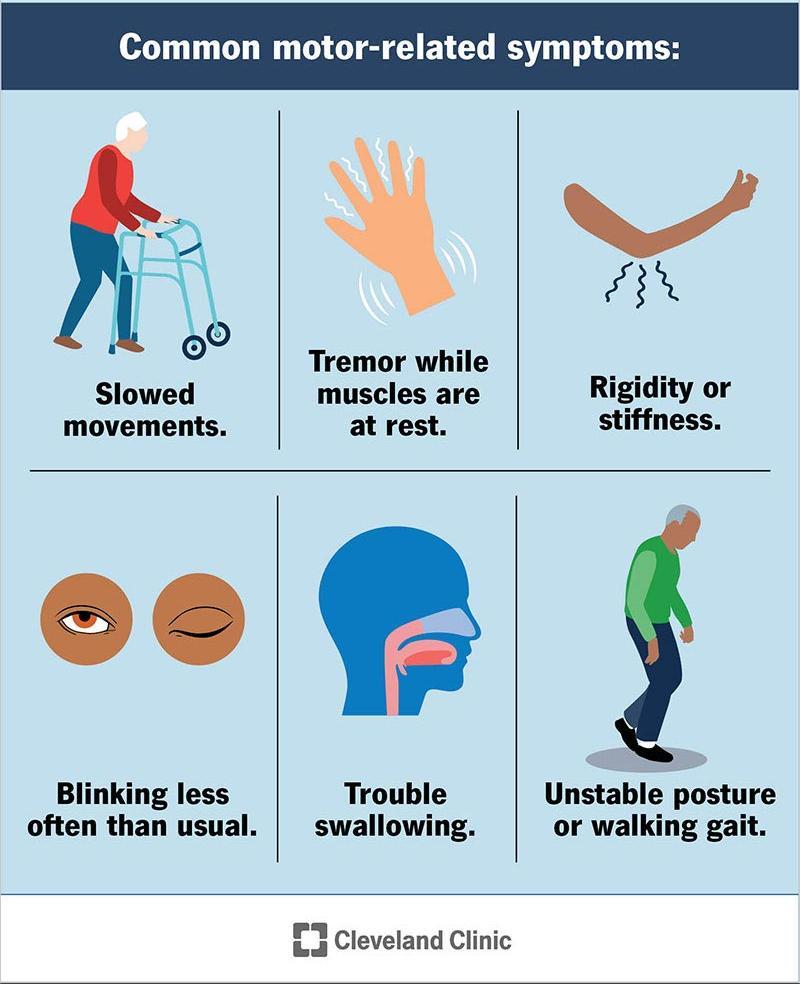
It’s commonly known for causing slowed movements (bradykinesia), tremors and balance problems, with symptoms often beginning subtly and intensifying as the disease advances.
Beyond motor symptoms, many people with Parkinson’s also experience non-motor symptoms such as:
- Sleep problems
- Loss of smell
- Constipation
- Mood disorders like anxiety and depression
While the exact cause of Parkinson’s is often a mystery, with some cases being inherited, the good news is that research is constantly advancing, bringing new insights and understanding.
Although a cure isn’t yet available, the landscape of treatment options is incredibly diverse and continually expanding, offering many ways to effectively manage symptoms and enhance quality of life.
Understanding Your Diagnosis
1. How Is Parkinson’s Diagnosed?
Diagnosing Parkinson’s disease isn’t as simple as a single test. Instead, doctors make a clinical diagnosis, carefully evaluating various factors to reach a conclusion.
It comprises several assessments made based on a thorough neurological examination, a review of your medical history, and an assessment of your signs and symptoms.
Relying purely on clinical diagnosis definitely has its flip side. That’s actually why new criteria from the International Parkinson and Movement Disorder Society are now used, reflecting our most current understanding of the condition.
These updated guidelines help doctors reach a more accurate diagnosis, allowing patients to begin treatment at earlier stages.
Your doctor may also order imaging tests, such as an MRI or PET scan, to rule out other conditions that could mimic Parkinson’s symptoms.
