17 Oct Top 10 Signs of Diabetes You Can See: Doctor Explains
Top 10 Signs of Diabetes You Can See: Doctor Explains
By Island Hospital | October 17, 2025 10:34:09 AM
Diabetes is like a silent epidemic, often creeping up on individuals unnoticed until it has already caused significant damage. Although many individuals are familiar with the more obvious symptoms, like excessive thirst or frequent urination, sometimes the overlooked signs at bay may also serve as critical early warnings.
This disease’s staggering prevalence, especially Type 2 diabetes, which accounts for over 95% of all cases according to the World Health Organisation, affects an estimated 422 million adults worldwide, with numbers only continuing to rise.
This article will cover ten subtle warning signs of diabetes, explaining the medical reasoning behind each one and offering practical advice on what to do. With these often-missed signals, our goal is to help you understand your body better and take the proactive steps you need towards your health.
Top 10 Visible Signs of Diabetes (Doctor Explains)
Diabetes is a condition where the body either doesn’t produce enough insulin or can’t effectively use the insulin it produces.
Think of your body as a bustling city, and your cells are its houses. The food you eat is like a giant truck delivering energy (sugar) to these houses.
Insulin is the special key that unlocks the doors to these houses, allowing the sugar to get in and be used for power. In an individual with diabetes, something goes wrong with this key which results in two main problems:
- Type 1 Diabetes
- Type 2 Diabetes
When sugar piles up in your bloodstream, it’s like a traffic jam. It can’t get to the houses that need it, so they become low on energy. At the same time, all that extra sugar in the blood can start to damage the roads, bridges, and other parts of the city (your organs, blood vessels, and nerves), leading to health problems down the road.
Here is a more detailed look at 10 common and visible signs of diabetes:
1. Frequent Urination (Polyuria)
- What it is: The need to urinate more often than usual, often in large amounts,
including waking up multiple times during the night to go to the bathroom.
- What you see/feel: You feel an intense need to urinate, and the volume of urine passed is often significant.
