
15 Nov Glaucoma vs. Cataracts: Which Eye Condition Are You At Risk For?
Glaucoma vs. Cataracts: Which Eye Condition Are You At Risk For?
By Island Hospital | November 15, 2024 12:00:00 PM
Medical Reviewer: Dr. Vanessa Naseem Neoh, Ophthalmologist
Glaucoma and cataracts are two prevalent eye conditions that can significantly impair vision and are major contributors to global blindness.
Although many people are aware of these degenerative eye conditions, they often lack a clear understanding of their differences and the potential consequences of neglecting treatment and effective management.
In this article, we will delve into the details of glaucoma and cataracts, exploring their causes, symptoms, and treatment options.
By the end, you’ll gain a clearer understanding of these conditions and be better equipped to protect your eye health.
What is Glaucoma?
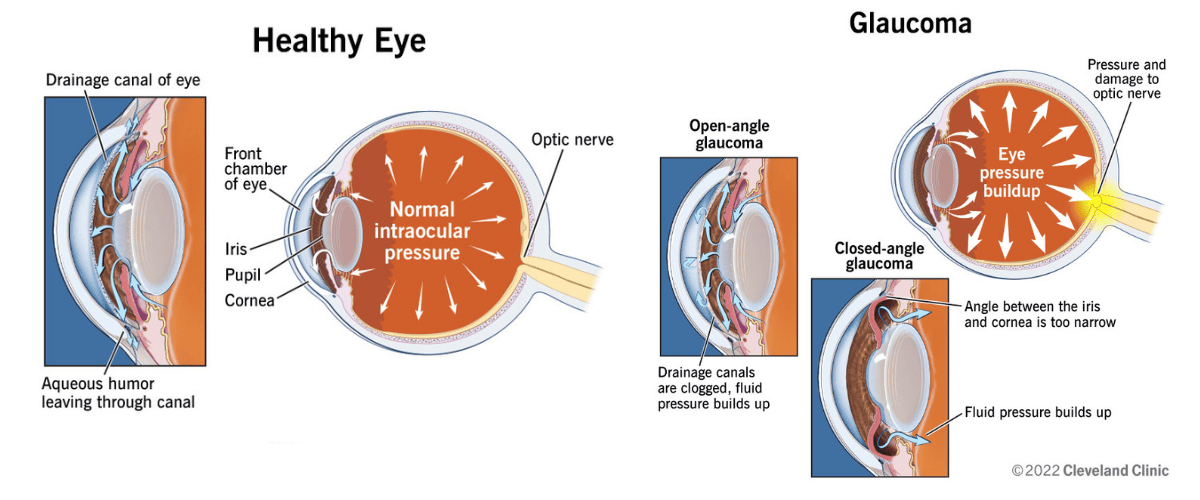
Photo by Cleveland Clinic
Glaucoma occurs when there is excessive pressure (intraocular pressure) within your eye. This pressure buildup happens when your eye’s natural fluid (aqueous humour) does not drain properly.
Usually, old fluid drains through a specific meshwork and a tiny opening. If these drainage pathways become blocked, pressure builds up. This increased pressure can potentially damage the optic nerve and lead to vision loss.
There are several types of glaucoma, which include:
- Acute angle-closure glaucoma
A less frequent type caused by a sudden blockage in the eye’s angle, leading to a rapid rise in pressure. - Congenital glaucoma (childhood glaucoma)
A rare condition present from birth, caused by an abnormality in the eye’s structure. - Primary open-angle glaucoma (POAG)
The most common type, gradually developing due to clogged drainage channels in the eye. - Secondary glaucoma
Develops as a result of an underlying condition, such as inflammation, diabetes, surgery, or steroid use.
Glaucoma is the second most common cause of blindness worldwide, following cataracts.
What is a Cataract?
