
16 Jun Peptic Ulcer Disease: Symptoms, Treatments, and Everyday Management
Peptic Ulcer Disease: Symptoms, Treatments, and Everyday Management
By Island Hospital | June 13, 2025 10:00:00 AM
Let’s take a quick inventory of these sensations:
- Fiery or aching discomfort, similar to hunger pangs
- Constant feeling of fullness or bloating
- Recurring heartburn attacks
Do any of these scenarios sound familiar? If they do, it might be helpful to consider peptic ulcer disease as a possible reason.
Rest assured, this guide is here to be your friendly companion, and together with the resources of Island Hospital, we’ll help you understand what causes these troublesome ulcers, how to spot them, what medical treatments are available, and even some everyday tips for a happy tummy.
What is Peptide Ulcer Disease?
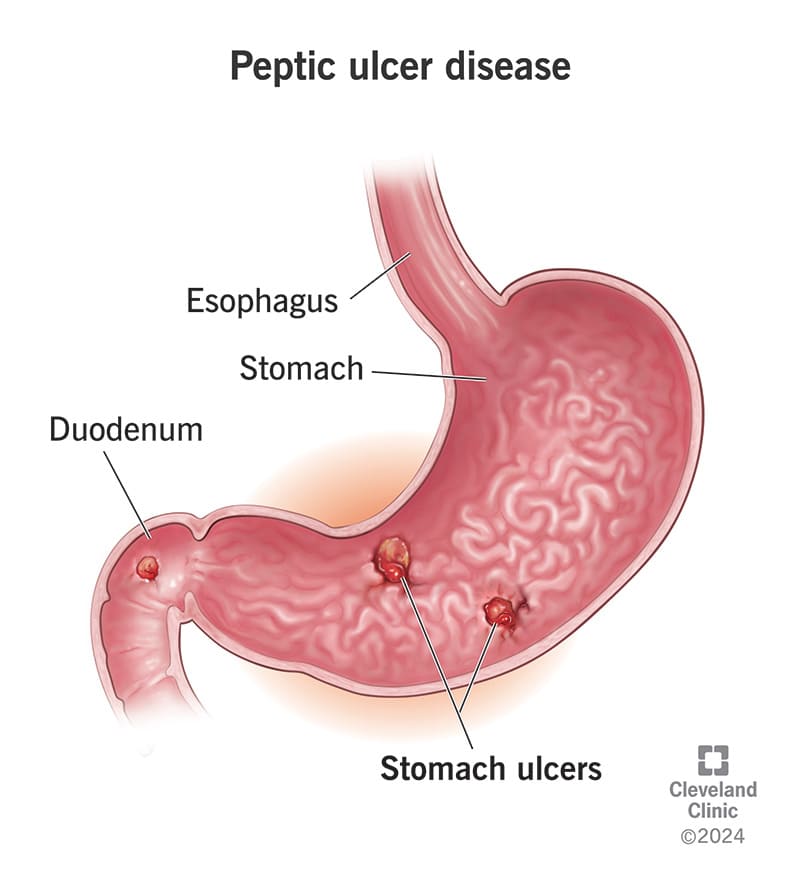
Peptic ulcer disease (PUD) is a condition in which painful little sores (or sometimes not-so-little) develop in the lining of the stomach or the duodenum, the first part of the small intestine.
These sores occur when the protective mucus lining of these organs gets worn away in certain spots, allowing stomach acid to irritate and damage the tissue.
This irritation can cause painful sores to develop – and those sores are what we call peptic ulcers. It’s similar to having a little wound inside that gets constantly irritated by the acid.
What Living with Peptic Ulcer Disease Feels Like
So, those sensations we listed at the start – the fiery pain, the constant fullness, the recurring heartburn?
For someone living with peptic ulcer disease, these aren’t just occasional annoyances, as the spectrum of experiences associated with this condition extends beyond just these:
| Common Signs & Symptoms | Signs & Symptoms of Complications |
|---|---|
|
|
It can be tricky to know if your ulcer is in your stomach or the start of your small intestine (duodenum). But here’s a hint:
- Stomach ulcer pain often gets worse soon after you eat, usually within half an hour, when your stomach is full of digestive juices.
- Duodenal ulcers often feel better after eating, but the pain returns 2 to 3 hours later as food enters the duodenum. Some people even think it’s hunger because eating can temporarily relieve the pain.