- Why it happens: When blood sugar levels are high, the kidneys work overtime to filter out the excess glucose. To do this, they draw more water from the body, leading to an increase in urine production. This is the body’s natural attempt to flush out the surplus sugar.
- Doctor’s insight: This is one of the classic early signs of diabetes. It’s the body’s way of trying to correct high blood sugar. If you notice a sudden and persistent increase in how often you urinate, especially at night, it’s a strong indicator that your blood sugar levels are elevated and you should get tested.
2. Acanthosis Nigricans
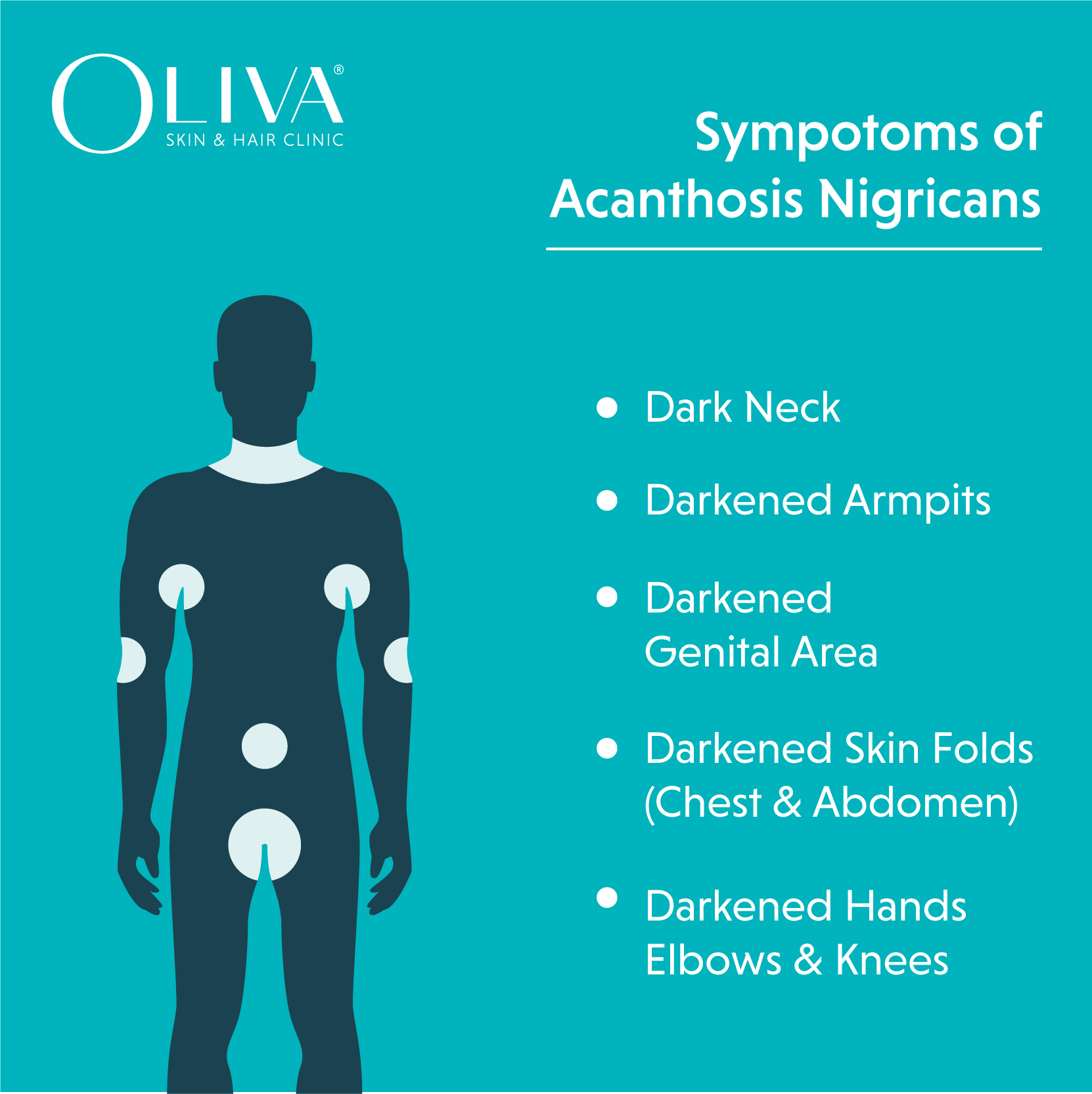
- What it is: A skin condition characterised by dark, velvety patches of skin, typically found in body folds and creases.
- What you see/feel: Patches of thickened, dark skin on the back of your neck, armpits, groin, elbows, or knuckles. The skin may feel soft and velvety to the touch.
- Why it happens: High levels of insulin in the blood, which is common in people with insulin resistance or Type 2 diabetes, can cause skin cells to reproduce more quickly than normal. This excess growth leads to the dark, thick patches.
- Doctor’s insight: This is a key visual marker of insulin resistance and often appears before a formal diagnosis of Type 2 diabetes. It’s a clear signal that the body is not using insulin effectively and is a good reason to get your blood sugar checked.
3. Skin Tags (Acrochordons)
- What it is: Small, soft, flesh-colored or brownish growths that hang off the skin.
- What you see/feel: Tiny, harmless bits of skin that often appear on the neck, armpits, or eyelids. They are typically painless unless they are irritated by clothing or jewelry.
- Why it happens: While the exact connection isn’t fully understood, skin tags are strongly linked to high insulin levels and insulin resistance. They are also common in people who are overweight, which is a major risk factor for Type 2 diabetes.
- Doctor’s insight: The presence of multiple skin tags can be a subtle but important clue. While they are not a definitive sign of diabetes on their own, a high number of them, especially in someone with other risk factors, should prompt a conversation with a doctor about getting screened for diabetes.