2. Is it normal to feel scared, confused, or angry?
The feeling of being scared, confused, or angry when receiving a Parkinson’s diagnosis is understandable and absolutely normal.
Being diagnosed with Parkinson’s can be a life-altering event, and it’s entirely normal to experience a wide spectrum of emotions. However, it is important to always allow yourself to feel these emotions without judgment.
Talking to trusted family members, friends, or a mental health professional can be incredibly helpful in processing your feelings. Remember, acknowledging your emotions is the first step towards coping and moving forward.
3. What should I expect in the first weeks after a Parkinson’s diagnosis, and what are the most important things to do in the first month?
The initial period after diagnosis can be disorienting for many. Let us help you highlight what to expect and some crucial steps to take your first month:
- There will be a lot of new information to take in upon your diagnosis. However, try not to feel pressured in absorbing everything at once but take it in slow.
- Love is one of the best medicines. While it’s completely normal for your feelings to fluctuate like an emotional rollercoaster, through it all, remember to be patient and kind to yourself.
Once you receive a diagnosis, your doctor will likely discuss initial treatment options and next steps with you. Having someone accompany you to these appointments can be incredibly helpful; they can offer support and ensure no crucial details are missed.
Important things to do in the first month:
1. Educate Yourself (Gradually): Begin to learn about Parkinson’s from reliable sources. Focus on understanding your specific diagnosis and what it means for you.
2. Start a Symptom Journal: It’s incredibly helpful to begin noting your symptoms, their severity, and how they impact your daily life.
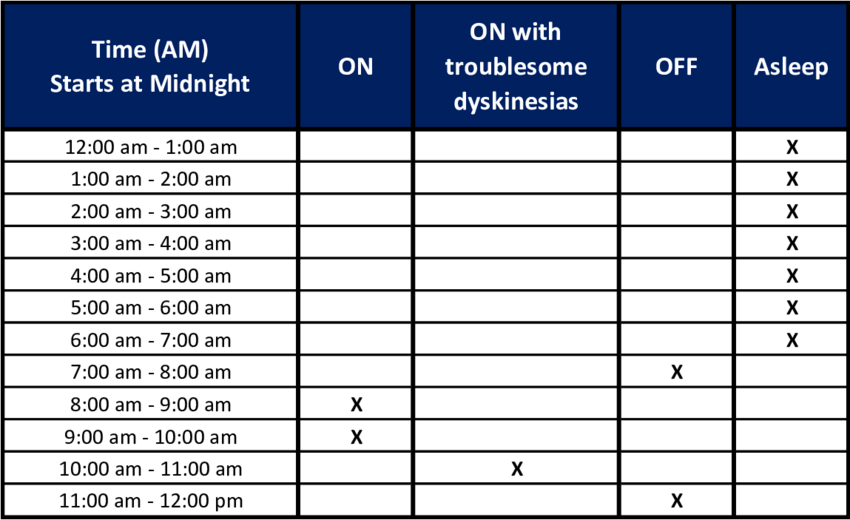
Tracking these changes, especially anything noticeable or progressive, will provide valuable data for your doctor in tailoring your treatment plan.
Here’s one example of a Parkinson’s Symptom Diary you can download to track!
3. Prioritise Self-Care: Self-care should always be your top priority, even amidst challenges. Remember, even small, consistent steps can make a significant difference in your overall well-being.
This includes things like ensuring you get adequate sleep each night, incorporating light exercise into your routine, and maintaining a balanced, nourishing diet. These seemingly minor adjustments can collectively contribute to a better quality of life and help you feel more in control.
4. Connect with Support: If you feel comfortable, share your diagnosis with a few trusted individuals in your life. Opening up to close friends or family can provide an invaluable support system, offering comfort and understanding as you navigate this journey.
5. Prepare for Your Next Appointment: If you have any doubts or concerns, it is encouraged to write them all down to ensure you address them with your doctor on the next visit.
Taking a proactive approach to your health starts with effective screening. Discover how to best prepare for your health screening in this comprehensive guide.
