
25 Jan Heartburn, Acid Reflux, or GERD: What’s the Difference?
Heartburn, Acid Reflux, or GERD: What’s the Difference?
By Island Hospital | Jan 25, 2026 12:00:00 PM
Heartburn, acid reflux, and GERD are often confused, but they are distinct conditions that separates one from the other. Occasional discomfort after a heavy meal is common, but frequent or severe symptoms may indicate a serious digestive problem that requires medical attention.
This guide explains the difference between heartburn, acid reflux, and GERD, when to see a doctor, how GERD is diagnosed, and practical ways to manage symptoms — including home remedies, dietary tips, and medical treatment options available at Island Hospital (IH).
Heartburn vs Acid Reflux vs GERD: What’s the Difference?
Many people use the terms “heartburn”, “acid reflux”, and “GERD” interchangeably, but they refer to different concepts.
Understanding the distinctions is key to helping you understand what it is and to managing symptoms effectively.
1. Acid Reflux
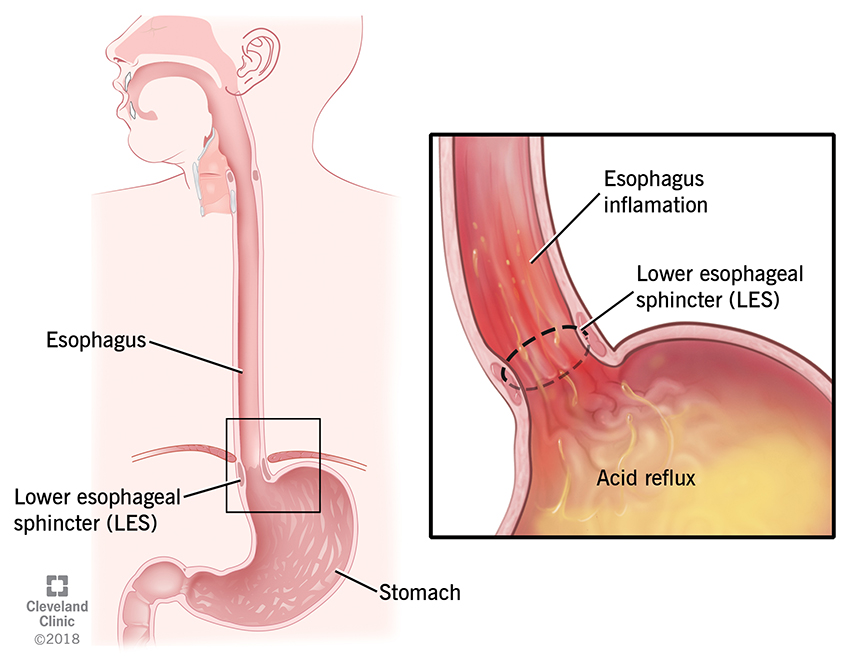
Acid reflux is the process when stomach acid flows backward into the esophagus due to a weakened lower esophageal sphincter (LES).
Some common triggers leading to this condition include:
- Large or fatty meals
- Spicy foods
- Alcohol or caffeine
- Lying down soon after eating
- Stress or obesity
Occasional acid reflux is common and usually manageable with lifestyle changes, such as avoiding trigger foods or eating smaller meals.
2. Heartburn
Heartburn is a symptom, not a disease. It is experienced as a burning sensation in the chest or throat when stomach acid irritates the lining of the esophagus (acid reflux).
However:
- Not everyone with acid reflux experiences heartburn.
- Not all heartburn indicates GERD.
- Symptoms may include a sour taste in the mouth, chest discomfort, or a feeling of food “sticking” in the throat.
3. GERD (Gastroesophageal Reflux Disease)
GERD is a chronic, more severe form of acid reflux. It is typically diagnosed when acid reflux occurs twice or more per week or when it significantly impacts daily life.
Potential complications if left untreated include:
- Inflammation of the esophagus (esophagitis)
- Ulcers or erosions in the esophagus
- Narrowing of the esophagus (stricture)
- In rare cases, increased risk of esophageal cancer
GERD often requires medical evaluation and may be managed with medications, lifestyle modifications, or in some cases, surgical interventions.
In summary:
| Condition | What It Is | How Often | Severity |
|---|---|---|---|
| Acid Reflux | Backflow of stomach acid | Occasional | Mild |
| Heartburn | Burning chest sensation | Occasional | Symptom only |
| GERD | Chronic acid reflux disease | Frequent | Moderate–Severe |
When You Should See a Doctor for Acid Reflux
While occasional acid reflux is common, persistent or severe symptoms may indicate a more serious condition. Seek medical attention if you experience any of the following:
| Persistent reflux lasting more than 2 weeks despite lifestyle changes. |
|
| Difficulty swallowing or a sensation of food getting “stuck” in your throat. |
|
| Chest pain that is unrelated to heart problems. |
|
| Chronic cough, hoarseness, or throat irritation. |
|
| Vomiting or vomiting blood. |
|
| Unexplained weight loss. |
|
| Nighttime choking or frequent awakening due to reflux. |
|
| Frequent reliance on antacids or prescription medications (PPIs). |
These symptoms could signal GERD or other serious conditions, so prompt evaluation by a healthcare professional is important.