4. Infections
- What it is: A higher-than-normal frequency of infections, particularly yeast infections, urinary tract infections (UTIs), and fungal infections.
- What you see/feel: Repeated yeast infections (thrush), UTIs, or slow-healing skin infections. The infections can be more severe and harder to treat than usual.
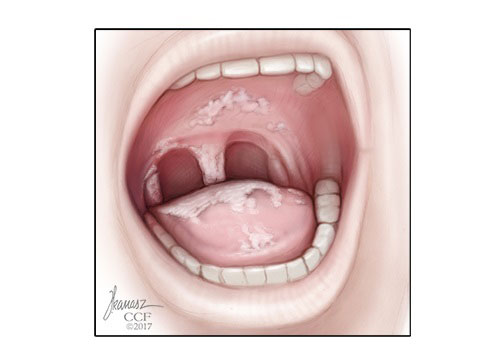
- Why it happens: High blood sugar creates a favorable environment for bacteria and fungi to thrive. Additionally, uncontrolled blood sugar can weaken your immune system, making it more difficult for your body to fight off infections.
- Doctor’s insight: Recurrent infections, especially in people who don’t have a history of them, can be a major red flag for undiagnosed diabetes. It shows that your body’s defense mechanisms are compromised.
5. Diabetic Stiff Hand Syndrome (Positive Prayer Sign)
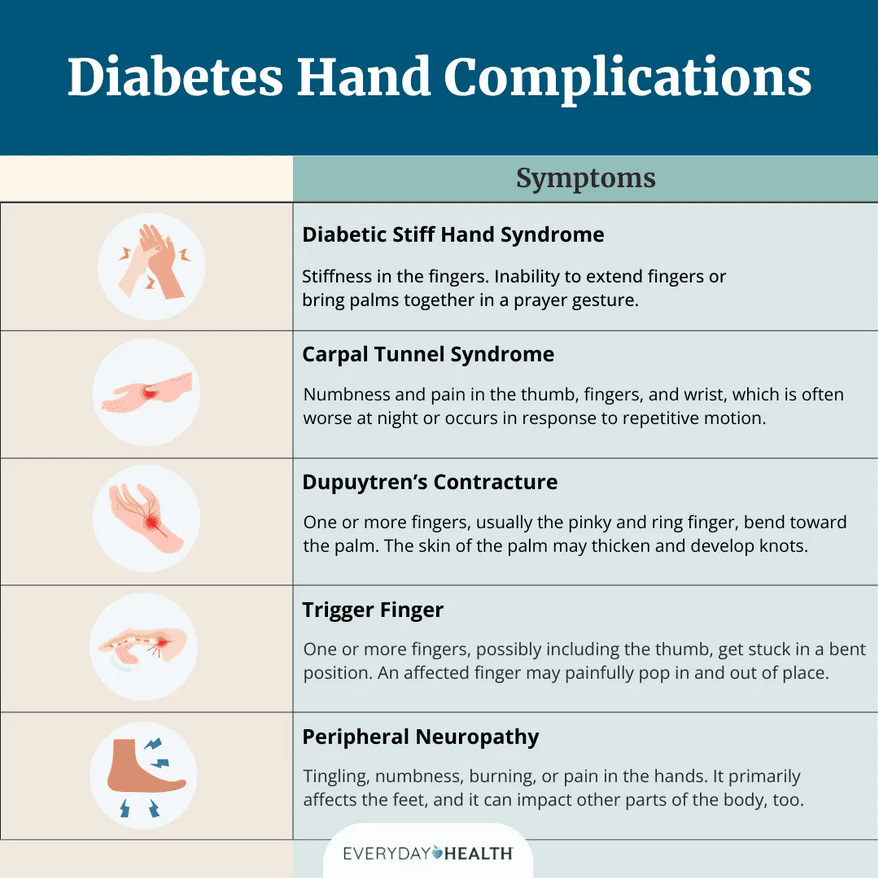
- What it is: A condition that causes the skin on the hands to become thick and waxy, and the joints in the fingers to stiffen.
