
24 Jan Treatment of an overactive thyroid gland or hyperthyroidism
Treatment of an overactive thyroid gland or hyperthyroidism
By Island Hospital | Jan 24, 2026 12:00:00 PM
Hyperthyroidism, also known as an overactive thyroid, is a common thyroid disorder associated with excess thyroid hormone production.
In 2023, a study found that the prevalence of thyroid disorders in Malaysia is about 3.4%, the second most common endocrine disorder after diabetes.
From recognising the symptoms to exploring treatment options. Whether you’ve just been diagnosed, are supporting a loved one, or simply want to learn more about thyroid health, you’ll find practical, evidence-based information to guide your journey.
Common Symptoms & How It Affects the Body
The thyroid hormone has physiological effects on multiple organ systems. Hyperthyroidism shows through many symptoms involving these organ systems, which can develop slowly or suddenly.
Some people experience mild symptoms, while others face severe effects that substantially affect their daily life.
Typical signs:
- Sensitivity to heat
- Muscle weakness
- Reduced libido
- Heart palpitation
- Shaky hands
- Increased
- Weight loss, but with a small amount (10%) of people experience weight gain
- Hair loss or brittle hair
- Enlarged thyroid gland, called a goitre, or a swollen neck
- Swelling of the eyes
The condition’s effects on mental health are just as important. One may experience:
- Nervousness, anxiety, and irritability
- Trouble sleeping (insomnia)
- Mood swings
- Hyperactivity and restlessness
- Tiredness
Extra thyroid hormones affect your central nervous system, causing these psychological symptoms.
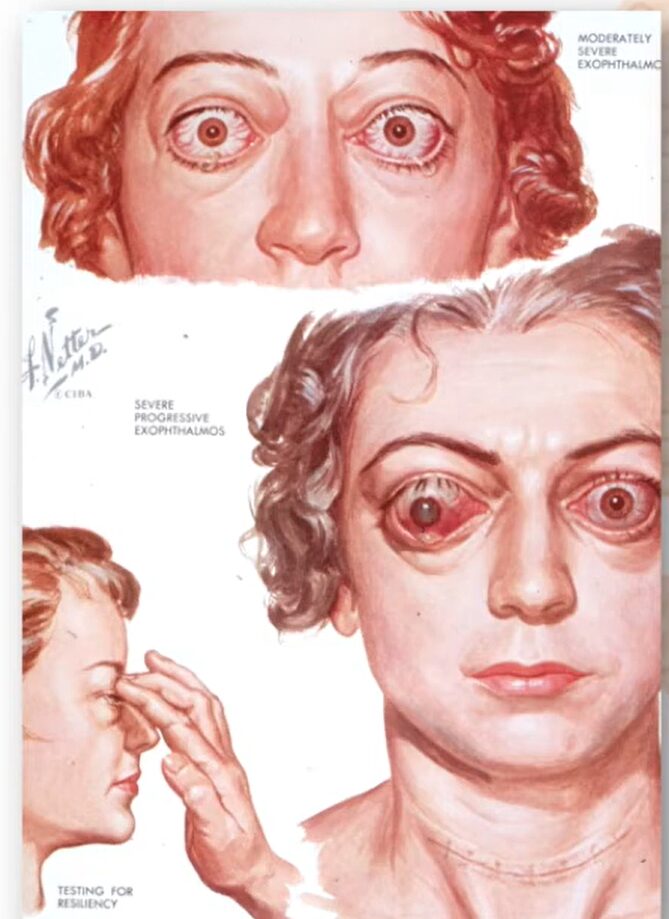
Illustration of thyroid eyes used in the (HOKKIEN) Treating an Overactive Thyroid Gland by Assoc Prof Dato’ Dr Malik Mumtaz video.
People with Graves’ disease (hyperthyroidism’s most common cause) can develop thyroid eye disease, which can range from mild to severe. Symptoms include:
- Bulging eyes (proptosis)
- Red, dry, or irritated eyes
- Light sensitivity
- Eye pain and headaches
- Double vision
- Vision loss in severe cases
Eye symptoms usually affect both eyes, but sometimes show up in just one. These changes might stay even after treating hyperthyroidism because scarring keeps tissues from returning to normal.
Autoimmune disease causes, which include Graves disease, affect women more than men and typically occur in those aged 20-40.