Symptoms of Severe GERD
GERD can range from mild to severe. When its severity develops, it often involves persistent or worsening symptoms that can affect your daily life.
These are the common symptoms of severe GERD you should take note of:
- Frequent heartburn: A burning sensation in the chest or throat that occurs regularly, often after meals or when lying down.
- Acid regurgitation: Stomach acid or partially digested food flowing back into the mouth, causing discomfort or a sour taste.
- Bitter or sour taste: A lingering unpleasant taste in the mouth, often due to acid reflux reaching the throat or mouth.
- Bloating and fullness: Feeling uncomfortably full after meals or experiencing abdominal pressure.
- Chest discomfort: Pain or pressure in the chest that may mimic heart-related symptoms, though it is caused by acid irritating the esophagus.
- Difficulty swallowing (dysphagia): Feeling that food is sticking in the throat or chest, which may indicate inflammation or narrowing of the esophagus.
Additional signs of severe GERD can also include:
- Chronic cough
- Hoarseness
- Sore throat
- Frequent nighttime symptoms that disrupt sleep
Persistent or worsening symptoms should prompt evaluation by a healthcare professional to prevent complications.
Possible Long-Term Complications
It is important to check any of these common and atypical symptoms to avoid possible long-term complications that may endanger your life.
Because untreated GERD can lead to:
- Esophagitis (inflammation)
- Esophageal ulcers
- Narrowing of the esophagus (strictures)
- Barrett’s esophagus
Increased cancer risk such as oesophagus cancer and stomach cancer (rare but serious)
Discover how robotic surgery is transforming GERD treatment and offering long-term relief from chronic acid reflux. Read the full article here to learn how this innovative approach could help you.
How to Stop Acid Reflux at Night
Nighttime acid reflux can interfere with sleep, leaving you uncomfortable and fatigued the next day. To reduce symptoms and promote better rest, try the following strategies:
- Elevate the head of the bed by 10–20 cm: Raising your upper body helps prevent stomach acid from flowing back into the esophagus while you sleep.
- Sleep on your left side: This position reduces pressure on the stomach and may decrease nighttime reflux.
- Avoid meals 2–3 hours before bedtime: Giving your stomach time to empty can minimise the risk of acid backing up while lying down.
- Limit caffeine, chocolate, and alcohol: These can relax the lower esophageal sphincter, making reflux more likely.
- Wear loose clothing: Tight garments around the waist can increase abdominal pressure and trigger reflux.
- Eat smaller, earlier dinners: Lighter meals reduce the amount of stomach acid needed for digestion and help prevent nighttime discomfort.
Implementing these simple changes can significantly reduce nighttime reflux and improve overall sleep quality.
Home Remedies for Heartburn
Managing heartburn at home involves both short-term relief for immediate discomfort and long-term habits to prevent recurrence. Here’s how!
Short-Term Relief:
- Warm water: Helps neutralise stomach acid and soothe the esophagus.
- Sugar-free gum: Chewing stimulates saliva production, which can help wash acid back down into the stomach.
- Ginger tea: Known for its anti-inflammatory properties, it can calm the digestive tract.
- Chamomile tea: May reduce inflammation and promote relaxation, easing heartburn symptoms.
- ⚠️ Baking soda: Can provide quick relief by neutralising acid, but should only be used occasionally and not as a long-term solution.
Long-Term Preventive Habits:
- Maintain a healthy weight: Excess weight can increase pressure on the stomach, worsening reflux.
- Avoid overeating and eat slowly: Smaller, mindful meals reduce the chance of acid backflow.
- Manage stress: Stress can trigger digestive issues and exacerbate heartburn.
- Stay hydrated and exercise regularly: Support overall digestive health and prevent bloating or reflux.
- Avoid over-reliance on antacids or long-term medications without consulting a doctor, as this may mask underlying issues.
Incorporating these strategies can help reduce heartburn frequency and improve overall digestive health over time.
Foods to Avoid for GERD: A Malaysia-Focused Guide
Many online guides overlook local diets, but in Malaysia, certain traditional foods can trigger acid reflux. Being mindful of these can help manage your GERD effectively.

Common Trigger Foods
These locally popular items are often high in fat, spice, or acidity, which can worsen reflux:
- Sambal, curry, tom yam: Spicy and acidic, these can irritate the esophagus.
- Nasi lemak: High-fat coconut milk and fried accompaniments may trigger symptoms.
- Fried kuey teow & roti canai: Fried, oily foods increase reflux risk.
- Teh tarik & kopi: Caffeine plus dairy can relax the lower esophageal sphincter.
- Carbonated drinks: Fizzy drinks increase stomach pressure and reflux.
- Chocolate & mint: Can relax the LES and promote acid backflow.
- Citrus fruits: Oranges, lemons, and other acidic fruits may worsen heartburn.
- Onions & garlic: Can trigger symptoms in some individuals, especially when raw.
