
14 Jul Limb Reconstruction Surgery Recovery: What to Expect & How to Heal Well
Limb Reconstruction Surgery Recovery: What to Expect & How to Heal Well
By Island Hospital | July 14, 2025 10:30:00 AM
At first glance, limb reconstruction surgery might sound intimidating—maybe even a little scary. For many, it conjures up images of complex procedures, long recoveries, and worst-case scenarios. And honestly? It’s completely normal to feel anxious about it. But behind the fear and misconceptions, it’s often not nearly as daunting as it seems.
In fact, whether it’s done to correct bone deformities, repair trauma-related injuries, or lengthen a limb for better movement and balance, limb reconstruction can be a turning point. It’s a chance to move better, feel stronger, and live more comfortably.
Sure, the road to recovery is a process, and yes, it does take time. But with patience, commitment, and the right medical team by your side, real progress isn’t just possible, it’s expected.
In this article, we’ll walk you through what recovery after limb reconstruction surgery really looks like. From phase-by-phase healing timelines and pain management options, you’ll get the guidance you need to recover not just physically, but mentally and emotionally too.
When is Limb Reconstruction Surgery Needed?

Limb reconstruction surgery isn’t something most people expect to need, but for those facing serious bone issues, it can be a vital step toward healing and improved mobility.
1. Severe fractures that won’t heal properly
Also known as non-union fractures, these occur when broken bones fail to mend on their own, even after months of immobilisation or surgery.
2. Bone infections (osteomyelitis)
Infections deep within the bone can cause significant damage, requiring removal of infected tissue and reconstruction of the affected area.
3. Congenital deformities or growth discrepancies
Some children are born with limb differences, like bowed legs or unequal leg lengths, which may worsen over time and affect mobility.
4. Bone loss due to trauma or tumour removal
Severe accidents, such as motor vehicle collisions or falls from height, can cause extensive bone damage or even loss of bone segments. In other cases, surgical removal of bone tumours, such as osteosarcoma or giant cell tumours, may leave gaps or weaken the bone structure.
When a significant portion of bone is missing or unstable, reconstruction is needed to restore limb strength, function, and alignment.
Early detection is the key to preventing serious health problems. Check out Island Hospital’s comprehensive screening services in this article.
Types of Limb Reconstruction Procedures
Limb reconstruction isn’t a one-size-fits-all procedure. Depending on the condition, age, and treatment goals, your orthopaedic surgeon may recommend one or a combination of several surgical techniques.
1. External Fixation

External fixation, like the Ilizarov frame, involves placing a circular or linear metal frame outside the limb, connected to the bone using pins or wires that pass through the skin. It’s commonly used for:
- Stabilising complex or hard-to-heal fractures
- Correcting bone deformities
- Gradually lengthening bones over time
The device may look intimidating at first, but it’s carefully designed to be adjustable, stable, and highly effective during the healing process. It also allows for gradual corrections without the need for additional surgery.
2. Internal Fixation
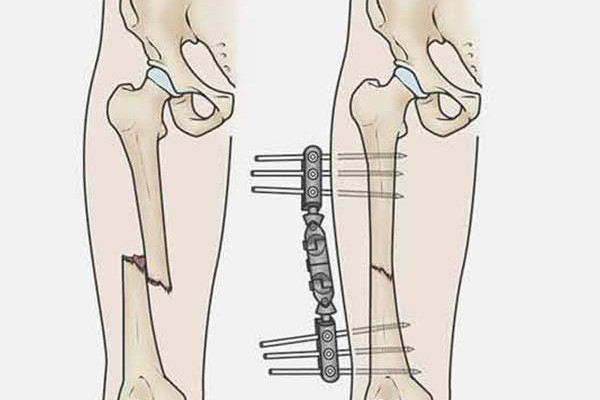
In this method, orthopaedic devices like plates, rods, and screws are implanted inside the body to hold the bone securely in place during healing. This technique is often used for fractures that need internal support or for maintaining alignment after correction.
- Plates and screws to bridge fractures.
- Intramedullary rods are placed within the bone for support.
This option is often preferred when less adjustment is needed after surgery.