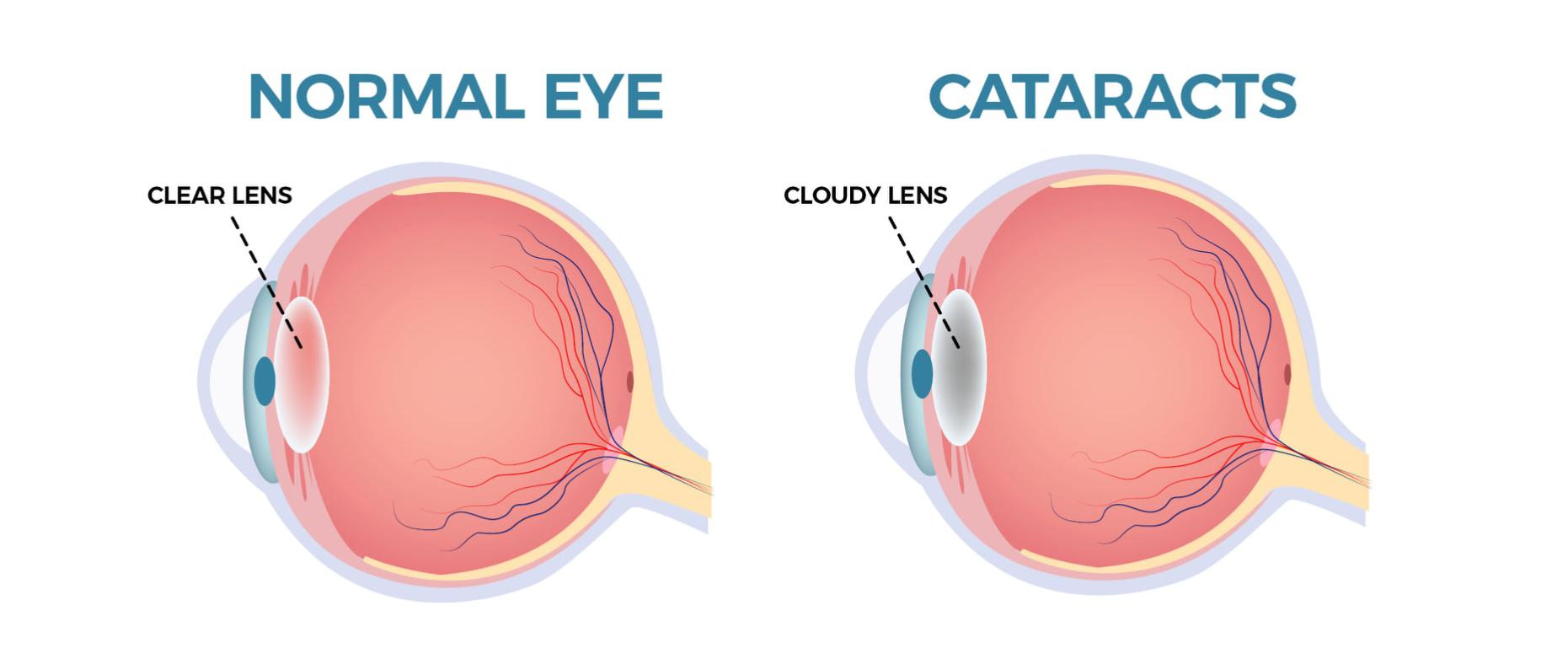
Cataracts are common, occurring when the eye lens becomes clouded with proteins that gradually grow larger over time, causing blurred or hazy vision.
While cataracts typically affect older individuals, they can occur at any age. The condition can develop in one or both eyes, but only one cataract can form per eye.
These visual impairments can significantly impact daily activities, such as reading.
Symptoms of Glaucoma and Cataract
Glaucoma Symptoms
Glaucoma can be completely asymptomatic in its early stages. However, typical symptoms include:
- Gradual loss of peripheral vision – often noticed as a “tunnel vision” effect.
