23 Mar Bariatric Surgery
Bariatric Surgery
By Island Hospital | Mar 23, 2020 3:26:24 PM
Bariatric surgery is a collective name for weight-loss surgery procedures that can help morbidly obese patients lose weight by making changes to their digestive system. These changes are often permanent, requiring commitment to life-long changes and adjustments to one’s lifestyle.
Obesity is a lifestyle problem; but for some people like the morbidly obese, the solution is often more complex than eating less, exercising more and a healthy diet. There are individuals who struggle to lose weight even after making many lifestyle adjustments, largely due to a combination of different external factors that are out of one’s control. Those struggling with obesity also struggle with health risks such as type-2 diabetes or high blood pressure.
While bariatric surgery is often a solution for those who struggle to lose weight; it is also not an easy way out of obesity and should not replace a healthy lifestyle.
The most common way to measure obesity is by calculating one’s BMI. One is generally considered overweight or pre-obese at a BMI of 25 and higher, while having a BMI over 30 classifies as being obese. The obese weight class is further divided into three classes:
Obese class I: BMI of 30 to 34.9
Obese class II: BMI of 35 to 39.9
Obese class III: BMI equal to or over 40
Class III obesity can also be classified as morbid obesity or severe obesity, and is widely considered a serious health condition. Individuals who are morbidly obese often experience difficulty with basic physical functions, as well as having an extremely high risk of developing several dangerous health complications due to excess weight.
It is important to understand that an individual’s BMI is only an estimate, as there are factors such as muscle mass or visceral fat to consider for certain people. Your BMI may not be at 35, but you may suffer from conditions like type-2 diabetes that still pose a risk to your health. BMI is not perfect as it measures using weight, not fat or muscle mass. Bodybuilders with low body fat may have a muscle mass that contributes to their BMI being calculated as overweight or obese, for example.
A proper assessment or input from a medical professional is advised if you wish to know how your current BMI may affect your daily life.
Apart from hindered basic physical functions, individuals who are overweight also suffer from increased risk of potentially fatal illnesses such as type-2 diabetes or high blood pressure.
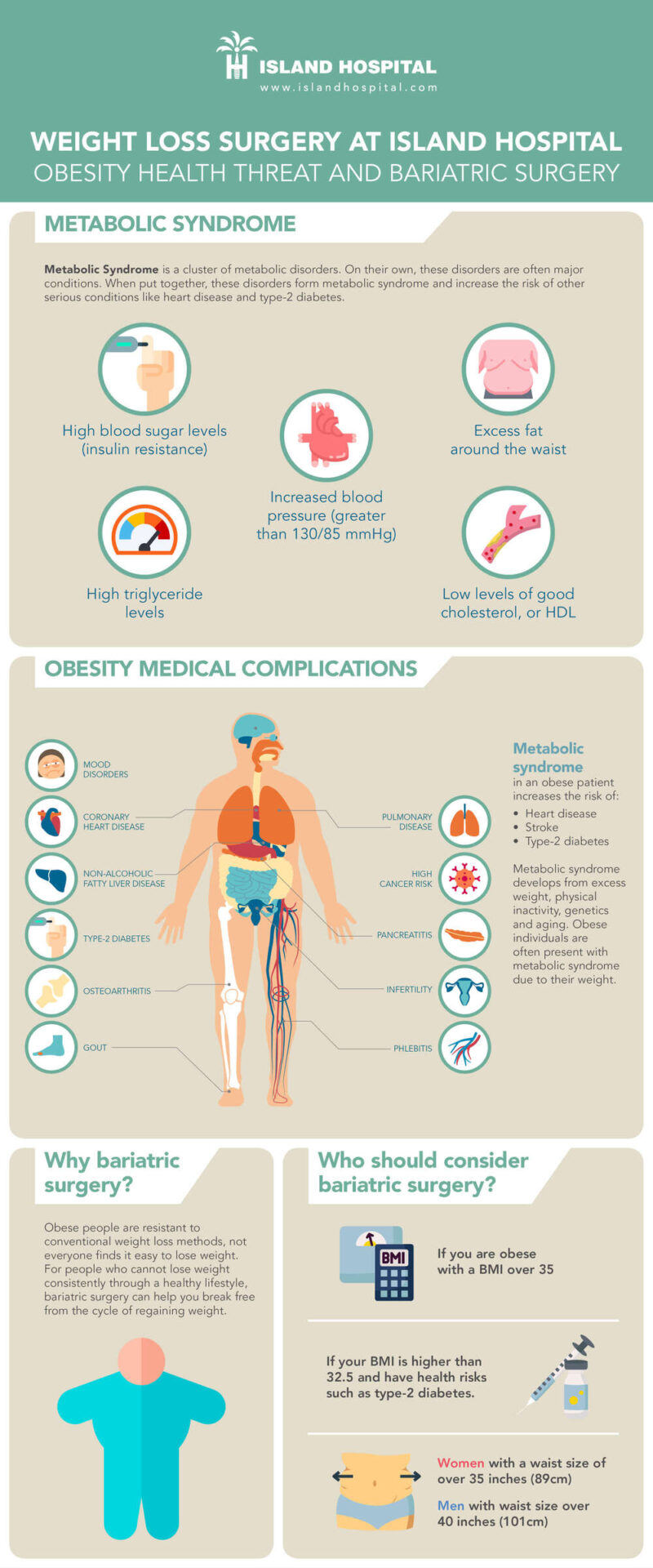
Obesity is primarily linked to what is called metabolic syndrome. Metabolic syndrome is a cluster of metabolic disorders, namely high blood pressure (hypertension), high blood sugar, excess body fat around the waist and abnormal cholesterol or triglyceride levels.