- What you see/feel: Your fingers feel stiff, and it becomes difficult to fully straighten or flatten your hands. A common test is the “prayer sign,” where you try to press your palms together. If your hands cannot meet completely, leaving a gap, it is a “positive prayer sign.”
- Why it happens: Long-term high blood sugar can cause a process called “glycation,” where sugar molecules attach to proteins in the body, including collagen. This makes the collagen in your skin and tendons less flexible, leading to stiffness.
- Doctor’s insight: This is a complication of long-standing diabetes. It’s a sign of the long-term damage that high blood sugar can cause to connective tissues and is often found in individuals who have had diabetes for a while.
6. Trigger Finger & Frozen Shoulder
- What it is: Trigger finger is a condition where a finger gets “stuck” in a bent position. Frozen shoulder (adhesive capsulitis) is the progressive stiffening and pain of the shoulder joint.
- What you see/feel: For trigger finger, a finger may catch, lock, or pop when you try to straighten it. For frozen shoulders, you experience a gradual loss of motion in your shoulder, making it difficult to lift your arm or perform everyday tasks.
- Why it happens: Similar to diabetic stiff hand syndrome, high blood sugar can affect the connective tissues in the hands and shoulders, causing inflammation, thickening, and scarring of the tendons and joint capsule.
- Doctor’s insight: These musculoskeletal issues are more common and can be more severe in people with diabetes. They often signal that the body’s connective tissues have been affected by high blood sugar over a period of time.
7. Neuropathy
- What it is: Nerve damage caused by high blood sugar. It most commonly affects the nerves in the legs and feet (peripheral neuropathy) but can also affect other parts of the body.
- What you see/feel: A wide range of sensations, including tingling, numbness, a pins-and-needles feeling, sharp pains, or a burning sensation. You may also experience muscle weakness or a loss of feeling in your feet, which makes you more prone to injury.
- Why it happens: High blood sugar levels can damage the small blood vessels that supply nerves with oxygen and nutrients. Without proper nourishment, the nerves begin to malfunction.
- Doctor’s insight: This is a serious complication that can be very painful and lead to other problems, especially foot complications. The loss of sensation can prevent a person from noticing a cut or sore, which can then become infected and lead to a more severe issue.
