
09 Feb Arthroscopy (Keyhole Surgery): Why It’s the Preferred Minimally Invasive Surgery
Arthroscopy (Keyhole Surgery): Why It’s the Preferred Minimally Invasive Surgery
By Island Hospital | 28 January 2026. 12:00:00 PM
If you’ve been told you might need arthroscopy, you’ve likely heard it described as “minimally invasive” or “simple keyhole surgery.”
As the name suggests, arthroscopy allows a surgeon to look inside a joint and treat certain problems through very small incisions that are often no bigger than a keyhole, using a tiny camera and specialised instruments.
For the right condition, this approach can be highly effective. But arthroscopy is not a universal solution for joint pain, and its success depends greatly on why it’s being done, which joint is involved, and what’s actually causing the problem.
This guide goes beyond the generic descriptions to explain what arthroscopy really does, who is most likely to benefit, when it may not help (or may not be necessary), and what recovery is like.
What Is Arthroscopy?
Arthroscopy is a surgical procedure where a surgeon inserts a small camera (arthroscope) into a joint through tiny incisions. The camera projects images onto a screen, allowing the surgeon to assess joint damage and, if needed, treat the problem using specialised instruments.
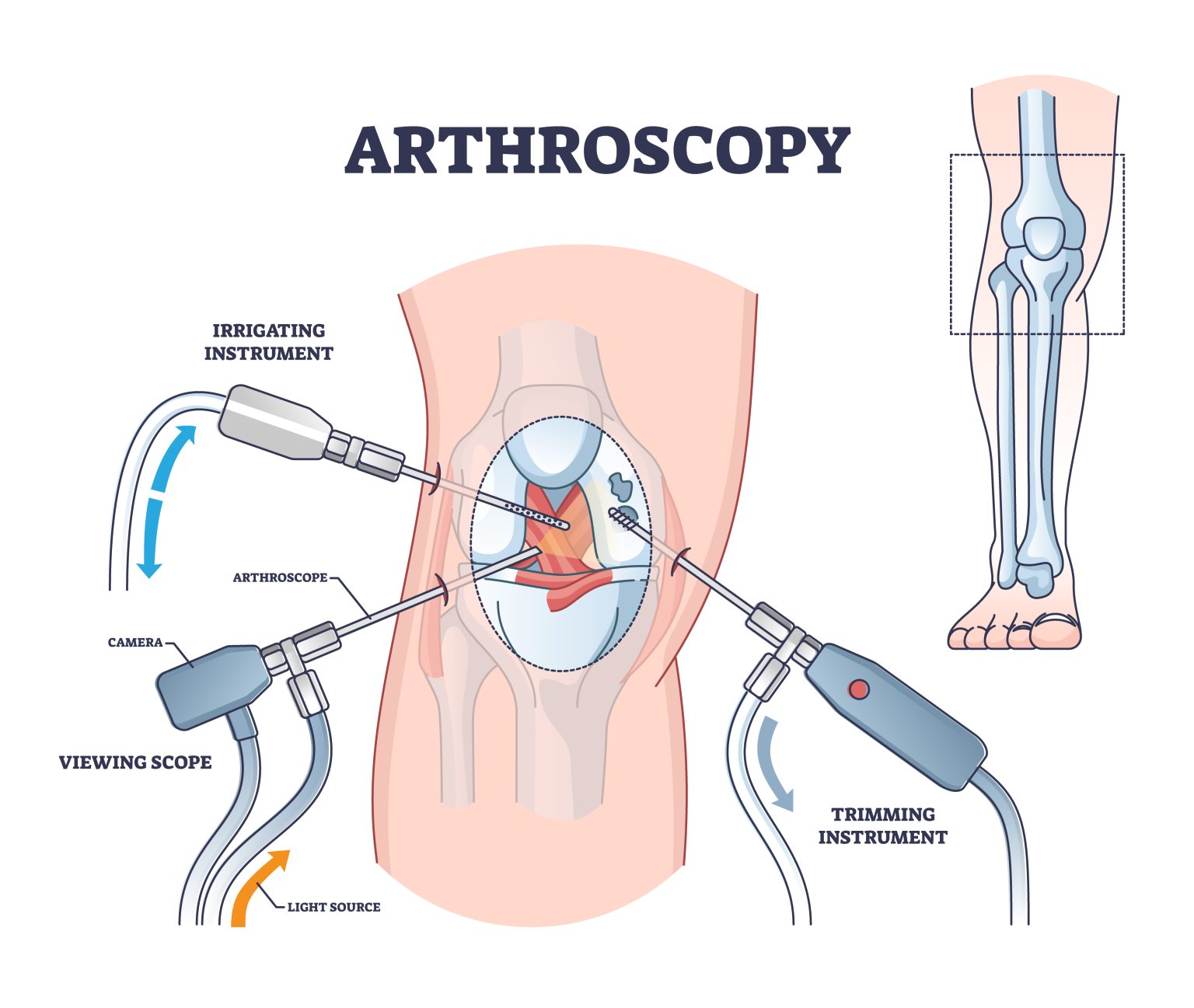
Arthroscopy is a surgical procedure where a surgeon inserts a small camera (arthroscope) into a joint through tiny incisions. The camera projects images onto a screen, allowing the surgeon to assess joint damage and, if needed, treat the problem using specialised instruments.
Which Joints Can Be Treated With Arthroscopy?
Arthroscopy can be performed on several joints, but outcomes and recovery differ depending on the joint involved.
Common joints treated with arthroscopy
- Knee (most common)
- Shoulder
- Ankle
- Hip
- Wrist and elbow (less common)
Why recovery differs by joint
Weight-bearing joints (like the knee and ankle) tend to have:
- More post-operative swelling
- Longer rehab timelines
- Greater impact on daily activities
Non-weight-bearing joints (like the shoulder) often allow earlier movement but require longer physiotherapy for strength and control.