Other causes include:
Toxic adenoma and toxic multinodular goitre are conditions where nodules in the thyroid gland begin producing excessive thyroid hormone autonomously.
Viral thyroiditis, also known as de Quervain’s thyroiditis, occurs when a viral infection causes inflammation of the thyroid gland, leading to temporary thyroid dysfunction.
Exogenous iodine, which refers to iodine consumed from external sources such as supplements or iodine-rich medications, can also disrupt normal thyroid function.
Certain medications like amiodarone, commonly used to treat heart rhythm disorders, are known to affect thyroid hormone production and can lead to either hyperthyroidism or hypothyroidism.
Untreated hyperthyroidism can cause serious problems, including heart issues like atrial fibrillation. In rare cases, poor control of the condition can lead to a thyroid storm, an emergency, life-threatening situation, or thyroid cancer
Early diagnosis and proper management depend on knowing these symptoms. Quick medical help becomes possible when you spot the signs, starting your path to successful treatment.
Medical Treatment Options
Antithyroid medications
Antithyroid medications (ATDs) block your thyroid’s hormone production.
Doctors often prescribe these:
- Methimazole (Tapazole) inhibits the enzyme thyroid peroxidase and is a primary choice for oral therapy. Also used for thyroid strom
- Carbimazole reduces symptoms by reducing the amount of hormones your thyroid produces. Comes in tablet form and improves symptoms in 1 to 3 weeks
- Propylthiouracil (PTU) move into your thyroid gland and stops the absorption of iodine.
The treatment usually runs for 12 to 18 months. Your thyroid hormone levels take several weeks or months to return to normal, and you’ll notice improvements gradually. These drugs control hyperthyroidism effectively while you take them.
ATDs remission rate is approximately 25-50%.
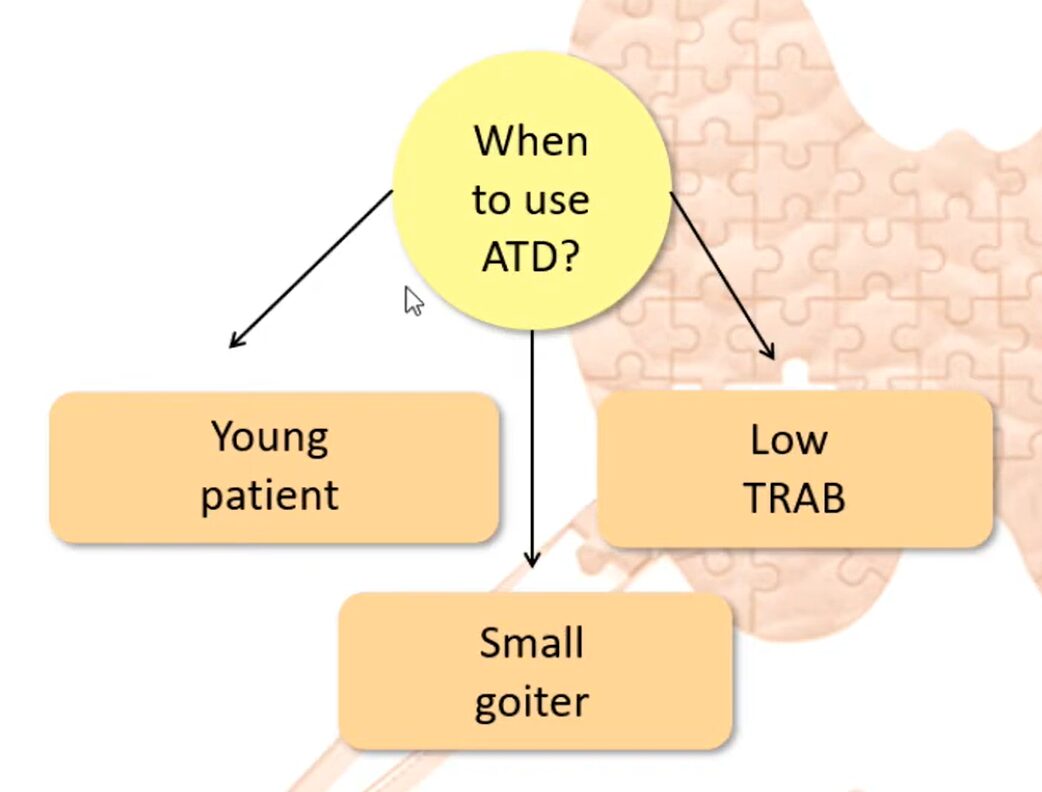
Antithyroid medications or drugs are a good fit for young adults, and patients with negative or low-titre TRAb in remission can discontinue medication depending on their circumstances.