When a person has metabolic syndrome, the risk of heart disease, stroke and type 2 diabetes increases. Metabolic syndrome is caused by excess weight, physical inactivity, genetic factors and aging; hence why people are more likely to develop metabolic syndrome as their weight increases while severely obese patients are often present with metabolic syndrome.
When a number of illnesses are present alongside a primary health condition (for example, high blood pressure in an obese person), the accompanying conditions are known as comorbidities. While heart disease, stroke and type-2 diabetes are not under metabolic syndrome, they are comorbidities that can be caused by metabolic syndrome. Hence, as metabolic syndrome develops due to weight, the risks of comorbidities increases together with the developing metabolic syndrome and weight of the patient.
This is why obese patients have a higher risk of developing illnesses when they continue to gain weight, while morbid obesity is regarded as a serious health condition due to the existence of metabolic syndrome and risks of comorbidities being extremely high.
Some of the comorbidities associated with obesity are:
Type 2 diabetes
Obese individuals build up a resistance to insulin, causing their blood sugar to increase together with the risk for Type 2 diabetes. When people overeat or enter a state of overnutrition, a network of membranes called the endoplasmic reticulum (ER) sends signals to the insulin receptors to stop producing insulin. This suppressing of the insulin receptors is what causes insulin resistance and makes it difficult for the body to remove sugar.
Heart diseases & high blood pressure
Increase in fatty tissue can directly contribute to atrial enlargement and ventricular enlargement, which causes the heart to work harder in order to pump blood throughout the body. This increases the risk of cardiovascular diseases and high blood pressure.
Pancreatitis
Pancreatitis is a condition where your pancreas becomes inflamed or damaged as a result of your digestive enzymes working inside the pancreas before they are released out to the rest of the body. While it often causes irritation and discomfort, it can develop into a severe condition and damage other vital organs such as our heart, lungs and kidneys.
Osteoarthritis
Excess weight places additional stress on the joints, which speeds up the degeneration of cartilages and causes pain in the joints. Knee osteoarthritis is especially common among obese patients as the knee shoulders our weight when we are walking. Other areas affected by weight are our hips and lower back, as our weight increases the stress applied on those areas increase too.