Choosing the Right Specialist
4. What’s the difference between a movement disorder specialist (MDS) and a general neurologist?
While both general neurologists and movement disorder specialists (MDS) are trained to diagnose and treat neurological conditions, an MDS possesses additional, highly specialised training focused specifically on movement disorders like Parkinson’s disease.
This advanced expertise means they have a deeper understanding of the nuances of Parkinson’s, including its various presentations, progression patterns, and the latest treatment advancements.
Let’s have a look at their differences:
| Feature | General Neurologist | Movement Disorder Specialist (MDS) |
|---|---|---|
| Scope of Practice | Diagnoses and treats a wide range of neurological conditions affecting the: | Focuses specifically on diagnosing and treating movement disorders such as: |
| Training | Completes medical school, a one-year internship, and a three-year residency in neurology. | Completes the same training as a general neurologist, plus an additional 1-2 years of specialised fellowship training focused exclusively on movement disorders. |
| Depth of Expertise | Broad knowledge across many neurological conditions. | Deep, specialised expertise in the intricacies of movement disorders, including their varied symptoms, progression, and management. |
| Familiarity with Specific Conditions | May treat Parkinson's disease as one of many conditions in their practice. | Sees a high volume of patients with Parkinson's disease and other movement disorders, leading to extensive experience and up-to-date knowledge of the latest research and treatments. |
| Medication Management | Prescribes and manages medications for a wide range of neurological conditions. | Highly skilled in optimising and adjusting medications specifically for movement disorders, understanding subtle nuances, side effects, and advanced treatment strategies. |
| Advanced Treatments | May refer to specialists for advanced treatments. | Often has expertise in and can manage advanced treatments like Deep Brain Stimulation (DBS) programming and Botulinum Toxin injections for specific movement-related symptoms. |
| Research & Clinical Trials | Generally aware of broader neurological research. | Often actively involved in or has direct access to the latest research and clinical trials for movement disorders, potentially offering patients opportunities for cutting-edge therapies. |
5. Why should I consider seeing an MDS as soon as possible?
Seeing an MDS early in your journey can be incredibly beneficial. Their specialised knowledge allows for a more accurate diagnosis, a more tailored and effective treatment plan from the outset, and faster adjustments to medications as your condition evolves.
This can significantly reduce trial-and-error in managing your symptoms and potentially slow disease progression, ultimately leading to a better quality of life.
6. How do I find and choose the right Parkinson’s specialist, and what questions should I ask to evaluate them?
Finding the right specialist is a first crucial step. Here’s how to approach it and what to ask:
- Referrals: Ask your diagnosing physician for a referral to an MDS.
- Hospital Affiliations: Look for neurologists affiliated with hospitals that have dedicated movement disorder clinics or Centers of Excellence.
Questions to ask when evaluating a specialist:
- Experience: “How many Parkinson’s patients do you see annually?”
- Specialisation: “What percentage of your practice is dedicated to movement disorders?”
- Multidisciplinary Team: “Do you work with a multidisciplinary team (e.g., physical therapists, occupational therapists, speech therapists, dietitians)?”
- Accessibility: “What is your typical response time for patient inquiries?”
- Patient Philosophy: “How do you involve patients in their treatment decisions?”
- Research & Clinical Trials: “Are you involved in any Parkinson’s research or clinical trials?”
At Island Hospital, our Movement Disorder Clinic is staffed by highly experienced neurologists with specialised training in movement disorders. We encourage you to learn more about our team and how we can support you by visiting our Island Hospital Movement Disorders Centre.
Common Questions After a Diagnosis
It’s completely natural to have a whirlwind of questions and concerns after receiving a diagnosis. We understand that your mind might be racing, and you’re likely wondering what comes next.
Fret not as we address some of the most common questions and thoughts that newly diagnosed patients often have:
7. What if I can’t keep working?
Juggling the demands of managing a chronic condition like Parkinson’s while also needing to earn a living can be immensely challenging for your mental well-being. It’s a heavy burden to carry, and it’s completely understandable if you feel overwhelmed by the constant balancing act.