Modern Malaysian lifestyles, including late-night meals, high-fat or spicy foods, caffeine, alcohol, and stress, can all contribute to acid reflux.
Popular habits like enjoying spicy sambal, fried dishes, kopi, teh tarik, or heading out for supper at mamak stalls—especially late at night—can increase the risk of reflux if done frequently or in large portions.
Being mindful of these common practices can help reduce discomfort and protect digestive health.
Early recognition and management are key to preventing progression to chronic GERD and long-term complications.
Foods That May Help Soothe Reflux
Including these foods in your diet may help calm your digestive system and reduce GERD symptoms:
- Oatmeal: High in fiber and gentle on the stomach.
- Bananas & melon: Naturally low-acid fruits that can help coat the esophagus.
- Ginger: Anti-inflammatory properties help soothe irritation.
- Brown rice & leafy greens: Mild, high-fiber options that support digestion.
- Lean proteins: Chicken, fish, and tofu are easier on the stomach.
- Yoghurt: Can be soothing for some, but monitor tolerance as dairy affects individuals differently.
Tip: Try keeping a food diary to help identify your personal triggers and tailor a digestive-friendly diet that minimises reflux while still enjoying Malaysian flavors!
Treatment Options: How to Manage Acid Reflux & GERD Long-Term
Managing acid reflux and GERD effectively often requires a combination of lifestyle changes, medications, and, in some cases, advanced medical procedures. Understanding each option can help you make informed decisions for long-term relief.
1. Lifestyle Treatments
Lifestyle modifications are often the first line of defense and can significantly reduce symptoms:
- Dietary adjustments: Avoid trigger foods such as spicy, fatty, or acidic dishes, and limit caffeine, chocolate, alcohol, and carbonated drinks. Include reflux-friendly foods like oatmeal, bananas, ginger, and lean proteins.
- Meal habits: Eat smaller, more frequent meals and avoid lying down within 2–3 hours after eating.
- Weight management: Maintaining a healthy weight can reduce abdominal pressure and minimise reflux.
- Sleep adjustments: Elevate the head of the bed and sleep on the left side to prevent nighttime symptoms.
- Stress management: Practices like meditation, yoga, or regular exercise can help lower stress-related digestive flare-ups.
- Avoid tight clothing: Loose clothing around the abdomen can reduce pressure on the stomach.
2. Medications (Under Doctor Supervision)
When lifestyle changes are not enough, medications may be prescribed to manage acid production and protect the esophagus:
- Antacids: Provide quick, short-term relief by neutralising stomach acid.
- H2 blockers: Reduce acid production for longer periods than antacids.
- Proton pump inhibitors (PPIs): Stronger acid-suppressing medications that can promote healing of the esophagus in severe cases.
- Prokinetics: Help strengthen the lower esophageal sphincter and improve stomach emptying.
⚠️ Important: Always use these medications under medical supervision. Overuse can mask symptoms or cause side effects, and long-term treatment should be guided by a doctor.
3. When Surgery or Advanced Treatment Is Needed
For individuals with severe or persistent GERD who do not respond to lifestyle changes or medications, surgical or advanced procedures may be considered:
- Fundoplication: A procedure that strengthens the lower esophageal sphincter to prevent acid reflux.
- Robotic-assisted GERD surgery: Minimally invasive, precise surgery with faster recovery times and long-term symptom relief.
- Endoscopic treatments: Newer, less invasive techniques that help tighten the esophagus or reduce reflux without major surgery.
Choose Island Hospital for GERD Care
At Island Hospital, we offer comprehensive care for patients dealing with acid reflux and GERD, combining expertise, technology, and personalised support:
- Experienced gastroenterologists: Our specialists provide accurate diagnosis and tailored treatment plans.
- Modern diagnostic facilities: Advanced endoscopy and imaging ensure precise assessment of your condition.
- Multidisciplinary medical support: Collaborating across specialties to address all aspects of your digestive health.
- Personalised treatment plans: From lifestyle guidance to medications and advanced procedures, care is tailored to your needs.
Regain comfort and peace of mind—book your GERD consultation today.
FAQ
1. Is GERD dangerous?
Yes. If left untreated, GERD can lead to long-term complications such as esophagitis, ulcers, narrowing of the esophagus, or, in rare cases, an increased risk of esophageal cancer. The good news is that with early diagnosis, lifestyle changes, and appropriate treatment, GERD is highly manageable.
2. Can stress worsen acid reflux?
Yes. Stress doesn’t directly cause GERD, but it can increase stomach acid production, slow digestion, and make the esophagus more sensitive, triggering or worsening symptoms like heartburn and regurgitation.
3. Is GERD lifelong?
Not necessarily. While GERD can be chronic for some, many patients successfully manage or even resolve symptoms through lifestyle modifications, dietary adjustments, and medical treatment. Ongoing care and monitoring can help prevent recurrence.
4. Are PPIs safe long term?
Proton pump inhibitors (PPIs) are highly effective at reducing stomach acid and healing the esophagus when used correctly. However, long-term use should always be monitored by a doctor to avoid potential side effects and ensure continued effectiveness.