Conditions Arthroscopy Can Help vs When It Can’t
Arthroscopy can be highly effective for certain joint problems but it isn’t always the answer for pain or stiffness.
Knowing which conditions respond best to this minimally invasive procedure helps patients make informed decisions and avoid unnecessary surgery:
| Condition or Problem | When Arthroscopy Is Often Helpful | When Arthroscopy Is Unlikely to Help |
| Meniscus tears | Traumatic or well-defined tears causing locking, catching, or giving way, especially after injury | Degenerative or age-related tears without mechanical symptoms |
| Loose bone or cartilage fragments | Free-floating pieces causing sudden pain, locking, or joint blockage | Diffuse cartilage wear without loose fragments |
| Cartilage damage | Isolated cartilage flaps or focal defects that can be trimmed or stabilised | Widespread cartilage thinning from osteoarthritis |
| Ligament-related impingement | Specific ligament tissue causing pinching or restricted movement | General ligament degeneration without clear impingement |
| Joint instability | Instability from specific injuries (e.g. sports trauma) with a clear structural cause | Instability related to muscle weakness or poor joint control |
| Unexplained joint pain | Pain with a clear mechanical cause confirmed by examination and symptoms | Generalized pain without locking, catching, or mechanical signs |
| Osteoarthritis | Very limited role in early, selected cases with mechanical symptoms | Advanced osteoarthritis with widespread joint degeneration |
For many degenerative conditions such as osteoarthritis or degenerative meniscus tears, physiotherapy and structured rehabilitation often provide outcomes similar to surgery, without the risks associated with an operation.
| Why selection matters:
Arthroscopy works best when there is a physical obstruction or structural defect that can be directly corrected. When pain comes from degeneration, inflammation, or wear-and-tear changes, surgery is far less effective. |
Not All Arthroscopies Are the Same (Why Outcomes Vary)
One common misconception among patients is that all arthroscopic surgeries are the same but they’re not.
The type of procedure, the tissues involved, and the recovery plan all influence the outcome.