Gout
Gout is characterized by a very intense pain at a joint, usually at the joint of your big toe; but can also occur in other joints as it is a complex form of arthritis. It occurs when urate crystals accumulate at a particular joint to cause inflammation; these crystals are formed due high levels of uric acid in your blood. Obese individuals produce more uric acid in their bodies, and have a higher risk of developing gout if their kidneys cannot keep up with the elimination of uric acid.
Phlebitis
Phlebitis is when a vein swells and becomes inflamed, causing irritation or pain in that specific area. If left for long, it may block the blood flow in the veins and lead to serious complications such as Deep-vein Thrombosis (DVT). Poor blood circulation in obese individuals tends to contribute to inflammation, which increases the risk of Phlebitis and DVT.
Sleep apnea & breathing problems
The fat deposits around airways cause blockage, restricting the amount of air taken in when inhaling. The body will send signals to the brain to wake you up, causing you to lose sleep. Sleep apnea can develop into a serious issue as it affects rest, causing drowsiness during the day, inability to sleep properly (insomnia) and may even cause you to stop breathing in your sleep.
Heartburn
When abdominal pressure increases due to excess weight, leakage or backflow of stomach acid can occur. This can lead to acid reflux or heartburn, which can further develop into Gastroesophageal reflux disease (GERD).
Infertility
Obesity in both men and women negatively affects the sperm production of men and the ovulation of women. Leptin is a hormone that signals our brain when we are hungry or full, to control our body fat. When our body fat increases, our leptin count goes up; which then inhibits other hormones. The hormones of our reproductive system are affected as a result.
Obese people build a certain resistance to normal methods of weight loss as they gain more weight, those in the third obese class may find it much more difficult to lose weight compared to people who are not obese. This is why exercising and eating less may not be an effective solution for everyone. Our body types, genetics and hormones can affect the rate at which we lose or gain weight, which is why some of us find it easier to lose weight than others. The reverse is also true, some people may find it tough to lose weight but easy to regain lost weight.
As such, while eating less and exercising more is the common way to treat obesity, for those who cannot achieve a healthy weight despite lifestyle changes: bariatric surgery is an option for you to consider. Remember that bariatric surgery is not a miracle solution for any obese person to lose weight. Obesity can be considered a lifestyle problem, where the person is trapped in a cycle of losing and regaining weight; or their body is at a balance of not losing enough weight. Bariatric surgery breaks that cycle, giving the person a chance to get into a new cycle that involves eating less, getting good exercise and living healthier.
Before surgery, a patient has to go through consultation and evaluation with a surgeon or physician well-versed in bariatrics, like the consultants at Island Hospital. Be prepared to eat in moderation, follow diet plans (as instructed by your doctor) and exercise regularly. Bariatric surgery can help you reach a point where these conventional weight loss methods become effective again. It also causes changes in your hormones that makes you feel full faster and eat less, preventing overeating.
Bariatric surgery should be taken into consideration if you are obese with a BMI over 35, or if your BMI is higher than 32.5 but also have serious health risks such as the aforementioned comorbidities, especially type-2 diabetes. Bariatric surgery is especially effective in causing remission of type-2 diabetes, many patients have stopped or reduced their intake of diabetes medication after bariatric surgery. The change in the body’s hormones and weight loss helps the body regain control over insulin levels without relying on medication as much as before, provided they remain physically active and exercise a controlled intake of sugar.
Apart from knowing your BMI, it is also important to know your waist size. Having excess fat around your waist can also lead to health risks, compared to having fat in other parts of your body. In fact, waist circumference has been shown to correlate with metabolic syndrome more than percentage fat in other areas of the body. Women with a waist size of over 35 inches (89cm) and men with waist size over 40 inches (101cm) may be at a higher risk of developing metabolic syndrome or diseases related to obesity.
Whether it’s your first time reading about bariatric surgery or if you already have an idea of what bariatric surgery is, you should know that at Island Hospital we perform 3 types of bariatric surgery and 1 endoscopic procedure for outpatients.
