
13 Oct Parkinson’s Disease: A Complete Guide to Symptoms, Treatment & Care
Parkinson’s Disease: A Complete Guide to Symptoms, Treatment & Care
By Island Hospital | October 13, 2025 10:34:09 AM
Waking up to a tremor that won’t listen, feeling a sudden stiffness that slows your every step, or facing a day where even simple tasks feel like a struggle—these are the quiet, daily battles that Parkinson’s disease brings. This is your reality, and it’s completely understandable to feel like you’re on a lonely path. But please, know this: you are not walking this journey alone.
Even a global icon like Michael J. Fox, a beacon of hope and resilience for so many, shares this very diagnosis. His journey since he was diagnosed at 29 years old, reminds us all that a Parkinson’s diagnosis doesn’t have to define your life.
This article is for you. It’s a compassionate guide to help you navigate the daily challenges and understand what’s happening in your body.
We’ll show you that a full, meaningful life is still within reach, connecting you with effective strategies for managing your symptoms and a supportive community right here in Malaysia.
What is Parkinson’s Disease?
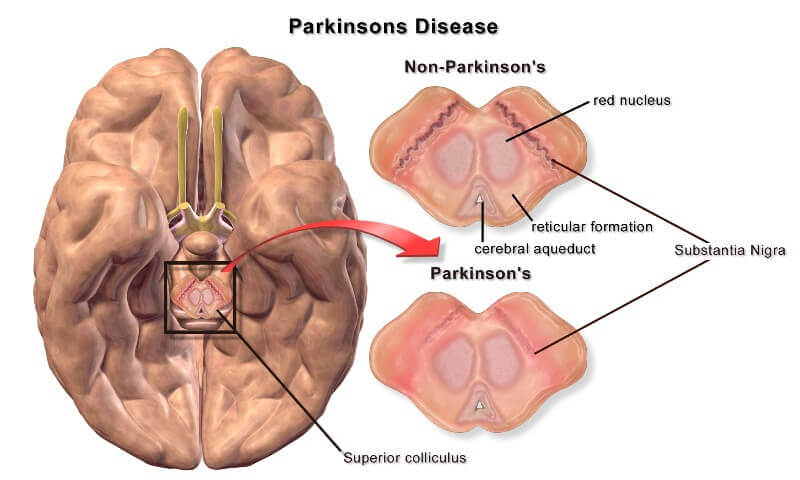
Parkinson’s disease is a progressive neurological disorder that primarily affects movement. To understand it, think of your brain as a complex conductor for a symphony. One of the key players in this orchestra is a chemical messenger called dopamine, which is responsible for coordinating smooth, purposeful movements.
In Parkinson’s disease, the brain cells that produce dopamine begin to gradually die off. As a result, the body’s ability to control movement is compromised, leading to the characteristic symptoms of the condition.
Early Signs and Symptoms of Parkinson’s
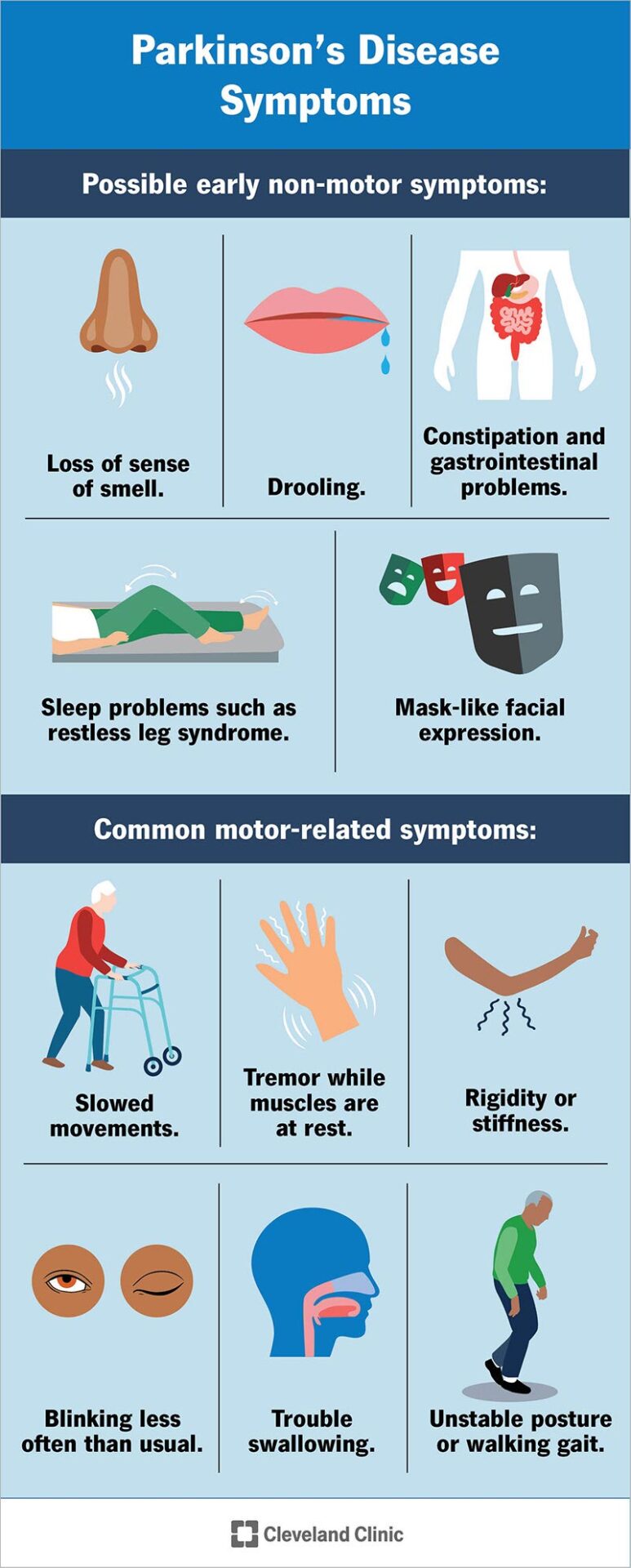
While tremors are the most recognisable sign of Parkinson’s, its full range of symptoms is often a hidden challenge. These signs can be subtle and varied, affecting not only movement but also non-motor functions like sleep, mood, and even sense of smell.
Learning to spot these early changes is vital, as it can lead to a more timely diagnosis and better long-term management.
5 Common Early Symptoms to Look Out For