8. Charcot Foot
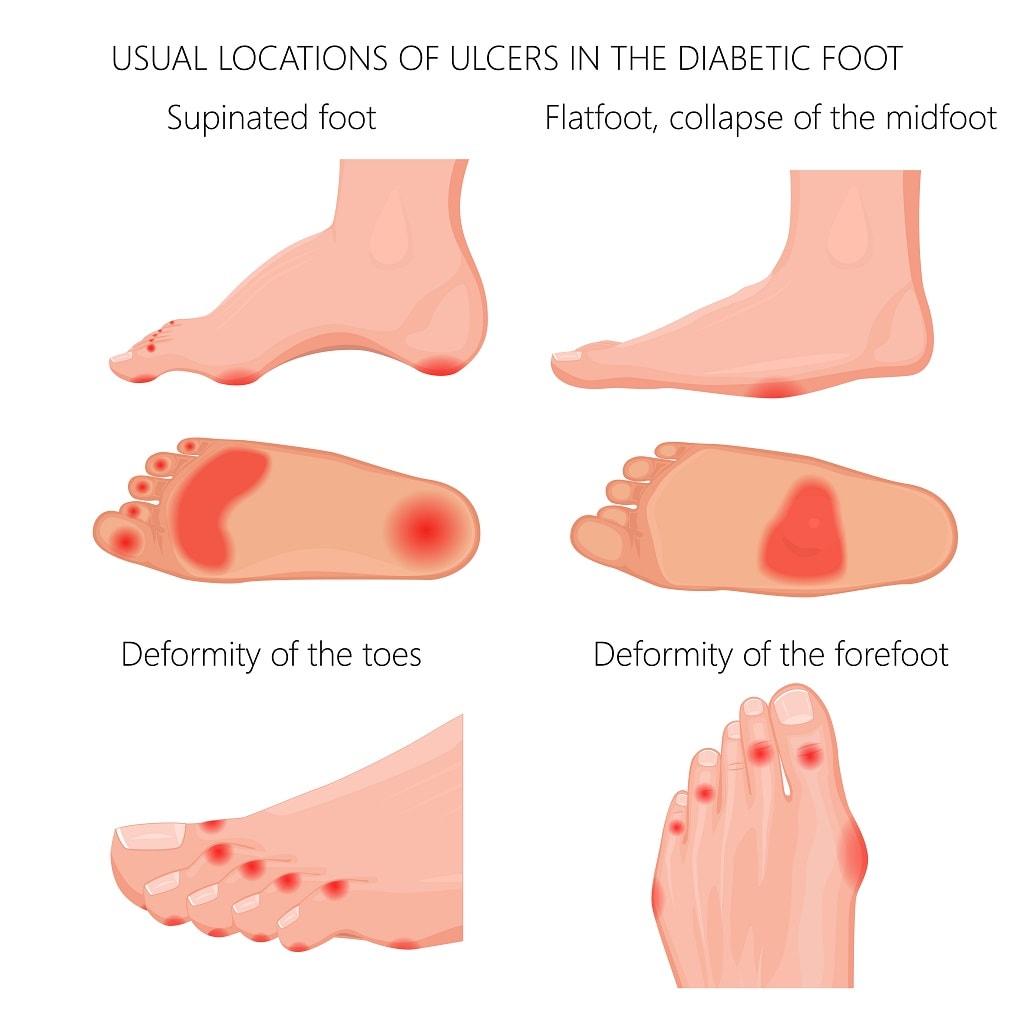
- What it is: A rare but severe complication of diabetic neuropathy where the bones in the foot weaken and fracture, leading to the collapse of the foot’s arch.
- What you see/feel: The foot may be swollen, red, and feel warm to the touch. As the condition progresses, the arch of the foot collapses, leading to a “rocker-bottom” shape. Due to the nerve damage, the person may not feel any pain, which can delay diagnosis.
- Why it happens: It’s a combination of nerve damage (neuropathy) and blood flow changes. The neuropathy prevents the person from feeling a minor injury or stress on the foot. The repeated stress on the weakened bones leads to fractures and joint dislocation, causing the foot to deform.
- Doctor’s insight: This is a medical emergency. If you have diabetes and notice a sudden change in the shape or temperature of your foot, especially with swelling, seek medical attention immediately. Early intervention is crucial to prevent severe deformity and potential amputation.
9. Diabetic Foot Infection
- What it is: An infection of the foot, often starting from a minor cut, blister, or callus that goes unnoticed due to nerve damage.
- What you see/feel: The wound may be red, swollen, and have pus or other drainage. There may be a foul odor. Because of neuropathy, the person may not feel pain, which can cause the infection to become serious before it’s noticed.
- Why it happens: The combination of nerve damage (loss of protective sensation), poor blood circulation, and a weakened immune system creates a perfect storm for a small wound to become a severe infection.
- Doctor’s insight: Foot infections are a leading cause of hospitalisation and amputation for people with diabetes. Regular foot checks are non-negotiable for anyone with diabetes. Look for any cuts, blisters, or red spots, and seek immediate care for any signs of infection.
10. Gastroparesis
- What it is: A form of neuropathy that affects the nerves of the stomach, causing the stomach muscles to slow down or stop working. This means food stays in the stomach for too long.
- What you see/feel: Nausea, vomiting, feeling full after only a few bites, a feeling of bloating, and a loss of appetite.
- Why it happens: High blood sugar over time can damage the vagus nerve, which controls the muscles of the stomach and small intestine. This damage disrupts the normal process of digestion.