Bariatric procedures at Island Hospital:
- Sleeve gastrectomy
- Roux-en-Y Gastric Bypass
- One-anastomosis Gastric Bypass
Weight-loss endoscopic procedures at Island Hospital:
- Gastric Balloon
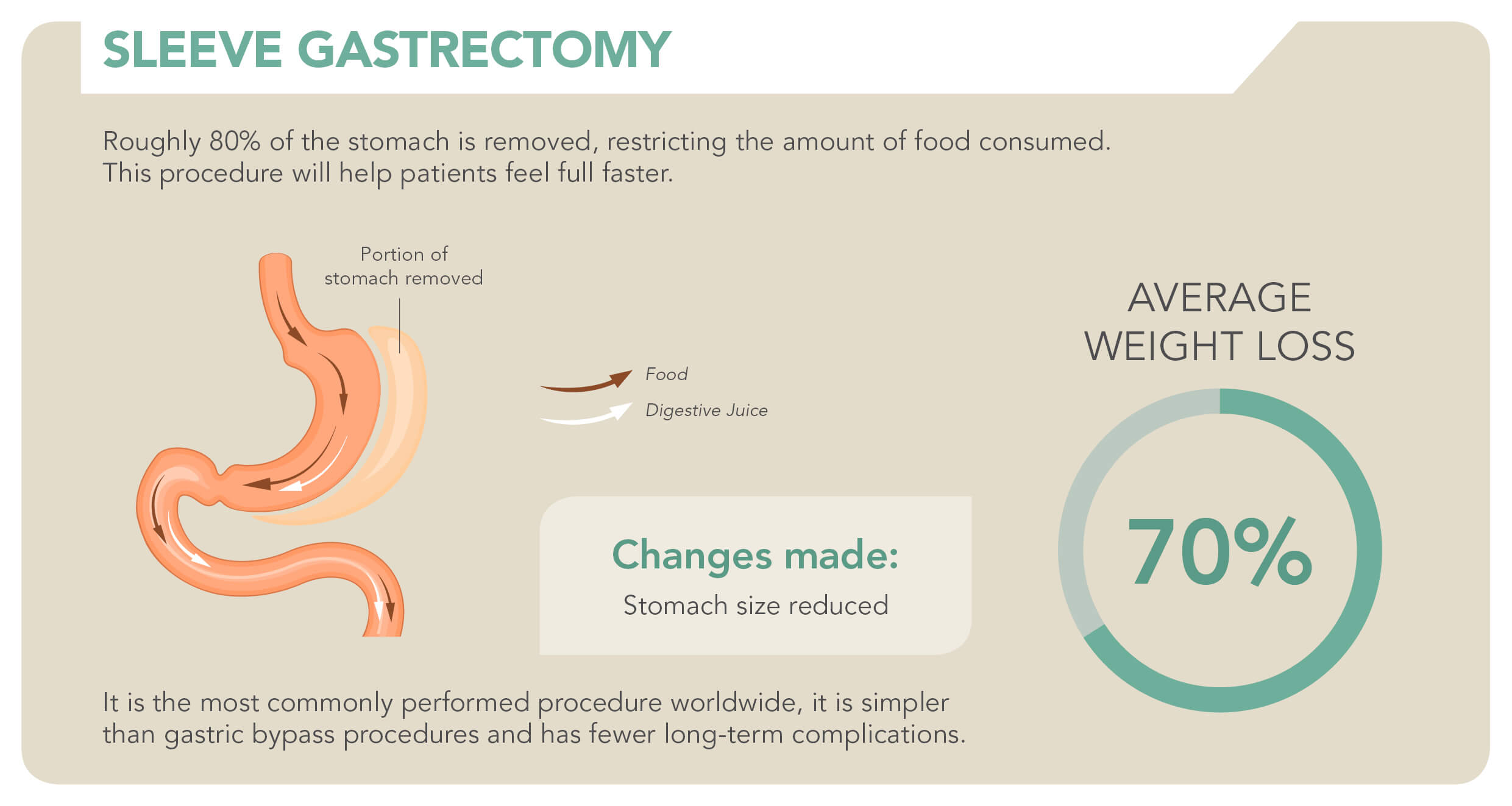
Vertical Sleeve Gastrectomy (VSG) – Is a weight-loss procedure where a large portion of the stomach is permanently removed (roughly 80%), reducing the size of the stomach from a pineapple shape to a banana shape. Limiting the stomach restricts the amount of food consumed, which also causes hormonal changes that assist with weight loss. It differs from gastric bypass procedures as there is no rerouting of the intestines needed. This procedure is permanent and non-reversible. It is a restrictive procedure.