- Tremor: A tremor, or shaking, often begins in a limb, typically in a hand or finger. It may occur even at rest.
- Slowed movements (Bradykinesia): This is one of the most common signs and can make simple tasks difficult and time-consuming. You may find that your steps become shorter when you walk, or that it’s harder to get out of a chair.
- Muscle stiffness: Rigidity can occur in any part of your body. This can be painful and may limit your range of motion.
- Impaired balance: Your posture may become stooped, and you may find it difficult to maintain your balance.
- Changes in handwriting or speech: Handwriting may become noticeably smaller (micrographia). Your speech may become softer, more monotone, or slurred.
Non-Motor Symptoms You Shouldn’t Ignore
Beyond movement-related issues, Parkinson’s can present with a range of non-motor symptoms that can often appear years before motor symptoms. These can include sleep disturbances, mood changes (such as anxiety or depression), fatigue, constipation, and loss of smell.
Causes and Risk Factors
The exact cause of Parkinson’s disease remains largely a mystery, but a complex interplay of genetic and environmental factors is believed to be the root cause. While researchers have not pinpointed a single trigger, what we do know so far provides important clues.
What We Know So Far
- Genetics
Researchers have identified specific gene mutations that can increase the risk of Parkinson’s. While hereditary cases are rare, family history is a known risk factor. - Environmental factors
Exposure to certain toxins or environmental factors may increase the risk of developing Parkinson’s, but the risk is relatively small. - Ageing
Age is the single biggest risk factor. The disease typically begins around age 60, but a small percentage of people can experience early-onset Parkinson’s before the age of 50.
How is Parkinson’s Diagnosed?
Unlike many conditions, Parkinson’s disease cannot be diagnosed with a single blood test or scan. Instead, a diagnosis is a careful, multi-step process that relies heavily on the clinical expertise of a neurologist. The primary goal is to identify a specific combination of symptoms while ruling out other potential causes.