ATDs can also be effective in those who have smaller goitres, avoiding the need for a thyroidectomy (total removal of the thyroid).
Symptom-relief drugs
Beta-blockers such as propranolol, atenolol, and metoprolol quickly ease many hyperthyroidism symptoms but without affecting hormone levels.
These medications help with rapid heartbeat, tremors, anxiety, and heat intolerance. They work by blocking the effects of adrenaline on nerve cells. Patients feel better with beta-blockers while other treatments normalise their thyroid function.
Radioactive Iodine Therapy (RAI)
RAI is a very effective treatment with a higher than 90% success rate, which destroys thyroid follicular cells, ultimately reducing the amount of hormones it can produce.
It is administered as a drink or capsule, containing iodine and a low dose of radiation that is absorbed by your thyroid. The dose Dato’ Dr Malik Mumtaz typically administers is 15mCi.
Dato’ Dr Malik Mumtaz shares: “80% of my patients drink it only once.”

Dato’ Dr Malik Mumtaz showcasing RAI treatment process.
Thyroidectomy
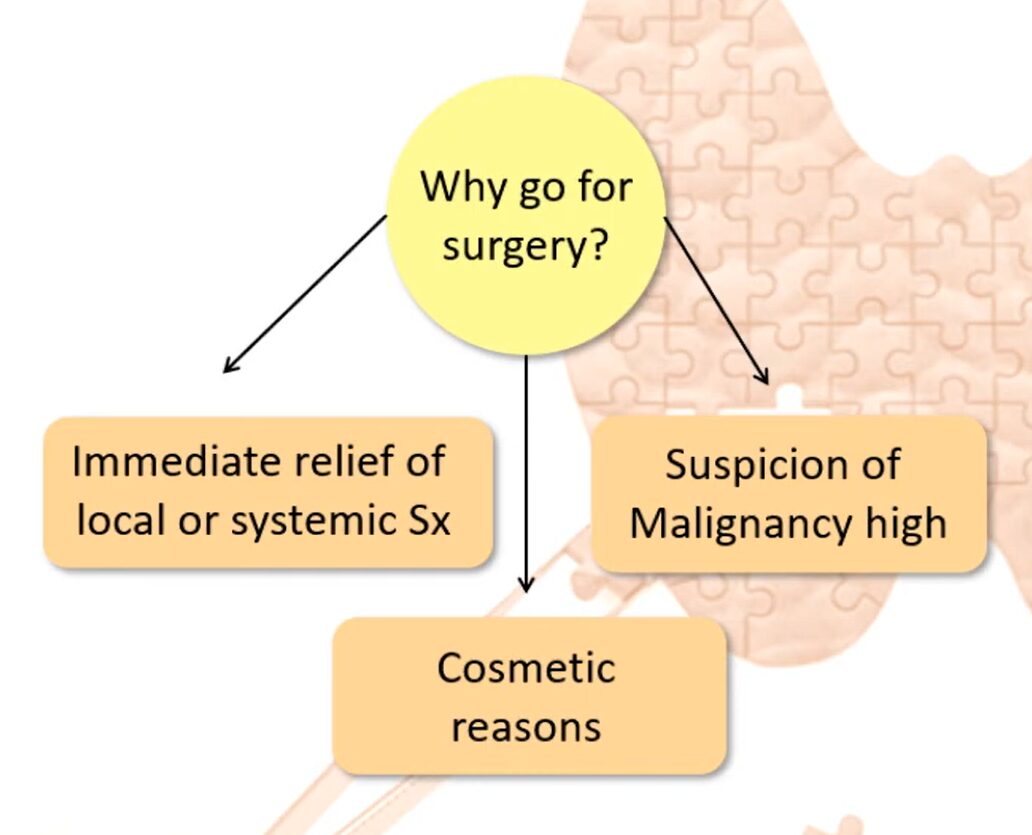
Thyroidectomy is the surgical removal of all or part of the thyroid. It offers quick relief, typically requiring only a day or two in the hospital and has a more than 90% success rate of ridding you of hyperthyroidism.