Alternate names for this procedure are laparoscopic sleeve gastrectomy, gastric sleeve or simply the sleeve. Patients and doctors appreciate procedures like VSG as the procedures are laparoscopic, meaning the surgery is done without opening up one’s body. It is instead done through small incisions using tiny surgical instruments.
Vertical sleeve gastrectomy originated as a modification and first part in a bariatric procedure called the duodenal switch, which is a much more complex procedure that involves sleeve gastrectomy and intestinal bypass. It was also used as a safer alternative or first part in two-stage procedures for patients who have specific lung or heart problems that would make it difficult for them to undergo long procedures or anesthesia.
This is due to not requiring any rerouting of organs. For example, if a patient’s heart condition is deemed too weak for long hours of anesthesia (meaning they wouldn’t be able to undergo gastric bypass surgery), VSG can be carried out to help reduce the patient’s weight to a safer level before making the decision to have RYGB surgery. It has since become a procedure of its own, and at Island Hospital most of our patients go through the sleeve procedure. It is faster, safer and capable of producing results on par with gastric bypass procedures.
After-effects
The risk of having a major complication after surgery for sleeve gastrectomy is lower compared to other types of bariatric surgery, as only the stomach is affected and no organs are bypassed. While the chances are extremely low, it is important for you to take note in case symptoms do occur and you are not confused over what is happening to you.
Improvement of comorbidities – Sleeve gastrectomy assists in losing excess weight, and as a result helps to improve comorbidities in patients. Many patients experience remission of type-2 diabetes after sleeve gastrectomy, improving as their weight goes down. Some are diabetes-free a year after surgery. Improvements will continue to happen if one continues to maintain a healthy weight and lifestyle after the surgery.
Leaks and infection – the stapled portion of the stomach may leak, which will cause stomach acid and partially digested food to leak out. This will cause an infection and can be life-threatening. The odds of a leak happening are low, average statistics show only 1 in 200 patients experience an anastomotic leak; however it is best to be on the lookout for any signs or symptoms. Symptoms include fever, vomiting, feeling nauseous, rapid heart rate, stomach pain and bleeding.
Non-reversible – While there are some cases where gastric bypass procedures have been partially reversed, a sleeve gastrectomy is a permanent choice.
Dumping Syndrome – Dumping syndrome is a condition that occurs due to reduced stomach size. Food consumed travels down to the bowel at a faster speed and causes discomfort, caused by a lack of pacing or overeating during meals. Dumping syndrome causes weakness, dizziness, abdominal discomfort or vomiting, occurring immediately after a high-calorie meal, whereas late dumping syndrome occurs a few hours after consuming too much sugar.