- Doctor’s insight: Gastroparesis can make it very difficult to manage blood sugar, as the delayed emptying of the stomach makes it unpredictable when and how much sugar will be absorbed into the bloodstream. It’s a more advanced complication and highlights the importance of keeping blood sugar well-controlled.
Noticing some of the common signs of diabetes? Don’t panic. Take the first step by understanding the symptoms and what you can do next in this article: What You Need To Know About Diabetes.
How Do Doctors Diagnose Diabetes?
If you notice any of the signs above, it is important to consult a doctor. During your visit, they will likely use one or more of the following diagnostic tests:
1. Hemoglobin A1c (HbA1c) Test
The hemoglobin A1c (HbA1c) test is a standard diagnostic tool used to check for diabetes. This test measures the amount of glucose attached to your red blood cells.
Since red blood cells live for about 2-3 months, the HbA1c test provides a clear picture of your average blood sugar levels over that period. It is considered the most effective diagnostic test as it does not require fasting and is not affected by short-term changes in diet or stress.
2. Random Blood Glucose Test
This test measures your blood sugar at a single point in time, regardless of when you last ate. While it can provide a quick snapshot, a single high reading does not always confirm a diagnosis of diabetes and must be followed up with further testing.
HbA1c vs. Random Blood Glucose: Which Test Is More Accurate?
| Criteria | Hemoglobin A1c (HbA1c) Test | Random Blood Glucose Test |
|---|---|---|
| Measures | Average blood sugar over the past 2-3 months | Blood sugar at a specific moment |
| Accuracy | Provides a long-term, more stable picture of blood sugar control | Provides a snapshot; levels can fluctuate based on food and stress |
| Why It's Better | Does not require fasting, less prone to daily fluctuations, and is a more reliable indicator of long-term health risk. | Quick and easy, but requires follow-up for a definitive diagnosis. |
Who Should Get Tested?
Based on the guidelines from the Ministry of Health (MOH) and the Malaysian Diabetes Association (Diabetes Malaysia), here is a breakdown of who should be tested for diabetes.
1. Anyone with Symptoms
Regardless of age or other risk factors, you should get tested if you experience any of the classic symptoms of high blood sugar. These include:
- Frequent urination
- Unexplained thirst
- Fatigue or feeling tired all the time
- Unexplained weight loss
- Blurred vision
- Slow-healing sores or wounds
- Recurrent infections (e.g., skin infections, yeast infections)
Children and teens should also be tested if they are overweight or have obesity and have at least two of the other risk factors listed above.
The best course of action is to have an open conversation with your doctor about your risk factors. They can determine if you need to be tested and what type of test is most appropriate for you.
2. Adults with Risk Factors
Screening is recommended for all adults who are at a higher risk of developing diabetes. The Malaysian Clinical Practice Guidelines (CPG) highlight the following risk factors:
- Age: Screening is generally recommended for all adults aged 30 years and above. This is a key difference from the ADA’s recommendation of age 35, reflecting the higher prevalence of diabetes in younger adults in Malaysia.
- Overweight or Obesity: This is a major risk factor, especially if your Body Mass Index (BMI) is ≥23kg/m2 for Asians.
- Central Obesity (Increased Waist Circumference): A waist circumference of ≥90cm for men and ≥80cm for women is a significant indicator of risk.
- Family History: Having a first-degree relative with diabetes (e.g., a parent, sibling) increases your risk.
- Sedentary Lifestyle: Not engaging in regular physical activity.
- Hypertension (High Blood Pressure): Being diagnosed with hypertension or being on medication for it.
- High Cholesterol: Having low HDL-cholesterol and/or high triglyceride levels.
- History of Gestational Diabetes: Women who had diabetes during pregnancy are at a high risk of developing Type 2 diabetes later in life.
- History of Polycystic Ovarian Syndrome (PCOS): This condition is strongly linked to insulin resistance.