- Eye pain (in cases of closed-angle glaucoma)
- Eye redness
- Headache
- Nausea or vomiting (in cases of acute angle-closure glaucoma)
- Blind spots or patches (in cases of open-angle glaucoma)
Cataract Symptoms
Common symptoms of cataracts include:
- Sensitivity to light
- Glare from headlights or sunlight
- Double vision
- Fading colours
- Frequent changes in eyeglass prescriptions
It’s important to note that early symptoms of glaucoma and cataracts can be subtle and may not be immediately noticeable.
Should you experience any of these symptoms, it is important to schedule a comprehensive eye exam with an ophthalmologist. Early detection and treatment can help prevent significant vision loss.
Unsure if you need to see an ophthalmologist? Check out our article on choosing the right eye specialist.
Risk Factors of Glaucoma and Cataracts
Understanding the risk factors for glaucoma and cataracts is crucial for preventative measures. By understanding these risk factors, you can take proactive steps to safeguard your vision.
Glaucoma Risk Factors
Here are the key factors which may increase your risk of glaucoma:
- Age: The risk of glaucoma increases with age, particularly after 40.
- Family History: A family history of glaucoma, especially open-angle glaucoma, significantly increases the risk.
- Race and Ethnicity: African Americans, Hispanics, and Asians have a higher risk of developing glaucoma.
- Eye Anatomy: People with thin corneas or large eyes may be at a higher risk.
- Certain Health Conditions: Poorly controlled high blood pressure and diabetes can cause glaucoma.
- Corticosteroid Use: Long-term use of corticosteroids, either as eye drops or oral medications, can increase the risk of glaucoma.
Cataracts Risk Factors
Here are the key factors which may increase your risk of cataracts:
- Age: The most significant risk factor for cataracts is age. As people get older, the lens of the eye naturally becomes clouded.
- Smoking: Smoking can accelerate the development of cataracts.
- Ultraviolet (UV) Radiation Exposure: Excessive exposure to UV radiation from sunlight can contribute to cataract formation.
- Eye Injuries: Injuries to the eye can increase the risk of developing cataracts later in life.
- Certain Health Conditions: Diabetes can increase the risk of cataracts and may also cause them to develop at a younger age.
- Corticosteroid Use: Long-term use of corticosteroids can increase the risk of cataracts.
By being aware of these risk factors and scheduling regular eye exams, you can help reduce the risk of developing glaucoma or cataracts and preserve your vision.
Don’t be misled: Learn the facts about glaucoma and debunk common myths by reading our comprehensive article, “The Most Common Myths Surrounding Glaucoma.“
Glaucoma vs. Cataracts: Similarities and Differences
Similarities
While glaucoma and cataracts have distinct causes and treatments, they can sometimes share similar symptoms such as blurred vision, halos around lights, and poor night vision.
Early detection and proactive management are also crucial for both glaucoma and cataracts.
To prevent vision loss with glaucoma, timely diagnosis is crucial. Early detection of cataracts enables monitoring and ensures timely surgery.
If left untreated, both conditions can lead to blindness.