1. The Clinical Evaluation
The most crucial step in diagnosis is a detailed clinical evaluation. Your neurologist will take a comprehensive look at your medical history, including any medications you’re taking and how your symptoms have progressed over time. During a physical exam, they will look for the hallmark motor symptoms of Parkinson’s:
- Bradykinesia: Slowness of movement, which can manifest as smaller handwriting or a shuffling gait.
- Tremor: A resting tremor, often beginning in a hand or finger, that subsides with movement.
- Rigidity: Stiffness or inflexibility in the limbs or trunk.
A diagnosis is typically made when a person exhibits at least two of these primary symptoms, with one of them being bradykinesia or a resting tremor.
2. The Role of Imaging
While no scan can definitively diagnose Parkinson’s, imaging tests play a vital supporting role. A neurologist may order tests like an MRI or PET scan to get a clearer picture of your brain’s health. These scans are primarily used to rule out other conditions that can mimic Parkinson’s, such as essential tremor, stroke, or other neurological disorders. In some cases, a PET scan may be used to look for evidence of reduced dopamine activity in the brain, which is a key sign of Parkinson’s.
3. The Importance of Early Diagnosis
Because the diagnosis is based on a doctor’s observation and evaluation, it can take time. However, getting an early and accurate diagnosis is critical. It allows you to begin treatment promptly, whether through medication or lifestyle adjustments, and gives you the best chance of effectively managing your symptoms and maintaining your quality of life for years to come.
Taking a proactive approach to your health starts with effective screening. Discover how to best prepare for your health screening in this comprehensive guide.
Treatment Options for Parkinson’s Disease
While there is currently no cure for Parkinson’s, a wide range of treatment options are available to manage symptoms and significantly improve a person’s quality of life. The best approach often involves a combination of medication, non-surgical therapies, and, in some cases, surgery.
1. Medications
Medications are the cornerstone of Parkinson’s treatment, designed to address the brain’s insufficient levels of dopamine.
- Levodopa
Considered the most effective drug for controlling the motor symptoms of Parkinson’s, levodopa works by being converted directly into dopamine in the brain. It is almost always prescribed in combination with carbidopa to prevent its premature breakdown, allowing more of the drug to reach the brain and reducing side effects like nausea. - Dopamine Agonists
Instead of replenishing dopamine, these drugs mimic its effects by directly stimulating the dopamine receptors in the brain. They are often used in the early stages of the disease or in combination with levodopa to help reduce motor fluctuations. - MAO-B Inhibitors
These medications help the brain’s natural supply of dopamine last longer. They work by inhibiting the enzyme, Monoamine Oxidase B, which is responsible for breaking down dopamine in the brain.
2. Non-Surgical Therapies
A comprehensive treatment plan goes beyond medication to address the physical and emotional challenges of Parkinson’s. A multidisciplinary team of therapists can play a crucial role.
- Physical Therapy
A physical therapist can create a personalised program to help you with balance, gait, and mobility issues. The goal is to improve your flexibility, strength, and coordination to reduce the risk of falls and help you move more confidently. - Occupational Therapy
An occupational therapist provides practical strategies to help you manage daily living tasks. They can offer solutions and modifications to make activities like writing, eating, dressing, and personal hygiene easier and less frustrating. - Speech Therapy: Speech and swallowing difficulties are common in Parkinson’s. A speech therapist can help you improve vocal volume and clarity (dysarthria) and teach safe swallowing techniques (dysphagia) to prevent choking and other complications.
3. Surgical Options
For select patients with advanced Parkinson’s, surgical intervention can be a life-changing option when medication alone is no longer providing adequate symptom control.
- Deep Brain Stimulation (DBS)
DBS is a sophisticated surgical procedure that involves implanting thin electrodes in specific areas of the brain. These electrodes are connected to a pacemaker-like device placed under the skin, which sends continuous electrical pulses to help control tremors, stiffness, and other motor symptoms. It can significantly improve a patient’s quality of life and often allows for a reduction in medication.
What to Expect at Island Hospital
Island Hospital offers a multidisciplinary approach to neurological care. Our Movement Disorder Clinic is a designated Centre of Excellence, staffed by highly experienced neurologists and neurosurgeons.