Risk Factors in Contracting Peptide Ulcer Disease
Several factors can increase your risk of developing PUD such as:
- H. pylori infection
This is a common type of bacteria that can live in your stomach. While it may not cause problems initially, it can sometimes damage the stomach lining over time. - Regular use of NSAIDs (Nonsteroidal Anti-inflammatory Drugs)
These common pain relievers, like ibuprofen and naproxen, can irritate and damage the stomach and intestinal lining, especially with frequent use. Having both an H. pylori infection and regularly using NSAIDs significantly raises your risk. Even early stages of H. pylori or infrequent NSAID use can combine to cause PUD.
- Other contributing factors
While less likely to cause PUD on their own, smoking, alcohol consumption, and certain other medications can further weaken the protective lining and increase the chances of developing ulcers, particularly when combined with H. pylori infection or NSAID use.
The sound of having an endoscopy might be scary but we’ve got you covered in this article on upper GI endoscopy (OGDS) procedure: what to expect.
Lifestyle Adjustments to Improve Peptic Ulcer Disease
It is undeniable that medical treatments are key to calming things down, but it is also your responsibility to incorporate healthy daily habits to keep the peace and help those little sores heal.
Let’s explore some simple lifestyle shifts that can make a big difference:
1. Nourishing Your Gut
Forget those old-fashioned “ulcer diets.” What truly matters when you have a peptic ulcer is becoming a mindful eater.
Gentle, cooked foods like milk, low-fat cheeses, yogurt, lean proteins such as tender meats and flaky fish, soft cooked veggies, and bananas are incredibly helpful for individuals with PUD.
Conversely, some foods and drinks can really irritate a sensitive gut. It’s wise to limit or even eliminate:
- Alcohol: Due to its potential to irritate the gastric mucosa.
- Coffee and Cola: These beverages possess a high acidity that may exacerbate ulcer symptoms.
- Fatty and Spicy Foods: These can be difficult to digest and may increase gastric irritation.
- Difficult-to-Digest Snacks: Overly processed or heavy snacks can place undue stress on the digestive system.
- Highly Acidic Foods (e.g., Citrus Fruits): While generally nutritious, their acidity may be poorly tolerated.
- Processed Meats: These often contain additives that can be detrimental to the gastrointestinal tract.
2. Proper Stress Management Techniques
Did you know that when you’re stressed, your whole body tenses up, and that can include your digestive system?
Finding your personal recipe for calm – whether it’s gentle walks, listening to soothing music, spending time in nature, or practicing deep breathing – can have a surprisingly positive ripple effect on your ulcer.
Consider these engaging avenues for cultivating inner peace by:
- Embracing mindful moments through yoga sessions
- Connecting with your creative side (e.g. painting, playing musical instruments, writing, or even gardening)
- Nurturing social connections with your loved ones
- Exploring aromatherapy
- Immersing in nature
Engaging in regular physical activity also benefits your overall health and the digestive system by promoting regular bowel movements. This can help mitigate constipation, a factor that may increase the risk of peptic ulcers.
Beyond simply aiding ulcer recovery, embracing stress management techniques is a valuable investment in your holistic well-being.
3. Using Pain Relief with Caution
Those over-the-counter NSAIDs (like ibuprofen) that you might reach for without a second thought can be like a double-edged sword for ulcers, potentially making things worse.
Therefore, it is imperative to avoid self-medicating with these medications if you are experiencing persistent symptoms.
Directly consult your doctor to discuss safer pain management alternatives, such as acetaminophen, which is generally better tolerated by the stomach.
4. The Meal Timing Trick
For individuals with PUD, stomach acid resembles a strong tide. Consuming large meals daily would be indicative of having three large surges of stomach acid.
To trick your stomach into creating lesser acid, aim for gentle, smaller ripples by consuming smaller, more frequent meals. This strategy ensures a more consistent acid level and reduces the likelihood of ulcer irritation.
After eating, give your stomach some time to do its initial work upright before you recline to prevent acid reflux.