When there is suspicion of cancer, it is also best to go for surgery. When discussing cosmetics, this refers to patients with enlarged goitres who are affected by their appearance.
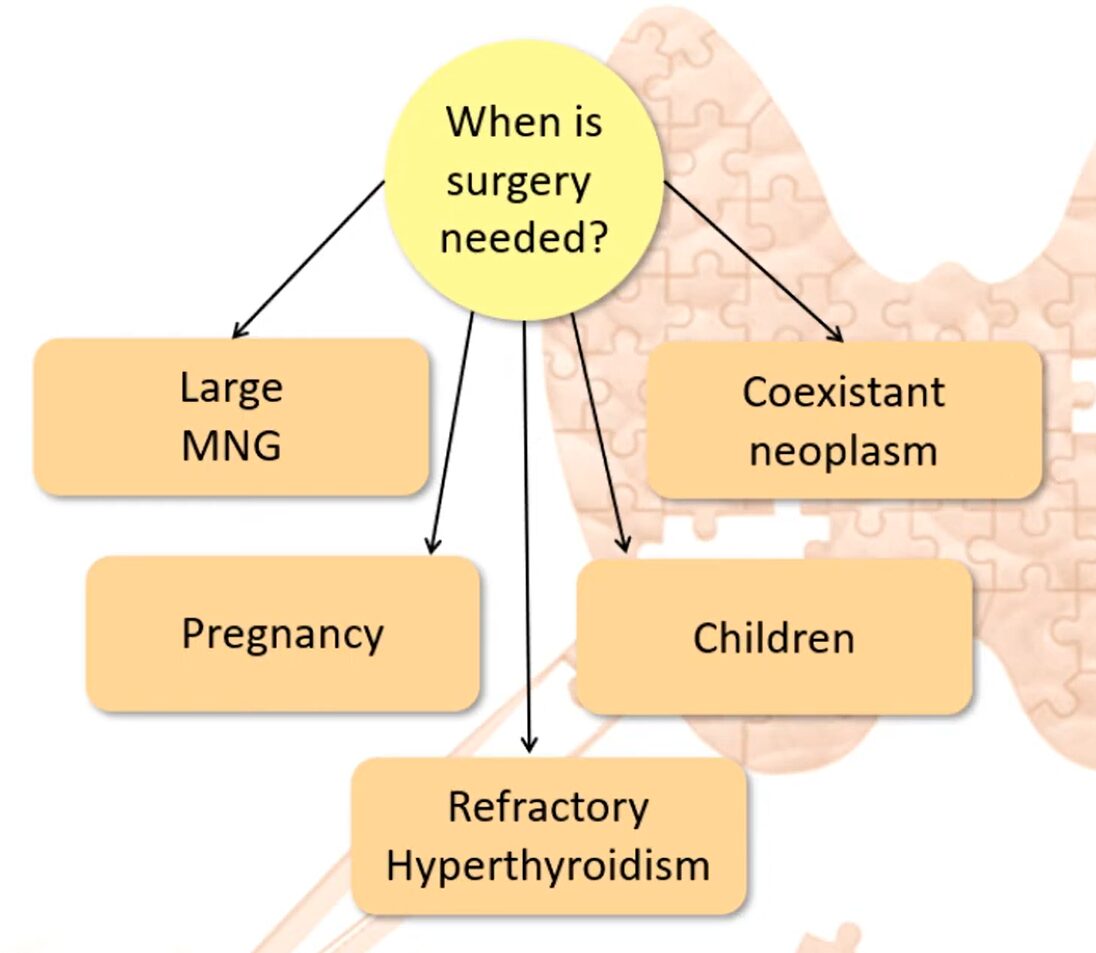
Patients who are a good fit for surgery tend to fall under these categories:
- Large multinodular Goitre (MNG): When goitres extend substernally and compress the trachea or oesophagus, thyroidectomy can relieve obstructive symptoms and improve quality of life.