Differences
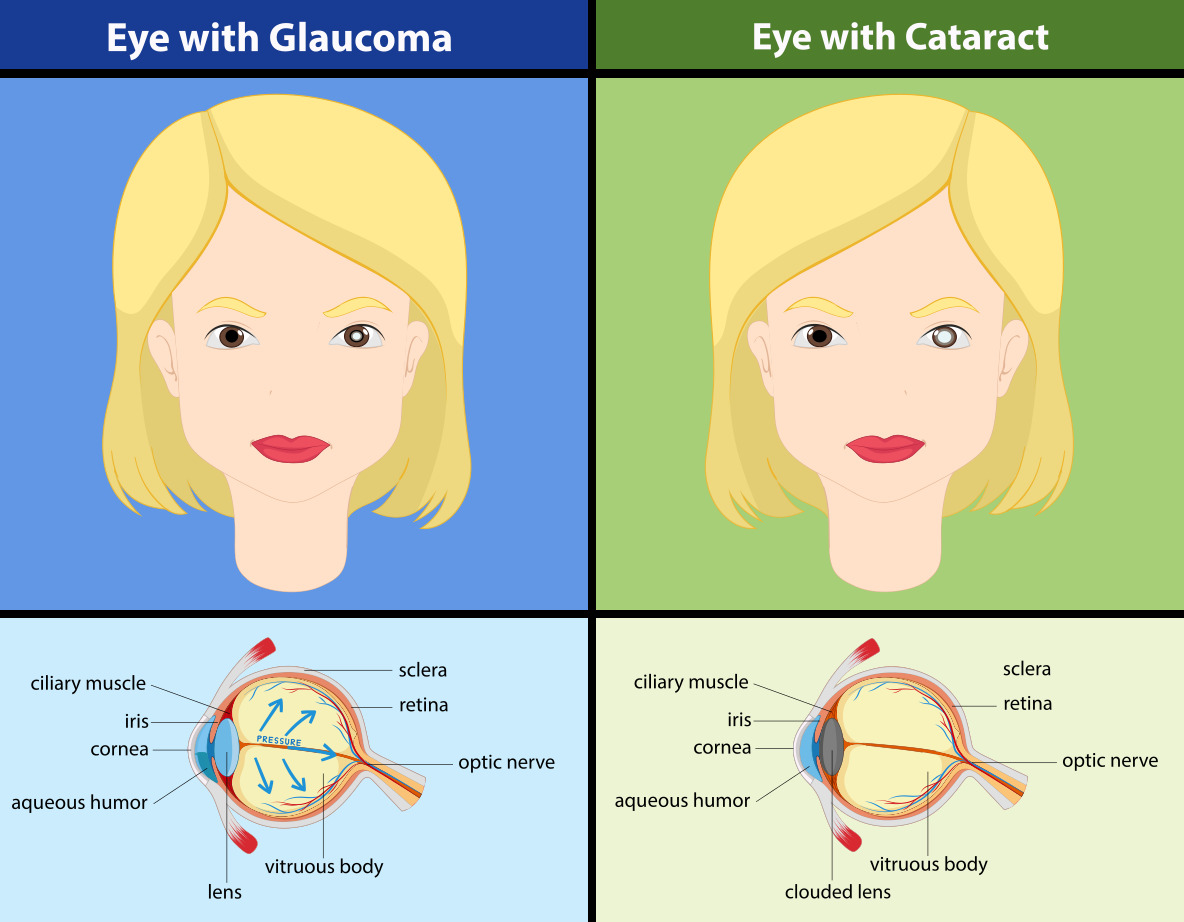
Photo by Freepik
While surgery is a common treatment for both, it’s the only option for cataracts, whereas glaucoma has multiple treatment possibilities.
| Affected area | ||
| Treatment and Reversibility | ||
| Surgical Procedures | ||
| Disease Progression | ||
| Urgency of Treatment |
Can Glaucoma Cause Cataracts (or Vice Versa)?
Glaucoma and cataracts can often coexist, and in some cases, one condition can contribute to the development of the other. A large cataract may obstruct the eye’s drainage system, increasing pressure.
While glaucoma does not cause cataracts, specific treatments, such as tube shunt surgery, trabeculectomy, or specific medications, may accelerate cataract formation.
Studies indicate that these interventions can contribute to the more rapid development of cataracts.
Treatment for Glaucoma and Cataract
Glaucoma Treatment
Glaucoma treatment aims to halt vision deterioration and may involve:
- Prescription eye drops
To lower intraocular pressure. - Oral medications
Such as carbonic anhydrase inhibitors (e.g., acetazolamide). - Laser therapy
Including selective laser trabeculoplasty (SLT) to improve drainage, peripheral iridotomy (PI) to unblock drainage channels, or cyclophotocoagulation to reduce fluid production. - Glaucoma surgery
To create a new drainage pathway or enhance the function of existing channels. Common procedures include trabeculectomy, aqueous shunt tube, PreserfFlo MicroShunt, ECP laser, and suprachoroidal shunts.
Additionally, cataract formation is common after glaucoma surgery. It is best to wait 1 to 2 years following certain glaucoma procedures to stabilise the eye before cataract surgery.