Here’s a breakdown to help you understand these differences and set realistic expectations:
Common Arthroscopic Procedures
| Procedure | What It Involves | Recovery & Considerations |
| Meniscus trimming (meniscectomy) | Damaged meniscus tissue is removed | Recovery is usually faster, but removing tissue can slightly increase long-term risk of arthritis |
| Meniscus repair | Torn meniscus is stitched back together | Preserves tissue and long-term joint health, but rehab is longer and requires careful adherence |
| Cartilage smoothing (chondroplasty) | Rough or damaged cartilage is shaved to reduce irritation | Can relieve symptoms, but it does not restore cartilage |
| Microfracture | Tiny holes are made in the bone to stimulate new cartilage growth | Can help regrow cartilage, but requires strict rehabilitation and limited weight-bearing |
| Joint lavage (washing the joint) | Joint is flushed to remove debris | Limited benefits for arthritis; generally only provides short-term relief |
Why This Matters
Two people can have “knee arthroscopy” and experience very different outcomes depending on:
- The exact procedure performed
- The quality of the tissue being treated
- How closely rehabilitation instructions are followed
________________________________________________________________________
For individuals who have recently undergone knee surgery, rehabilitation is a crucial step towards full recovery. Find out how in: Knee Surgery Rehabilitation: Tips for a Successful Recovery.
________________________________________________________________
What Happens During Arthroscopy Surgery?
Arthroscopy is a minimally invasive procedure that allows surgeons to see inside a joint and treat certain problems without making large incisions. Here’s what you can expect:
Before Surgery
- Your surgery will be performed under general anaesthesia (you are fully asleep) or regional anaesthesia (numbed from the waist or limb down).
- Your surgeon will review the joint problem, MRI findings, and goals of the surgery.
- Consent discussions are critical at this stage because what the surgeon finds during arthroscopy may differ from imaging.
During Surgery
- Small incisions (usually 2–3, each about the size of a keyhole) are made around the joint.
- A tiny camera (arthroscope) is inserted, projecting the joint interior onto a screen.
- Special surgical instruments are introduced through other small incisions to:
- Remove or repair damaged tissue (e.g., meniscus tears, loose fragments)
- Smooth cartilage or stimulate healing (e.g., microfracture)
- Address ligament or tendon issues causing impingement
- Surgery is usually quick where it takes about 30–90 minutes, depending on the joint and procedure.
After Surgery
- Most patients go home the same day, though some may stay overnight if needed
- Small wounds are dressed, and crutches or support devices may be provided
Surgeons often provide detailed post-op instructions, including wound care, pain management, and rehab exercises
Arthroscopy vs Non-Surgical Treatment
1. When Non-Surgical Treatment Should Come First
For many joint problems—especially degenerative conditions—non-surgical approaches are usually tried first. These include:
- Structured physiotherapy to strengthen muscles, improve mobility, and reduce strain on the joint
- Activity modification to avoid movements that worsen symptoms
- Weight management to reduce pressure on weight-bearing joints
- Short-term pain relief or injections to manage discomfort while other treatments take effect
These strategies can often significantly reduce pain and improve function without exposing you to the risks of surgery.
2. When Arthroscopy May Be Reasonable
Surgery may be considered if:
- Mechanical symptoms persist, such as locking, catching, or giving way
- Conservative treatment has failed despite adequate time and effort
- Daily function is significantly affected, limiting work, exercise, or everyday activities
- Imaging findings correspond with symptoms, confirming a treatable structural problem
What Arthroscopy Recovery is Like
Recovery after arthroscopy is gradual and unique to each person. Use this checklist to track what you might experience at each stage:
1. First Week After Surgery
- Keep the surgical site clean and protected
- Expect swelling and stiffness around the joint
- Pain levels vary depending on the procedure
- You may need crutches temporarily for support
2. Weeks 2–6
- Follow your rehab exercises consistently for best results
- Attend physiotherapy sessions focused on motion and strength
- Desk work or light activity may be possible earlier than physically demanding jobs
- Swelling may persist longer than expected—this is normal
3. 2 to 3 Months and Beyond
-
- Gradually return to sports or high-impact activity under guidance
- Kneeling or squatting may still feel uncomfortable
- Some symptoms, like mild swelling or stiffness, can linger even with good recovery
- Remember: Recovery is not linear and temporary setbacks are common and normal
| Use this checklist as a guide, but always follow your surgeon or physiotherapist’s instructions as everyone heals differently. |
Risks, Complications & Why Pain Sometimes Persists
Even though arthroscopy is generally safe, all surgeries carry some risks. Being aware of them helps you set realistic expectations.