- Previous Test Results: A previous diagnosis of pre-diabetes (Impaired Fasting Glucose or Impaired Glucose Tolerance) is a strong signal for regular monitoring.
Being diabetic doesn’t mean that you can’t enjoy the flavours of food like you used to. Let’s get your FAQs answered in this article on: Diet for Diabetes Patients: 10 Frequently Asked Questions.
How to Prevent Diabetes: Expert Tips
Preventing diabetes is all about making smart, long-term lifestyle changes. Here are some expert tips to help you take control of your health.
1. Healthy Diet Principles
A balanced diet is a powerful tool in preventing diabetes. Focus on a diet that is high in fibre, low in processed foods and refined sugar, and rich in complex carbohydrates.
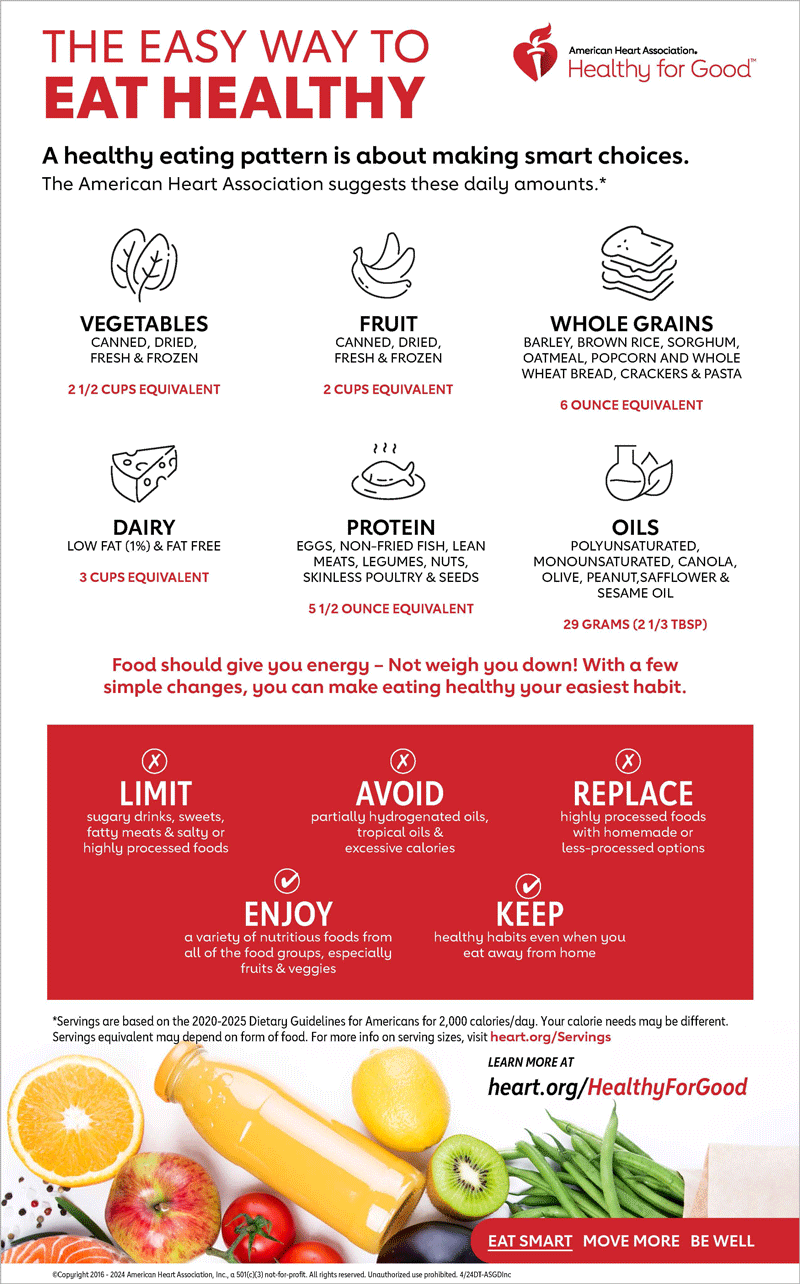
- High-fibre foods: Include plenty of green leafy vegetables like spinach and kale, as well as nuts, seeds, and beans.