Medical Treatments for Peptic Ulcer Disease
There are different types of medications that can help soothe your gut irritation and tackle the root causes. Let’s explore these key players:
1. Proton Pump Inhibitors (PPIs)
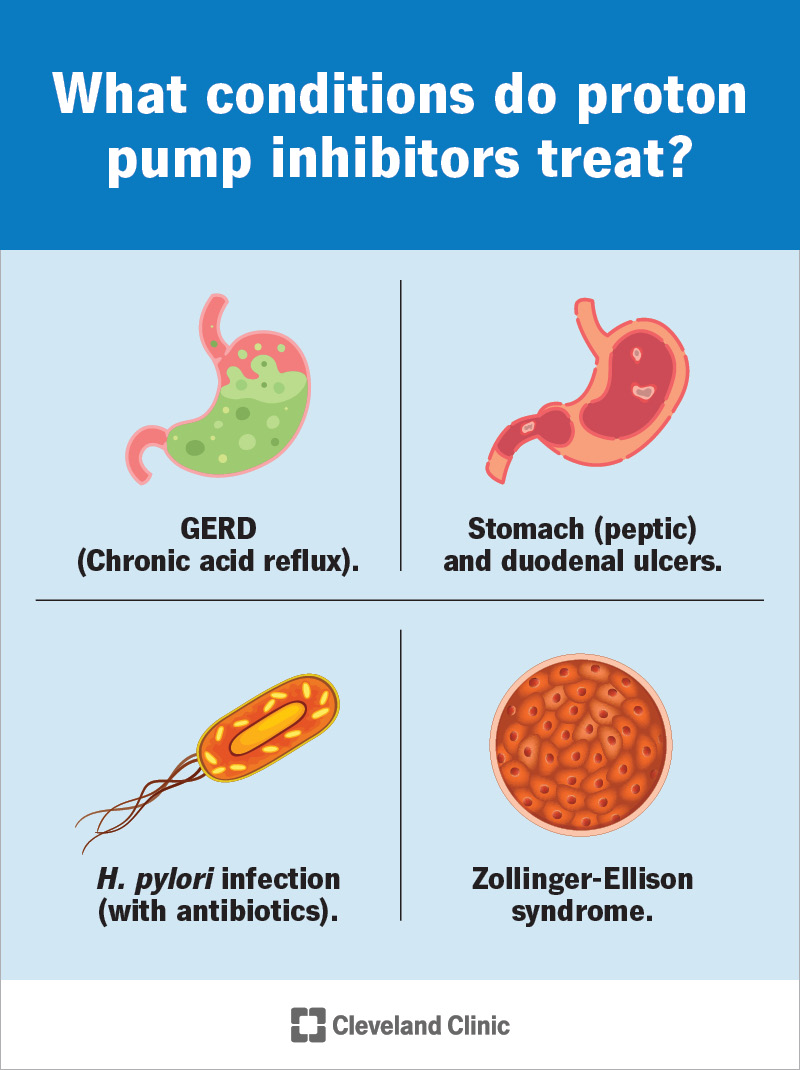
Proton Pump Inhibitors, or PPIs, are often a first-line treatment for many peptic ulcers. They function as master switches that powerfully dial down the activity of tiny pumps that churn stomach acid.
Medications like Nexium (esomeprazole), Prevacid (lansoprazole), and Prilosec (omeprazole) create a less corrosive environment, allowing the ulcer to heal more effectively and preventing further damage.
2. H2-Receptor Blockers
H2-receptors are like messengers that tell your stomach to produce acid.
Medications like H2-receptor blockers, such as famotidine (Pepcid), ranitidine (Zantac), and cimetidine (Tagamet), function contradictingly by blocking these messages to produce lesser stomach acid.
While not as potent as PPIs in reducing acid, they still effectively suppress acid production, providing relief from symptoms and aiding in the healing process. They are often used for milder ulcers or for nighttime acid control.
3. Antibiotics
If the culprit behind your ulcer is the H. pylori bacteria, then antibiotics are your frontline warriors. These medications specifically target and eliminate this infection, which is a major cause of peptic ulcers.
Typically, doctors prescribe a combination of two or three different antibiotics, such as amoxicillin, clarithromycin, and metronidazole, to effectively eradicate the bacteria.
Completing the full course of antibiotics is crucial to prevent the infection from returning and the ulcer from recurring.
4. Antacids
Antacids act as quick firefighters for your stomach acid. These over-the-counter medications contain alkaline substances that directly neutralise stomach acid, providing rapid, though often temporary, relief from heartburn and indigestion associated with ulcers.
Some common examples include Gaviscon, Gastrorelief, and Tum which can be purchased at pharmacies and online retailers.
While they can ease symptoms, they don’t address the underlying cause of the ulcer and are usually used for short-term relief.
5. Cytoprotective Agents
Similar to mucosal protectants, cytoprotective agents help to strengthen the stomach lining’s defenses.
Medications like misoprostol (Cytotec) can help protect the lining from damage caused by NSAIDs by increasing the production of protective mucus and reducing acid secretion.
6. Acetaminophen
For those with peptic ulcers who need pain relief, acetaminophen (Tylenol) is often a preferred choice over NSAIDs. As we discussed earlier, NSAIDs can irritate the stomach lining and hinder ulcer healing.
Acetaminophen provides pain relief without the same risk of exacerbating ulcer symptoms.
Who Should I Consult?

Understanding the intricacies of digestive health can feel overwhelming, but identifying the right specialist is a crucial first step toward effective care.