3. Limb Lengthening
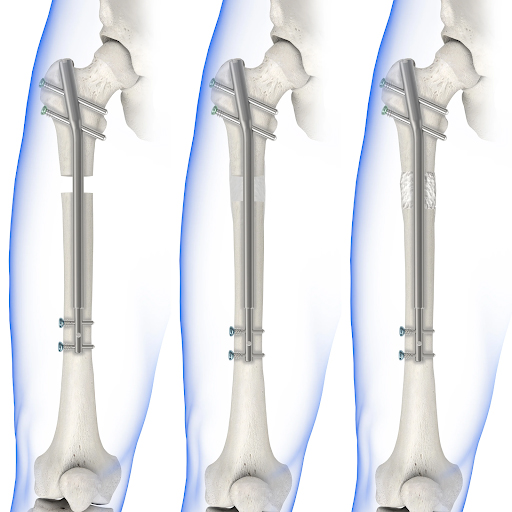
Limb lengthening surgery, such as with the PRECICE nail system, is used to gradually lengthen a shortened limb over time.
The modern PRECICE nail is magnetically controlled, allowing for precise, non-invasive adjustments during follow-up visits, making the entire process more comfortable and manageable for patients.
4. Bone Transport or Regeneration
This technique is used when a portion of bone is missing or has been removed due to trauma or infection. Using external fixation, the surgeon gradually moves a healthy segment of bone into the gap, encouraging new bone to grow behind it. It’s a complex yet powerful method of regeneration.
Diagnosis and Tests Before Limb Surgery
Before recommending limb reconstruction surgery, your medical team will perform a series of evaluations to fully understand your condition. These tests help determine the severity of the issue, rule out other complications, and plan the most suitable surgical approach.
1. Physical examination
Your doctor will assess your limb alignment, joint function, range of motion, and overall mobility to understand how the condition affects your movement and daily life.
2. X-rays
X-rays provide clear images of the bone structure and are often the first step in evaluating fractures, deformities, or length discrepancies.
3. MRI (Magnetic Resonance Imaging)
Used to examine soft tissues, such as muscles, ligaments, and cartilage, especially if the injury involves more than just the bone.
4. CT scan (Computed Tomography)
Offers highly detailed cross-sectional images of the bone and surrounding tissues, useful for planning complex reconstructions.
5. Blood tests
Used to check for infections, inflammation, or underlying conditions (like anaemia or clotting issues) that could affect surgical safety or healing.
What to Expect After Surgery
Recovery from limb reconstruction surgery doesn’t happen all at once; it unfolds in stages. Each phase brings its own set of challenges, milestones, and moments of progress. Here’s what to expect during each stage to help ease anxiety and keep you focused on healing.
1. Hospital Stay (Day 0-7)
Right after undergoing limb reconstruction surgery, you’ll typically spend between 1 to 7 days in the hospital. During this time, your medical team will closely monitor your condition and guide you through the first steps of recovery.
Here’s what you can expect during your hospital stay:
- Monitoring and infection control
Nurses and doctors will regularly check your vital signs, surgical site, and dressings to prevent infection and ensure the area is healing properly. - Pain relief
Pain is managed through nerve blocks, IV medications, or oral painkillers. - Managing swelling and dressings
Swelling is expected and will be controlled using elevation, cold therapy, and careful dressing changes. - Physiotherapy
Passive movements may start as early as Day 2 or 3, depending on your condition, to prevent stiffness and encourage circulation. - Mental and emotional adjustment
It’s common for patients to feel anxious, frustrated, or uncertain during the early stages of recovery. To support you through this, your care team will provide emotional support, ensure adequate rest, and maintain clear communication every step of the way.
2. Recovery at Home (Week 1–4)
Once you’re discharged from the hospital, recovery continues at home. This stage is all about managing pain, preventing complications, and gradually regaining movement.
- Wound and pin-site care
If you have an external fixator, daily cleaning of the pin sites is essential to prevent infection. For internal devices, you’ll need to keep the wound area clean and dry and watch for signs of swelling, redness, or discharge. - Pain management
Oral medications will help control discomfort during this stage. You may also be advised to use anti-inflammatory foods, cold therapy, or gentle movement to ease stiffness and swelling. - Using mobility aids
To avoid putting too much weight on the affected limb, you’ll likely need crutches, a walker, or other assistive devices to move around safely. - Physiotherapy continues
Following the passive movements started in the hospital, home-based physiotherapy or outpatient sessions will usually continue in a more active and structured way.During this phase, patients are guided through specific exercises designed to gently improve joint mobility, maintain muscle activity, and begin rebuilding strength, step by step.
3. Mid-Recovery (Week 4–12)
By this stage, you’re likely starting to feel more stable and confident in your movement. Pain should be more manageable, and your energy levels may begin to improve. However, this is also when patients often feel impatient or discouraged, especially if progress seems slow, but steady improvement is a good sign.