The good news is that many people with Parkinson’s successfully maintain their careers for years, especially with the right strategies in place.
Effective symptom management and workplace accommodations can make a huge difference. It’s a great idea to have an open conversation with your employer about your needs and to work closely with your healthcare team to explore what adjustments might help you continue.
Remember, resources like vocational rehabilitation services are also there to offer valuable support and guidance, helping you navigate your options and find solutions that work best for you.
8. Will I lose my independence quickly?
It is one myth among the many that most patients with Parkinson’s will need to be highly dependent on their caretaker. However, Parkinson’s patients can maintain their independence for a significant period with the right care and proactive management.
Early intervention, consistent medication, lifestyle adjustments, and therapies can help you preserve your functional abilities and quality of life for many years.
9. How fast does Parkinson’s usually progress?
Parkinson’s progression varies significantly from person to another as it’s a highly individual disease. While symptoms generally worsen over time, there is no fixed timeline for the rate of its progression.
However, your doctors can foresee these general stages of progression:
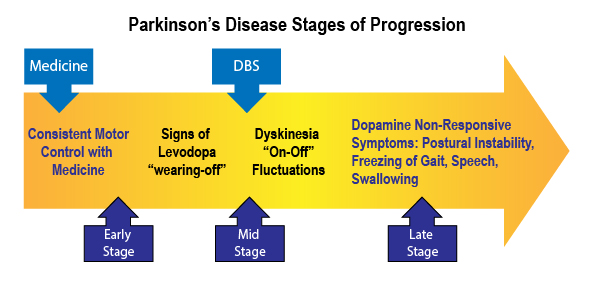
Northwest’s Parkinson’s Foundation
Therefore, regular monitoring with your specialist will help track your unique progression and adjust your treatment plan accordingly.
10. Should I start medication immediately?
The decision to start medication is a personal one, made in consultation with your doctor. It depends on the severity of your symptoms and how they impact your daily life.
Your specialist will weigh the benefits of symptom control against potential side effects to determine the optimal timing for starting medication.
11. Can diet really make a difference in my symptoms?
It is true that managing your eating habits well can make a difference in your symptoms. Although it may not be the cure for Parkinson’s, research has shown that a well-balanced, nutritious diet can play a supportive role in managing symptoms and overall well-being.

For example:
- High-fiber diets can help with constipation, a common non-motor symptom in most Parkinson’s patients . Some people also find certain foods trigger or alleviate their symptoms.
- Drinking sufficient fluids will maintain your balance and prevent kidney problems as the medications used to treat this disease often causes dehydration.
- Consuming high-protein foods in the morning especially when you’ve taken your medicine will maximise the medication’s effects as carbidopa-levodopa (the commonly used drug in treating Parkinson’s) is absorbed in your small intestine.
Some examples of high protein meals you can take include oatmeals or eggs!
12. Is Parkinson hereditary and life-threatening?
In most cases (around 85-90%), Parkinson’s disease is not directly inherited and is considered “sporadic.” However, about 10-15% of cases are thought to have a genetic link.
If you have a family history of Parkinson’s, discussing it with your doctor is advisable. Island Hospital provides excellent information on the genetics of Parkinson’s.
You can breathe a sigh of relief as Parkinson’s disease itself is not considered a fatal illness. Despite that, complications associated with advanced Parkinson’s, such as falls, pneumonia, or choking due to swallowing difficulties, can be serious and potentially life-threatening when the muscles in your body undergo constriction.
With proper management and support, many people with Parkinson’s live long, fulfilling lives.
It’s easy to dismiss a headache, but knowing the signs of something more serious can bring peace of mind. Read up on: Brain Tumours: Everything You Need to Know.
Lifestyle Changes
Making simple adjustments to your daily routine can significantly improve your quality of life with Parkinson’s.
13. What simple lifestyle changes can help me feel better right away?
Making small, consistent changes to your daily routine can have a surprisingly big impact on how you feel, both physically and mentally. Think of these as simple, everyday habits that your body will truly thank you for:
14. How can I make my home safer to prevent falls?
Falls are a significant concern for people with Parkinson’s. Here are some simple home safety checklist that can greatly reduce risk in falling:
- Remove tripping hazards: Clear clutter, loose rugs, and electrical cords.