- Coexistent Neoplasm: Coexistent Neoplasm refers to two tumours found in a patient. With surgery, doctors can accurately diagnose the cancer risk by removing the thyroid and performing a biopsy.
- Pregnancy: Surgery is an option for pregnant women as it improves symptoms quickly and has a great chance of remission, but ATDs are also an option that can be explored.
- Children: Surgery is chosen when definitive therapy is required or the child is too young for radioactive iodine
- Refractory Hyperthyroidism: Surgery is recommended when hyperthyroidism fails to respond to conventional antithyroid medications .This includes relapse of hyperthyroidism after antithyroid drugs or low uptake of radioactive iodine.
Check out the outcome of a thyroidectomy below.
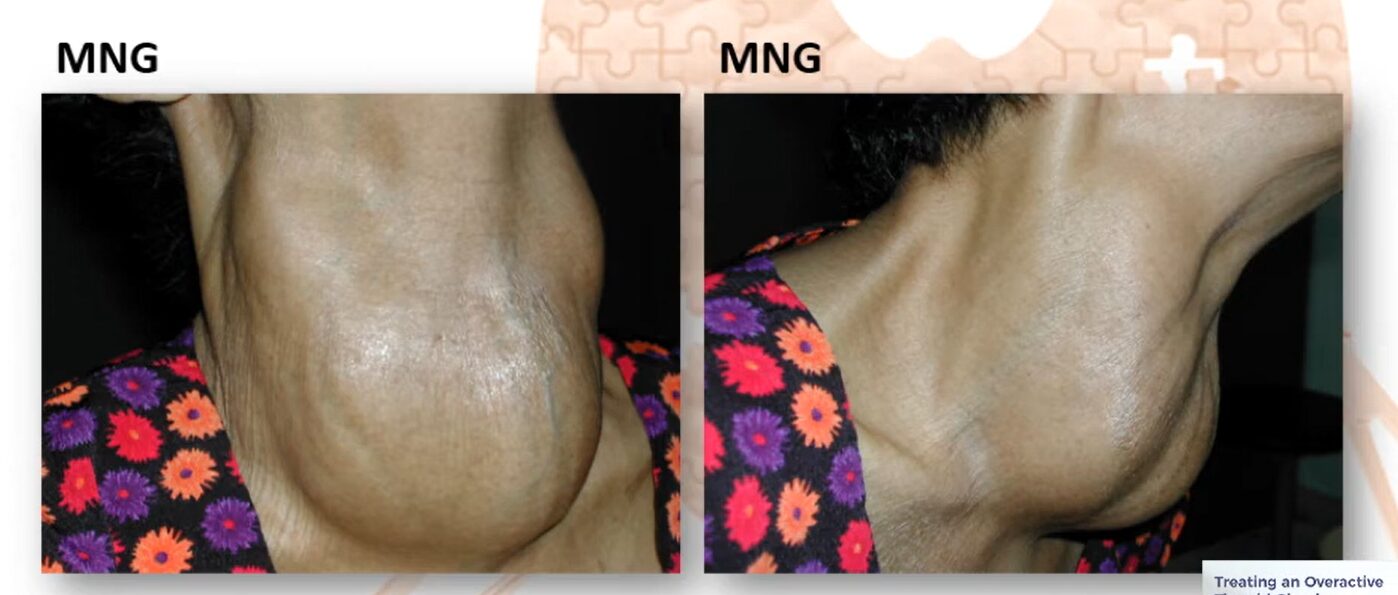
A patient with multinodular Goitre (MNG).

Patient after surgical removal of the thyroid.
Long-Term Management & Monitoring
The goal of hyperthyroidism treatments is to achieve remission, where the thyroid stops producing an excessive amount of hormones. However, each treatment comes with some risk, specific benefits and remission rates mentioned above.
Without your thyroid, you become hypothyroid, which occurs when a person experiences hypothyroidism (when the thyroid gland does not make and release enough hormone).
Those who undergo a thyroidectomy or radioiodine therapy need lifelong treatment with thyroid hormone replacement medication, such as Euthyrox, which supplies the body with healthy amounts of thyroid hormones.
Smoking cessation is also essential when dealing with hyperthyroidism, especially with Graves’ ophthalmopathy.