- Complex carbs: Choose whole grains like brown rice, oats, and whole wheat bread over white rice and refined bread.
- Low sugar & processed foods: Avoid sugary drinks, processed snacks, and fast food. Focus on lean proteins and healthy fats like those found in fish, avocados, and olive oil. For more tips on a balanced diet, read our articles on Diet for Diabetes Patients and the Malaysian Healthy Plate
2. Best Exercises to Lower Diabetes Risk
Regular physical activity helps your body use insulin more effectively. Aim for at least 150 minutes of moderate-intensity exercise per week.
- Cardio: Activities like brisk walking, jogging, cycling, and swimming.
- Strength training: Incorporate exercises like lifting weights, using resistance bands, or doing bodyweight exercises (e.g., squats, push-ups) at least two times a week.
3. Extra Lifestyle Tips for Long-Term Health
- Maintain a healthy weight: Losing even a small amount of weight can significantly reduce your risk.
- Quit smoking: Smoking can increase insulin resistance.
Get Checked as the First Step!
The insidious nature of Type 2 diabetes lies in its slow, gradual onset. Many people live with the condition for years without realising it, a period when uncontrolled high blood sugar can quietly damage vital organs, including the heart, kidneys, eyes, and nerves.
The first step towards a healthier life starts from noticing the symptoms or having risk factors, to scheduling a simple consultation and blood test to provide clarity and peace of mind.
Island Hospital’s Endocrinology and Diabetes Care Centre is here to support you with expert advice and comprehensive care. Our specialists can help you with screening, diagnosis, and a personalised treatment plan.
FAQs
How do I know for sure if I have diabetes?
The only definitive way to know is through a professional diagnosis by a doctor, which involves a specific blood test. These tests, such as a fasting blood glucose test, an HbA1c test, or an oral glucose tolerance test, measure your blood sugar levels and provide an accurate diagnosis. If you’ve noticed any of the common symptoms (like frequent urination, thirst, or fatigue) or if you have risk factors such as a family history of diabetes, being overweight, or being over the age of 30, it is highly recommended that you consult a doctor for screening.
Can I use a home test to check if I have diabetes?
A home blood glucose meter is an excellent tool for people with a diagnosed condition to monitor their blood sugar daily, but it is not sufficient for a diagnosis. A single reading from a home meter only provides a snapshot of your blood sugar at that moment. For a definitive diagnosis of diabetes or pre-diabetes, you must have a lab blood test (like an HbA1c test) performed at a clinic or hospital.
Is pre-diabetes a reversible condition?
Yes, absolutely. Pre-diabetes is a warning sign, and it can be a reversible condition. It is a critical window of opportunity to prevent the progression to Type 2 diabetes. By making significant lifestyle changes—such as adopting a healthier diet, increasing physical activity, and losing weight—you can often bring your blood sugar levels back to a normal range and avoid a diabetes diagnosis.
What are the blood sugar levels for pre-diabetes?
The pre-diabetes range is defined by specific blood test results, which indicate higher-than-normal blood sugar but not yet high enough for a diabetes diagnosis:
- HbA1c test: A level between 5.7% and 6.4%.
- Fasting Blood Glucose test: A level between 100 and 125 mg/dL.
- Oral Glucose Tolerance Test: A result between 140 and 199 mg/dL after a two-hour period.
What is considered a normal HbA1c level? Does it change with age?
For most healthy adults, a normal HbA1c level is below 5.7%. While this is a general guideline, a doctor may set a slightly different target based on an individual’s age and overall health. For example, older adults or those with other chronic conditions may have a slightly higher target range to reduce the risk of hypoglycemia (low blood sugar), so it is important to discuss your personal target with your healthcare provider.