Cataracts Treatment
Cataracts can be identified during a routine eye exam through a simple dilation test. Your doctor will administer eye drops to dilate your pupil, allowing for a clearer view of the lens.
If your cataracts are small, adjusting your prescription may be sufficient. However, advanced cataracts may require surgical intervention.
Cataract surgery is a widely performed procedure involving the replacement of your clouded lens with artificial ones. There are different choices of lens implants, including:
- Extended depth of focus lenses
- Monofocal lenses
- Multifocal lenses
- Toric lenses
Reduce your risk of vision loss through treatment. Our article on Diabetic Retinopathy provides detailed information on this essential preventive measure.
Protect Your Vision Now!
Glaucoma and cataracts can both lead to permanent visual impairment if not diagnosed and treated early.
To keep your eyes healthy and your vision clear, especially as you get older, it is important to have regular eye exams to ensure that glaucoma or cataracts are detected early.
At Island Hospital, our ophthalmology department features a team of internationally recognized ophthalmologists dedicated to providing exceptional eye care for visual impairments, conditions, and diseases.
Our commitment to excellence in advanced diagnostics, cutting-edge therapies, and compassionate support has earned us local and worldwide recognition:
A finalist for Malaysia’s Flagship Medical Tourism Hospital Programme
A place on Newsweek’s list of World’s Best Hospitals 2024
A place Global Health Asia Pacific Awards 2024
Time is of the essence when it comes to eye health. Don’t wait for symptoms to worsen. Book your eye exam with us today to learn more about our treatment options.
FAQ
How to prevent glaucoma and cataracts?
There is no guaranteed way to prevent glaucoma or cataracts. However, adopting certain lifestyle habits and seeking regular eye care can significantly reduce your risk:
Even if you have no symptoms, it's crucial to have regular eye exams, especially as you age. Early detection of glaucoma can help prevent vision loss. Prolonged use of corticosteroids can increase the risk of glaucoma. Discuss the potential risks with your doctor if you need to use them. If you have diabetes, high blood pressure, or other health conditions that increase your risk of glaucoma, work with your doctor to manage them effectively. | Wear sunglasses with UV protection and a wide-brimmed hat to shield your eyes from harmful UV rays. Prolonged use of corticosteroids may increase your chances of getting cataracts. Smoking can accelerate the development of cataracts. Diabetes and high blood pressure can increase the risk of cataracts. |
While these lifestyle changes can help reduce your risk, they may not entirely eliminate it. Regular eye exams remain crucial for early detection and treatment of both glaucoma and cataracts.
Is glaucoma or cataract more serious?
Both glaucoma and cataracts can lead to severe vision loss if left untreated. However, the severity of each condition can vary depending on individual factors and the stage of the disease. Here’s a quick rundown of each condition:
- Glaucoma poses a more serious threat as it can irreversibly damage the optic nerve, resulting in blindness. If not detected and treated early, glaucoma can progress rapidly and cause significant vision loss.
- Cataracts, while not typically as urgent, can also significantly impair vision if left untreated. However, they are generally treatable with surgery, which can often restore vision.
Can I have cataract surgery if I have glaucoma?
Although individual cases may vary, cataract surgery is generally considered safe for those with glaucoma. However, there’s evidence suggesting that cataract surgery can temporarily elevate intraocular pressure. Therefore, individuals with glaucoma may opt to undergo both procedures simultaneously.
Does glaucoma go away after cataract surgery?
No, glaucoma does not go away after cataract surgery. While cataract surgery can improve vision by replacing the cloudy lens, it does not address the underlying cause of glaucoma, which is increased intraocular pressure.
Is it possible to combine glaucoma surgery and cataract surgery?
If you suffer from both glaucoma and cataracts, it is best to consider treating them concurrently.This can help prevent further vision loss and reduce the need for multiple surgeries.
Your ophthalmologist will be able to advise you on the best treatment course based on your situation.
Related Doctors
| Derived from | Complications |
|---|