Monitoring Treatment Of Hyperthyroidism
After Radioactive Iodine Treatment (RAI)
Once your thyroid hormone levels return to normal, you’ll need yearly thyroid function tests for the rest of your life, or more frequently if you develop symptoms of an underactive or overactive thyroid. It’s important to note that TSH levels (a key thyroid marker) can remain artificially low for a month or more even after your hyperthyroidism is resolved, so your doctor will interpret these results carefully alongside your free T4 and free T3 levels to get the complete picture.
Patients Treated with Antithyroid Drugs (ATDs)
Once your thyroid hormone levels stabilise on the lowest effective dose of medication, you’ll need check-ups and blood tests every 2–3 months. If you’ve been on methimazole (MMI) for an extended period (more than 18 months), your doctor may reduce the frequency of monitoring to every 6 months, provided your condition remains stable.
Want to hear about Treating an Overactive Thyroid Gland in Indonesian? Mengobati Kelenjar Tiroid yang over aktif atau hipertiroid by Assoc Prof Dato’ Dr Malik Mumtaz
Risks and Trade-Offs: Medication, RAI and Surgery
Side effects of ATD
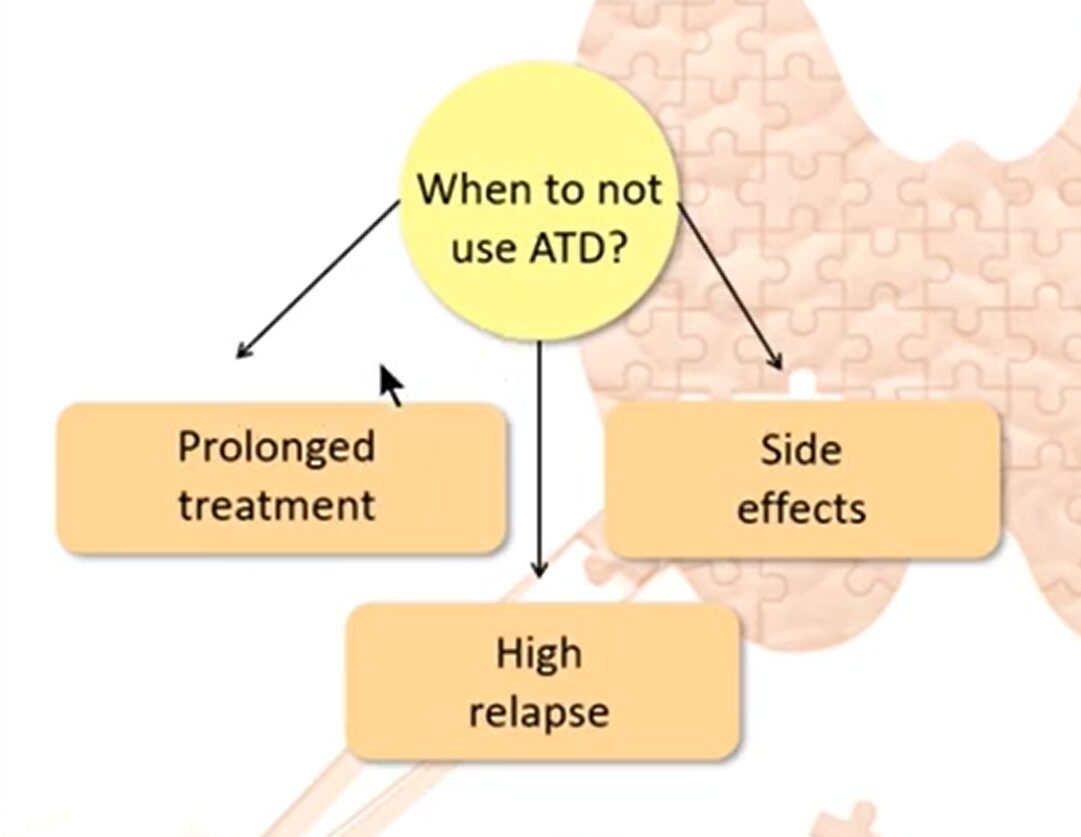
The side effects of ATDs are:
Allergies: For some, medication may result in a rash but it may resolve with a lower dose. In some cases there is also a 10% chance of cross-reactivity by CMZ and PTU when using
Agranulocytosis (low levels of granulocytes (a type of white blood cell): This happens rarely, less than 3 in 10,000 cases. It feels like a severe sore throat or fever and doctors will diagnose it by testing your white blood count.