- Improve lighting: Ensure all areas are well-lit.
- Install grab bars: In bathrooms and near staircases.
- Use non-slip mats: In bathrooms and kitchens.
- Keep pathways clear: Ensure easy movement throughout your home.
Aside from the aforementioned, it is also highly advisable to make some renovations and adaptations to your home for easy manoeuvring to ensure proper safety.
Building a Support System
You don’t have to face Parkinson’s alone. A strong support system is vital for both emotional well-being and practical assistance.
15. Who should be part of my care team besides my doctor?
A strong care team is crucial for navigating Parkinson’s disease, and it’s often a multidisciplinary effort designed to support every aspect of your well-being. This comprehensive approach means you’ll have a dedicated group of professionals working together to empower you, boost your morale, and ensure you live your best life.
Your care team can be multidisciplinary and may include:
- Movement Disorder Specialist (MDS)
- Physical Therapist: To improve mobility, balance, and gait.
- Occupational Therapist: To help with daily activities and adaptive strategies.
- Speech-Language Pathologist: To address voice and swallowing difficulties.
- Dietitian: For nutritional guidance.
- Social Worker/Counsellor: For emotional support and resource navigation.
- Caregivers/Family Members: Your most immediate support.
This team approach not only addresses your physical symptoms but also provides the emotional and practical support that truly boosts your morale and enhances your overall quality of life.
They’re all working together to help you maintain independence and well-being.
16. How do I involve family or caregivers in my care?
Open communication is key. Share information about your condition, your needs, and your feelings. Involve loved ones in appointments to ensure they understand your treatment plan and can help you remember instructions.
What’s important is to clearly communicate how they can best support you, whether it’s through practical help, emotional encouragement, or attending support groups with you.
Why Choose Island Hospital for Parkinson’s Care?
Living with Parkinson’s disease can present physical and mental challenges, and at Island Hospital, we want you to know you’re not alone. Our arms are opened to provide warm, comprehensive, and advanced care, ensuring you feel supported and empowered throughout your journey.
17. What makes Island Hospital different from other Parkinson’s clinics?
Our differentiator lies in our patient-centered approach, combining specialised expertise with a holistic understanding of Parkinson’s impact on your life. We don’t just treat symptoms; we empower you with knowledge, support, and a dedicated team. Our commitment to excellence is reflected in our:
- Dedicated Movement Disorder Clinic: Staffed by highly experienced neurologists with advanced training in movement disorders.
- Multidisciplinary Team: Our specialists collaborate closely to provide integrated care, encompassing neurology, physical therapy, occupational therapy, speech therapy, and nutritional guidance.
- Focus on Patient Outcomes: We continuously monitor and evaluate our patient outcomes to ensure we are providing the most effective and personalised care.
- State-of-the-Art Technology: We leverage the latest advancements in diagnostic tools and treatment modalities, including advanced imaging and Deep Brain Stimulation (DBS) capabilities.
- Emphasis on Education and Support: We believe in empowering our patients and their families with knowledge, offering educational resources and connecting them with support networks.
18. What specialised services does Island Hospital offer for newly diagnosed patients?
For newly diagnosed patients, we offer:
- Expedited appointments with our Movement Disorder Specialists.
- Comprehensive initial assessments to establish a baseline and tailor a personalised care plan.
- Educational resources and access to our patient support programs.
- Guidance on lifestyle modifications and connecting with allied health professionals.
Emotional support and connections to counseling services if needed.
Find Yourself Again
The challenge in having a Parkinson’s diagnosis is not an easy road but it also opens doors to new knowledge, connections, and an opportunity to prioritise your well-being.
At Island Hospital, we’re ready to stand by you on every step of your journey.
Explore our comprehensive Neurology and Neurosurgery Medical Speciality services to learn more about how we can support you.
Ready to start your journey with us? Book a consultation with us today.