- Partial weight-bearing may begin
With your doctor’s clearance, you can gradually apply weight to the affected limb. This transition is important for building bone strength and balance. - Physiotherapy becomes more active
Your sessions will now include light strengthening, flexibility, and assisted exercises to improve endurance and coordination. - Mobility milestones
You may start walking short distances indoors with minimal support. Daily activities like using stairs, light housework, or standing for longer periods may become possible. - Returning to daily life
Some patients may begin transitioning back to desk-based or hybrid workwith proper accommodations. If cleared, driving may resume around 10–12 weeks post-op, especially if the non-dominant or upper limb was affected.
4. Functional Recovery & Activity Resumption (Month 4-6)
By now, many patients begin to feel a genuine return to normalcy. Pain is significantly reduced, and the focus shifts toward rebuilding strength, endurance, and joint stability.
- More intensive physiotherapy
Rehab now includes strength training, balance exercises, and coordination drills designed to restore functional movement and reduce long-term instability. - Improved independence in daily tasks
You may be able to walk longer distances, stand for extended periods, and move around your home without assistive devices. - Resuming hobbies and light activity
Light activities like gardening, walking, or cooking can be resumed with your doctor’s clearance - Work becomes routine
If you’ve already returned to work in the last few weeks, this is when it starts to feel more manageable. You may now be handling longer hours or more tasks with less fatigue. - Light recreational activities
Under supervision, some low-impact fitness such as stationary cycling or water therapy may be introduced to support stamina and coordination.
5. Long-Term Recovery & Reintegration (Month 6-12)
This phase marks the final stretch of your recovery journey. At this stage, the goal isn’t just recovery, it’s sustainable reintegration. Your limb may feel normal again, but healing continues beneath the surface. Prioritise long-term limb health through regular movement, proper technique, and follow-up visits when needed.
- Return to normal daily activities
Most patients are able to resume full independence in everyday life, including tasks like shopping, commuting, and handling stairs confidently.
- Resuming physical or active jobs
With your surgeon’s clearance, you may return to more physically demanding or manual work.
- Recreational and sports activities
Low-impact sports or fitness routines, such as swimming or gym workout can usually resume under physiotherapist guidance. Higher-impact activities like running, hiking, or contact sports should be gradually reintroduced and only with medical clearance to avoid re-injury.
- Ongoing physiotherapy
While formal physio may taper off, some patients still benefit from occasional sessions to fine-tune strength, gait, or address minor imbalances.
- Joint care and flare-up management