The Malaysian Endocrine And Metabolic Society (MEMS) also suggests that “liver function and hepatocellular integrity should be assessed in patients taking MMI or PTU who experience pruritic rash, jaundice, light-coloured stool or dark urine, joint pain, abdominal pain or bloating, anorexia, nausea, or fatigue.”
Considerations with RAI
RAI is typically not suitable for
- Pregnant/breastfeeding women
- Planning for a pregnancy in the next 6 months
- Children below 5 years old
- Those with severe thyrotoxicosis, the risk of thyroid storm
- Severe thyroid eye disease
- Very large thyroid gland, in this case, it would be more effective to opt for surgery
While rare, there is also a possibility of triggering radiation alarms in security scanners or at airport checkpoints. Do not fret. Medical documents and a clear description of the situation regarding your treatment to the officers should suffice.
Surgery Consideration and Risks
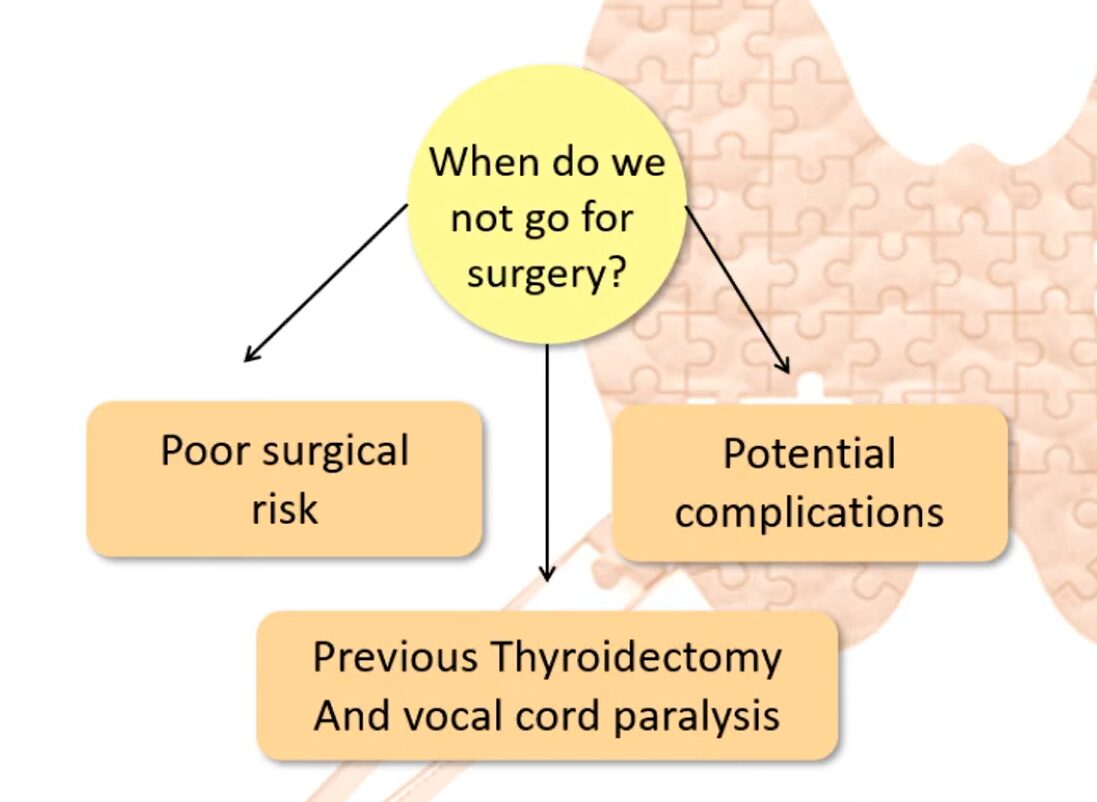
Your doctor also considers certain factors before recommending surgery, as it is not a good fit for elderly who are poor surgical risk or individuals with existing conditions that can be potential complications.
Patients with a previous thyroidectomy and vocal cord paralysis are also not a fit for surgery.