We utilise cutting-edge equipment, including advanced imaging technologies like the Siemens Biograph mCT PET/CT scanner, which can help in diagnosing neurological disorders. We are also proud to provide Deep Brain Stimulation (DBS) surgery for Parkinson’s patients.
Lifestyle and Self-Management Strategies
Beyond medical treatments, embracing healthy lifestyle habits is one of the most powerful tools for living well with Parkinson’s. Taking an active role in your daily routine can significantly improve both physical and emotional well-being.
- Regular Exercise
Consistent physical activity is one of the best ways to combat the motor symptoms of Parkinson’s. It’s not just about staying fit; it’s about maintaining your mobility. Activities like walking, cycling, swimming, tai chi, or yoga can all help improve your balance, flexibility, and muscle strength. Aim for regular movement that you enjoy to keep your body and mind active. - Balanced Diet
What you eat can have a direct impact on your brain health and energy levels. A diet rich in fruits, vegetables, and whole grains provides the antioxidants and fiber needed to support your overall health. Staying well-hydrated is also crucial. A dietitian can help you tailor your diet to your specific needs, including managing medication timing to ensure maximum effectiveness and reducing side effects. - Sleep Hygiene
Many people with Parkinson’s experience sleep disturbances, which can lead to fatigue and affect mood. Practicing good sleep habits is key. This includes maintaining a consistent sleep schedule, creating a dark and quiet bedroom environment, and avoiding caffeine and screens before bed to help your body prepare for rest. - Stress Management
Stress can often worsen Parkinson’s symptoms like tremors and stiffness. Learning to manage it is a powerful form of self-care. Techniques such as meditation, deep breathing exercises, mindfulness, or simply listening to music can help you cope with emotional challenges and find a sense of calm.
Emotional and Mental Well-Being
It’s normal to feel a range of emotions after a diagnosis. Coping with anxiety and depression is a vital part of managing the condition. Support groups can be an invaluable resource for sharing experiences and connecting with others who understand your journey.
Caregiver Support and Family Guidance
The journey with Parkinson’s is a family journey, and the role of a caregiver is crucial. Your dedication and support are invaluable, and it’s important for families to have access to both practical tips and a strong network of emotional support.
Practical Tips for Caregivers
- Learn About the Condition
Knowledge is power. By educating yourself on the symptoms, medication schedules, and potential progression of Parkinson’s, you can better understand what your loved one is experiencing and anticipate their needs. This includes learning about “on” and “off” periods and recognising subtle changes in their well-being. - Assist with Medication Schedules
Consistency is key for managing symptoms. Help your loved one stay on a strict medication schedule, as a delay of even a few minutes can impact their motor control. Consider using a pill organiser or setting phone reminders. - Encourage a Healthy Lifestyle
Be a partner in wellness. Encourage and join your loved one in their exercise routine, whether it’s a daily walk or a yoga class. Plan nutritious meals together to ensure they are getting a balanced diet that supports their brain health and energy levels. - Prioritise Your Own Well-being
The role of a caregiver is demanding, and burnout is a real risk. Make time for your own hobbies, rest, and social connections. Remember, taking care of yourself allows you to better care for your loved one.
Local Resources
Finding a community that understands can be a lifeline. The Malaysian Parkinson’s Disease Association (MPDA) is a key local resource that offers a wealth of support and education for patients, caregivers, and families. The MPDA provides:
- Support group meetings where you can connect with others facing similar challenges.
- Educational seminars to help you stay informed about the latest treatments and research.
- Social events that encourage community and reduce feelings of isolation.
By reaching out to organisations like the MPDA, you can find a network of support that truly understands your journey.
Myths vs. Facts about Parkinson’s Disease
Myth-busting is an important part of understanding any medical condition. When it comes to Parkinson’s disease, there are many misconceptions that can create unnecessary fear and misunderstanding.