| Category | Details | What It Means For You |
|---|---|---|
| Common Risks | Swelling | Normal after surgery; may last a few weeks |
| Stiffness | Temporary limitation in joint motion is common | |
| Infection | Rare, but watch for redness, warmth, or fever | |
| Less Common but Important Risks | Blood clots | Uncommon but potentially serious; follow prevention advice |
| Nerve irritation | Tingling, numbness, or temporary weakness may occur | |
| No improvement in symptoms | Surgery may not relieve pain as expected | |
| Why Arthroscopy Sometimes Doesn’t “Work” | Surgery fixed what was seen on imaging | The main source of pain may be elsewhere |
| Degenerative joint disease continues | Arthritis or wear-and-tear may progress despite surgery | |
| Insufficient rehabilitation | Recovery may be limited if exercises are not followed |
_______________________________________________________________________
Having persistent joint pain or mobility issues? Stay informed on how to bid farewell to Bunion pain in Island Hospital’s guide to surgery options and smooth recovery.
________________________________________________________________________
Explore Your Arthroscopy Options with a Trusted Specialist
Arthroscopy can be an effective procedure for diagnosing and treating certain joint conditions. However, as with any medical procedure, it is important to fully understand its benefits, risks, and whether it is the most suitable option for your specific condition.
Every joint, every condition, and every person is different. This is why consulting a specialist can make all the difference. In some cases, obtaining a second opinion may also help you feel more confident about your treatment plan.
Discuss anything from your symptoms, lifestyle, and treatment goals with Island Hospital’s qualified surgeons, and let us help you take the first step toward a healthier, more active life.
Explore your options and find the care that’s tailored to you. Consult with our healthcare professional today!
FAQs
1. Is arthroscopy painful?
Some discomfort is normal after arthroscopy, particularly in the first few days to a week. Pain levels depend on the joint involved, the type of procedure, and your individual pain tolerance.
Surgeons usually prescribe pain relief medication, and following rehabilitation exercises can help reduce stiffness and discomfort. Most patients find the pain manageable and improve steadily after the first week.
2. How long does swelling last after arthroscopy?
Swelling is common and can last from a few weeks to several months, depending on factors like:
- The joint treated (knees and ankles may swell longer than shoulders)
- The extent of the procedure
- Your activity level and adherence to rehab protocols
Elevating the joint, using ice packs, and wearing compression wraps can help reduce swelling faster. Mild swelling may persist for months, even after full recovery.
3. Can arthroscopy fail?
Yes. Arthroscopy can sometimes fail to relieve pain or improve function, especially if the underlying issue is degenerative rather than mechanical. Common reasons for limited improvement include:
- Arthritis or widespread cartilage wear
- Incomplete rehabilitation
- Symptoms originating from a different part of the joint or surrounding structures
Understanding the cause of your joint problem and following a structured recovery plan improves the likelihood of a successful outcome.
4. When can I drive after arthroscopy?
Driving depends on which leg or joint was treated and your comfort level:
- For procedures on a non-driving leg, most patients can drive after 1–2 weeks
- If the driving leg is involved, you may need longer (often 2–4 weeks) until you can safely control the vehicle and react in an emergency
Always check with your surgeon and your insurance guidelines before resuming driving.
5. How long does it take to fully recover from arthroscopy?
Full recovery after arthroscopy varies depending on the joint treated, type of procedure, and individual factors.
- Knee or ankle arthroscopy: Most patients regain daily activities within 4–6 weeks, but full return to sports or high-impact activity can take 2–3 months.
- Shoulder or hip arthroscopy: Recovery may take 6–12 weeks for everyday activities, with 3–6 months for full strength and mobility.
- Recovery is not always linear—temporary setbacks like swelling or stiffness are common.
- Following rehabilitation exercises and physiotherapy as recommended is crucial for the best outcomes.