Occasional discomfort, stiffness, or swelling may still occur, especially with weather changes or overuse. Long-term joint care strategies such as stretching, rest days, and supportive footwear help prevent setbacks.
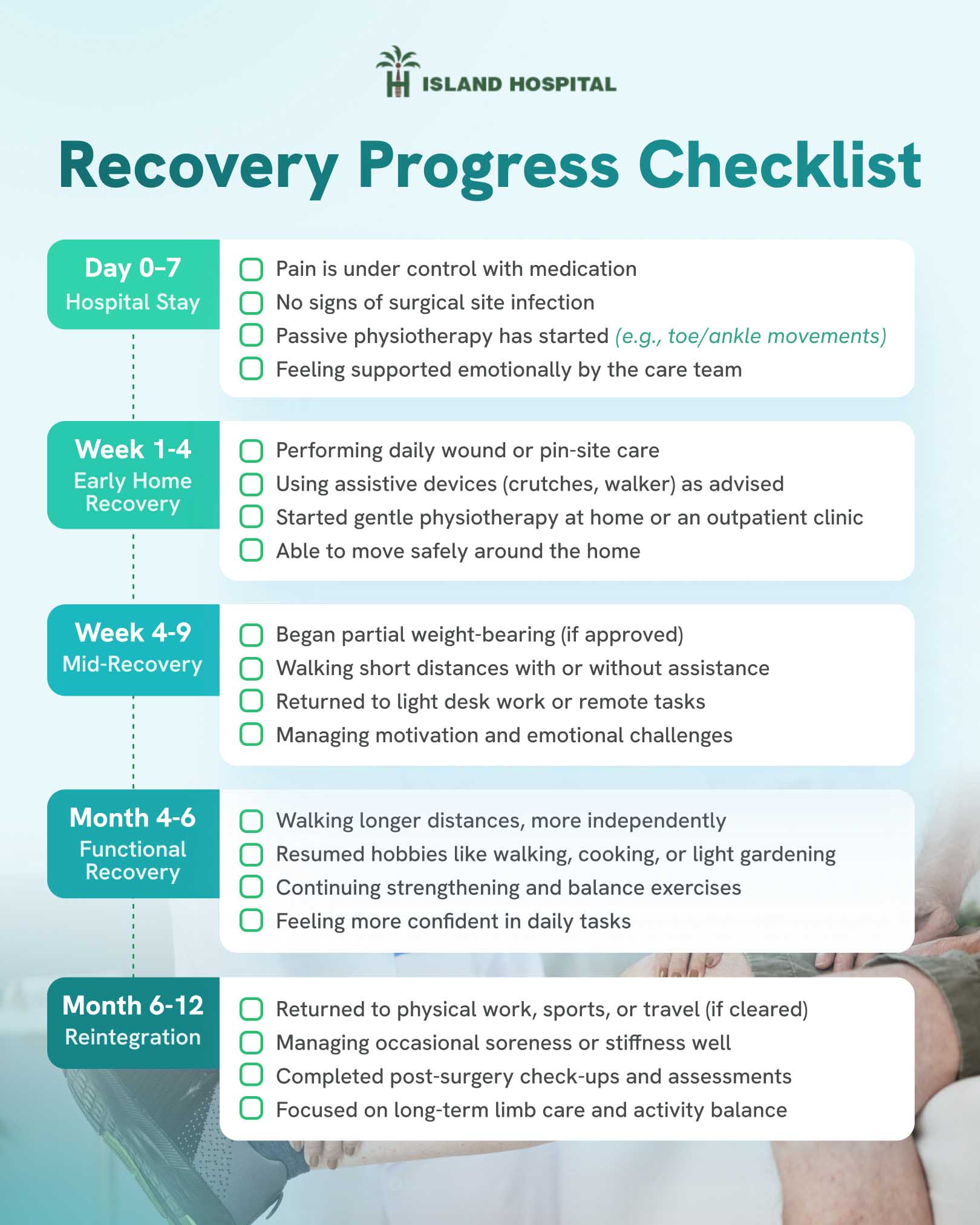
Recovery Progress Checklist
Hospital Stay (Day 0–7)
- Pain is under control with medication
- No signs of surgical site infection
- Passive physiotherapy has started (e.g., toe/ankle movements)
- Feeling supported emotionally by the care team
Early Home Recovery (Week 1–4)
- Performing daily wound or pin-site care
- Using assistive devices (crutches, walker) as advised
- Started gentle physiotherapy at home or an outpatient clinic
- Able to move safely around the home
Mid-Recovery (Week 4–12)
- Began partial weight-bearing (if approved)
- Walking short distances with or without assistance
- Returned to light desk work or remote tasks
- Managing motivation and emotional challenges
Functional Recovery (Month 4–6)
- Walking longer distances, more independently
- Resumed hobbies like walking, cooking, or light gardening
- Continuing strengthening and balance exercises
- Feeling more confident in daily tasks
Reintegration (Month 6–12)
- Returned to physical work, sports, or travel (if cleared)
- Managing occasional soreness or stiffness well
- Completed post-surgery check-ups and assessments
- Focused on long-term limb care and activity balance
Managing Pain Safely and Effectively
Pain is a natural part of the recovery process after limb reconstruction surgery, but with the right approach, it doesn’t have to take over your healing journey. Whether you’re in the hospital or recovering at home, pain can be managed safely through a combination of medical treatments, practical strategies, and gentle alternatives.
1. Immediately After Surgery
In the first few days post-surgery, pain is typically more intense and requires stronger, hospital-managed interventions.
- Nerve blocks
These are used during or immediately after surgery to numb specific nerves and block pain signals from the surgical site. They can provide relief for up to 24–48 hours. - IV medications
Provide fast-acting and controlled pain relief during your hospital stay, ensuring you are comfortable in the immediate post-surgery phase. - Cold therapy
Ice packs or cooling devices are applied to reduce swelling, inflammation, and pain in the affected limb.
2. Mid- to Long-Term Pain Relief
As you transition home, your pain should begin to subside, and your focus shifts to managing discomfort in safer, lighter ways.
- NSAIDs (non-steroidal anti-inflammatory drugs)
Medications like ibuprofen may be prescribed to reduce inflammation and pain. - Paracetamol (acetaminophen)
A common option for general aches and moderate pain. It’s well-tolerated and often used alongside NSAIDs for balanced relief. - Sleep positioning
Elevating the leg or using pillows to support the limb can significantly reduce strain, improve blood flow, and ease nighttime discomfort.
3. Gentle Alternatives and Supportive Therapies
Complementary strategies can be used alongside medication to improve comfort without side effects.