While complications from thyroidectomy are uncommon, potential risks include:
- Severe haemorrhage that may obstruct the airway and impair breathing
- Nerve damage resulting in vocal cord paralysis and voice hoarseness
- Injury to the parathyroid glands, causing hypoparathyroidism and reduced blood calcium levels
These complications are more likely in patients with invasive tumours, cancer spread to neck lymph nodes, or those undergoing repeat thyroid surgery.
When to See a Doctor and What to Ask
If you observe any of the symptoms above, reach out to your local healthcare provider.
Your doctor will run a thyroid function test (blood test) to measure your thyroid-stimulating hormone (TSH), triiodothyronine (T3), and thyroxine (T4) hormone levels. A combination of low TSH with high T3/T4 points to hyperthyroidism. Your physician might need antibody tests to determine why it happens, such as in Graves’ disease.
You’ll need to see an endocrinologist if thyroiditis isn’t likely or has been ruled out. Pregnant women need immediate specialist care because untreated hyperthyroidism can affect both mother and baby.
Here are some questions to ask your doctor:
| What treatment options do I have, and which is best for my situation? | |
| How will I know if my treatment is working? | |
| What side effects should I watch for? |
|
| How often will I need follow-up testing? | |
| Will my hyperthyroidism treatment affect my other health conditions? |
Doctors will consider age, aetiology, severity of the case, their experience and your preference to develop a treatment plan for you.
Want to see this article presented in Hokkien?
A Trusted Team of Thyroid Specialists
Island Hospital‘s Endocrinology Department offers complete thyroid care from specialists who excel at managing hyperthyroidism. Our team have been praised for their ability to comfort and provide hope to patients during treatment.
If you are looking to visit Island Hospital’s Endocrinology Department, book an appointment here.
FAQ
1. What should I avoid while receiving treatment for a thyroid condition?
Strenuous exercise in patients with uncontrolled hyperthyroidism or hypothyroidism is not advisable since these conditions affect the person’s metabolism and heart rate.
Following thyroid surgery, strenuous activity and heavy lifting should be avoided for at least two weeks, and patients should avoid over-extending the neck backwards for 2 weeks after surgery or until the doctor advises otherwise.
After radioactive iodine treatment, you must isolate or stay a distance away from pregnant women and children, as there’s a risk of radiation exposure to people around you.
The time span of isolation depends on the dose administered.
2. When should I start checking my thyroid function, and how often should screening be done?
For individuals 40 and older, you should participate in regular screening together with your annual health checkups, especially for women. More frequent screening is appropriate in people with risk factors such as family history of thyroid problems, and women with infertility, recurrent miscarriage, or undergoing fertility treatment.
3. How to treat hyperthyroidism in pregnancy?
The prevalence of hyperthyroidism in pregnancy ranges from 0.1% to 0.4%, with Graves’ disease accounting for 85% of these cases.
For pregnant women, medication therapy is typically the sole option. Because radioiodine treatment kills the embryonic thyroid gland and causes permanent hypothyroidism in the newborn, it is not recommended during pregnancy.
Subtotal thyroidectomy is a treatment option in situations where the woman has not been able to follow antithyroid medication therapy, where consistently high doses of antithyroid medications are required to control the hyperthyroidism, or when serious adverse reactions to antithyroid medication therapy are observed.
The common antithyroid drugs used in pregnancy are the thionamides, propylthiouracil (PTU), methimazole and carbimazole.
4. Can I shower or get the wounds wet after the procedure?
Most patients can shower within 24–48 hours, but soaking the wounds in a bath or swimming should be avoided until healing is complete. Always follow your surgeon’s specific instructions to reduce the risk of infection.
5. How and when should I take hypothyroid medication (Levothyroxine)?
Hypothyroidism is something that happens after RAI or surgical removal of your thyroid. You’ll then need to consume medication to ensure your body maintains stable hormone levels. Follow these rules for best results:
- Timing: Take your tablet on an empty stomach. The best times are either one hour before breakfast or at bedtime (at least three hours after your last meal).
- Watch what you drink: Avoid taking your pill with coffee (especially espresso) or grapefruit juice, as these can block absorption. Use plain water instead.
Note: Even if your symptoms (like dry skin or feeling cold) start to improve, do not change your dose without a blood test. These tests are necessary because symptoms alone are not always a reliable way to tell if your dose is correct.