Separating the myths from the facts is the first step toward a more informed and empowering journey. The table below helps clarify some of the most common beliefs about Parkinson’s.
| Myth | Fact |
|---|---|
| “Only old people get Parkinson’s.” | While it is more common in older adults, younger-onset Parkinson’s disease can affect people under 50 |
| “Parkinson’s only causes tremors.” | Non-motor symptoms such as depression, anxiety, sleep problems, fatigue, and loss of smell are common and can significantly impact a patient’s quality of life, often appearing years before motor symptoms. |
| "There’s nothing you can do once diagnosed." | On the contrary, many effective treatment and lifestyle options exist to manage symptoms and enable a high quality of life for many years. Early diagnosis and proactive management are key to slowing symptom progression. |
Debunk common myths about Parkinson’s Disease and ensure that you’re fully prepared for your next doctor’s visit in this article: Ask Our Parkinson’s Specialists: Addressing Your Concerns About a New Parkinson’s Diagnosis.
When Should You See a Doctor?
If you or a loved one are experiencing persistent symptoms like shaking, stiffness, or slowed movements, it is essential to consult a neurologist for an evaluation. Early diagnosis allows for a proactive approach to managing the disease and preserving your quality of life.
Who Should I Consult?
At Island Hospital, we have a team of neurologists with vast expertise in movement disorders, including names like Dr. Yap Siew Mei and Dr. Wong Chee Keong. Our designated Neurology and Neurosurgery specialty is equipped to provide comprehensive care. Our Movement Disorder Clinic is a centre of excellence dedicated to the diagnosis and management of conditions like Parkinson’s disease.
A Path Forward
Parkinson’s disease is a complex condition, but with the right information, a strong support system, and a comprehensive care plan, it is possible to live a full and meaningful life.
We believe in empowering you with knowledge and standing alongside you on this journey. At Island Hospital, we are committed to being your partner in care, providing compassionate, advanced, and personalised support every step of the way.
Don’t face this journey alone. If you have any concerns or questions about a recent diagnosis or are seeking to better manage your symptoms, we encourage you to schedule a consultation with our neurology specialists. We are here to provide the expert guidance and care you deserve.
FAQs
Can Parkinson’s be cured?
There is currently no cure for Parkinson’s disease. However, this does not mean there is nothing that can be done. The good news is that a wide range of effective treatments—including medications, lifestyle adjustments, and therapies—are available to manage symptoms and significantly improve a person’s quality of life. With a proactive approach and a personalised care plan, many people with Parkinson’s continue to live full, active, and meaningful lives for many years after their diagnosis.
What is the difference between Parkinson’s disease and Parkinsonism?
This is a common and important question. Parkinson’s disease (PD) is the most common form of a broader group of conditions known as Parkinsonism. Parkinsonism is a medical term used to describe a set of symptoms that include tremors, slowness of movement (bradykinesia), and rigidity. While PD accounts for the vast majority of cases, other neurological conditions—such as multiple system atrophy (MSA) or drug-induced Parkinsonism—can also cause these symptoms. A proper diagnosis from a neurologist is crucial because these other conditions often require different treatments and have different prognoses than PD.
Can younger people get Parkinson’s?
Yes, absolutely. While it is true that the risk of Parkinson’s disease increases significantly with age, a small percentage of people are diagnosed before the age of 50. This is known as young-onset Parkinson’s disease (YOPD). The symptoms and progression can differ from those in older adults. For instance, YOPD is more likely to have a genetic link and may present with more rigidity and dystonia (involuntary muscle contractions) than tremors. A famous example of this is actor Michael J. Fox, who was diagnosed with YOPD at age 29.
Is Parkinson’s disease fatal?
Parkinson’s disease itself is not considered a fatal condition. People with Parkinson’s disease can live for many years after their diagnosis. However, the progressive nature of the disease can lead to complications that may become life-threatening. For example, severe stiffness can increase the risk of falls, while difficulties with swallowing (dysphagia) can lead to aspiration pneumonia. The goal of treatment is to manage symptoms effectively to prevent or minimise these complications, thereby protecting a person’s health and life expectancy.
Is Parkinson’s hereditary?
For the vast majority of people, Parkinson’s is not hereditary. Most cases are considered sporadic, meaning they occur without a known family history. However, there is a small percentage of cases (about 10-15%) that have a known genetic link. Researchers have identified several specific gene mutations that can significantly increase a person’s risk of developing the disease. If you have a family history of Parkinson’s, a genetic counselor can help you understand your personal risk.