- Mindfulness and breathing techniques
Deep breathing, guided meditation, and relaxation exercises can reduce anxiety and help your body better cope with persistent pain. - Anti-inflammatory diet
Foods rich in omega-3s (like salmon and flaxseeds), turmeric, berries, leafy greens, and nuts may help naturally reduce inflammation in the body. - Hot or cold packs at home
Alternating heat and cold therapy can help with muscle soreness, stiffness, and swelling during recovery. - Gentle massage or acupuncture
With your doctor’s approval, these therapies may help relieve tension and promote healing.
Discover how proper rehabilitation after knee surgery can speed up your recovery, restore mobility, and reduce long-term discomfort. Read more about it here!
Coping with Emotional and Mental Challenges
Recovery isn’t just about healing the body. It’s also about navigating the emotional ups and downs that come with it. Recognising and addressing these feelings can make a meaningful difference in both your recovery and overall well-being.
1. Common Feelings During Recovery
Many patients report:
- Frustration – When progress is slow.
- Helplessness – Due to physical dependence or mobility imbalance.
- Impatient – Wanting to return to normal life faster than the body allows
These feelings are valid and temporary, but they shouldn’t be ignored.
2. Tips to Stay Mentally Strong
- Celebrate small wins
Track your progress weekly, no matter how small. Walking a little further, needing less assistance, or simply feeling better, counts. - Join a support group
Connecting with others who’ve undergone similar surgeries in person or online can reduce isolation and provide hope. - Talk to past patients
Hearing real recovery stories can help you set realistic expectations and feel less alone in your journey. - Set manageable goals with your physiotherapist
Breaking big milestones into weekly goals can reduce the feeling of being overwhelmed and keep you focused.
3. When to Seek Professional Help
Emotional low points are common during recovery, but if you experience any of the following, it may be time to speak with a mental health professional. Seeking support is a sign of strength, and it can play a key role in your overall healing.
Signs to watch for:
- Persistent feelings of sadness, hopelessness, or worthlessness
- High levels of anxiety or panic that interfere with daily life
- Loss of interest or motivation in daily activities
- Social withdrawal from loved ones or support systems
Need support now? Speak to our orthopaedic care team at Island Hospital for expert guidance on your physical and emotional recovery needs.
Practical Tips for Home Recovery

Creating a safe, accessible, and low-stress environment at home can make a big difference during your early recovery. Here are some helpful adjustments and daily tips to support your healing process:
1. Home Adjustments
Make your living space safer and easier to navigate:
- Remove loose rugs or clutter to prevent tripping
- Install grab bars in bathrooms and near stairs
- Use night lights for better visibility during late-night bathroom trips
- Keep essentials like medication, water, and phones within arm’s reach
2. Mobility Aids
Using the right tools can reduce strain and improve confidence:
- Crutches or walkers for safe movement early on
- Knee scooters
- Elevated toilet seats to reduce bending and pressure on joints
3. Daily Life Hacks
Simple adjustments can reduce fatigue and help you maintain independence:
- Prepare meals in batches or arrange for meal delivery services
- Use a shower chair or a handheld shower head for seated bathing
- Ask family or friends to assist with transportation to appointments
Ready to Take the Next Step in Your Recovery?
Limb reconstruction surgery is more than just a physical procedure—it’s a journey of regaining strength, mobility, and confidence. With the right guidance, a strong support system, and a personalised care plan, full recovery is absolutely possible.
At Island Hospital, our team of renowned orthopaedic specialists brings years of experience in bone and joint care, and is committed to supporting every part of your recovery, both physically and emotionally.
FAQ
1. What happens if something feels wrong after I go home?
If you experience unusual pain, fever, redness, swelling, or changes at the surgical site, contact your care team immediately. Early intervention prevents complications. Don’t wait it out, your care team expects you to report anything that feels off.
2. Can I travel while still recovering from limb reconstruction surgery?
Short trips may be possible after the first few months, especially if your doctor clears it and you’re mobile with assistive aids. Long-distance travel or flying may require extra precautions like anti-clotting measures, elevation, or medical documentation.
3. Is limb reconstruction surgery expensive?
Costs can vary depending on the type of procedure, implants used (e.g., external vs internal fixation), and hospital stay duration. While it can be a significant investment, many hospitals offer detailed cost breakdowns and options to help you plan ahead.
4. Will the metal frames or rods be removed?
In most cases, yes. External frames like the Ilizarov device are typically removed after the bone has healed, while internal devices (plates, rods, screws) may stay in place unless they cause discomfort or need to be taken out for another reason.
5. What happens if I miss a physio session or fall behind schedule?
It’s normal to have occasional setbacks, but consistency is key. Missing physiotherapy sessions can delay recovery, reduce mobility gains, or increase stiffness. If you fall behind, inform your care team early so they can adjust your plan and help you get back on track safely.