If you’re experiencing symptoms related to your digestive system, a gastroenterologist is the expert you should consult. These physicians specialise in disorders affecting the esophagus, stomach, intestines, liver, gallbladder, and pancreas.
From managing common issues like acid reflux and irritable bowel syndrome to diagnosing and treating more complex conditions such as peptic ulcer disease, a gastroenterologist possesses the in-depth knowledge and skills to provide comprehensive care.
Meet Island Hospital’s Gastroenterology Specialists
Island Hospital is proud to feature a distinguished team of gastroenterologists, each committed to providing exceptional patient care:
- Dr. Damian Wong Nye Woh
- Dr. Doreen Koay Siew Ching
- Dr. Low Eng Joo
- Dr. Michael Ding Ju Wern
- Dato’ Dr. Robert Ding Pooi Huat
At the heart of Island Hospital’s commitment to digestive health is their state-of-the-art Digestive Centre. This specialised unit offers a comprehensive suite of diagnostic and therapeutic procedures, including essential tools like endoscopy and colonoscopy.
These procedures allow for detailed visualisation of the digestive tract, enabling accurate diagnosis and targeted treatment of conditions such as peptic ulcer disease and other gastrointestinal issues.
Get Proactive Health Insights with Island Hospital’s Executive Health Screening Package

Beyond specialised care, Island Hospital emphasises proactive health management through its comprehensive Executive Health Screening package.
Priced at RM 760.00, this thorough assessment covers a wide range of health indicators, including bone health, diabetes risk, inflammation markers, thyroid function, kidney and liver health, lipid profiles, infection screening, blood and urine analysis, cardiovascular health, vision assessment, and radiological screenings.
This package also includes a physician consultation, with additional tests available upon request.
Find relief from Peptic Ulcer Disease
Take the first step towards a pain-free life.
Explore Island Hospital’s comprehensive digestive health services and find lasting relief from peptic ulcer disease.
For inquiries or to schedule an appointment, please contact us at +604 238 3198/3199 or email us at appt@islandhospital.com.
FAQ
Can peptic ulcers heal on their own?
No, while some individuals might experience temporary relief of symptoms, peptic ulcers are unlikely to heal completely without appropriate medical intervention.
The underlying causes, such as H. pylori infection or the chronic use of nonsteroidal anti-inflammatory drugs (NSAIDs), often persist and can continue to erode the stomach or duodenal lining.
Untreated ulcers can lead to serious complications, including bleeding, perforation (a hole in the stomach or duodenum wall), and obstruction (blockage preventing food from passing through).
Therefore, seeking timely diagnosis and adhering to a prescribed treatment plan are crucial for healing and preventing these potentially life-threatening issues.
Can peptic ulcers come back after treatment?
Yes, unfortunately, there is a risk of peptic ulcer recurrence even after successful treatment. Several factors can contribute to this. If the initial cause, such as an H. pylori infection, was not completely eradicated, the ulcer can certainly return.
Additionally, continued use of NSAIDs, smoking, and potentially even high stress levels in some individuals can increase the likelihood of recurrence.
To minimise this risk, it’s essential to follow your doctor’s recommendations regarding lifestyle modifications and long-term management strategies, especially if you have a history of recurrent ulcers.
In some cases, maintenance therapy with acid-suppressing medications might be considered.
How long does it take for a peptic ulcer to heal with treatment?
With consistent adherence to the prescribed treatment plan, which typically involves medications to reduce stomach acid and antibiotics to eradicate H. pylori if present, you should start to experience a noticeable improvement in your symptoms within a few weeks.
However, complete healing of the ulcer crater itself takes more time which is anywhere from 1 to 3 months for the ulcer to fully heal, depending on its size, location, and the individual’s overall health.
It’s vital to continue taking your medication for the entire duration prescribed by your doctor, even if you feel better, to ensure complete healing and reduce the risk of recurrence. Follow-up appointments or endoscopic examinations might be necessary to confirm complete healing.
Are peptic ulcers contagious?
Peptic ulcers themselves are not contagious but H. pylori, can be transmitted from person to person. The exact mode of transmission isn’t fully understood, but it’s believed to occur through direct contact with saliva, vomit, or fecal matter.
This can happen through close personal contact, such as kissing, or through contaminated food or water, although this is less common in developed countries with good sanitation.
Can children or teens get peptic ulcers?
Yes, although peptic ulcers are more common in adults, children and teenagers can also develop them. The causes in this age group can be similar to those in adults, including H. pylori infection, NSAID use, and, less commonly, stress or underlying medical conditions.
Symptoms in children and teens might be less typical than in adults, sometimes presenting as recurrent abdominal pain, nausea, vomiting, or poor appetite.