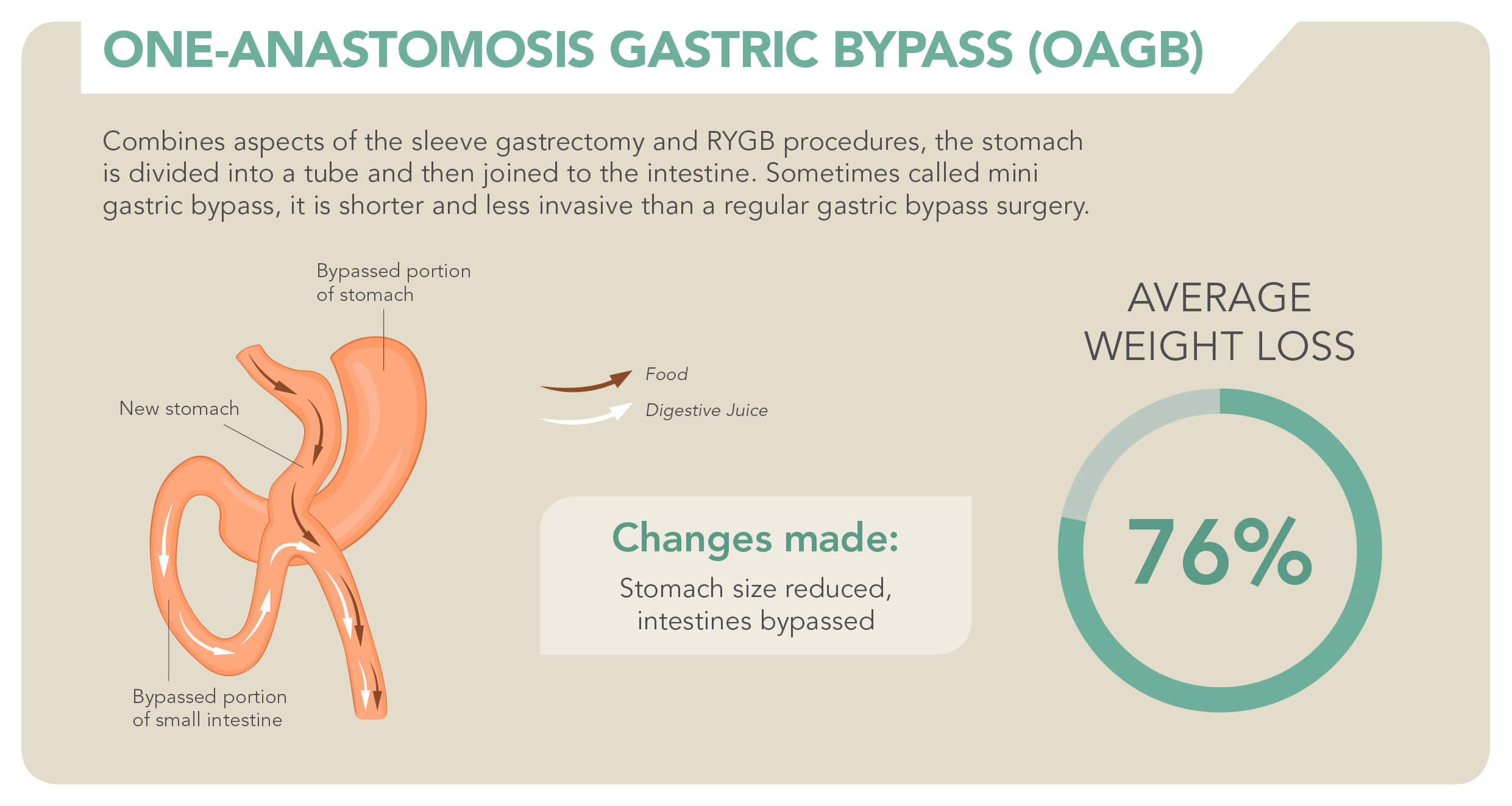
One-anastomosis gastric bypass (OAGB) – Is a weight loss procedure that combines certain aspects of the sleeve gastrectomy and Roux-en-Y gastric bypass. The upper portion of the stomach is divided into a tube similar to a sleeve procedure, and then joined to the intestine. It is both a malabsorptive and a restrictive procedure.
This procedure is also known as the Single Anastomosis Gastric Bypass or Mini Gastric Bypass. It is called mini as it involves less rerouting of the intestines and shorter surgery time compared to traditional gastric bypass surgeries.
The primary benefit of the OAGB is that the surgery is shorter and less invasive. The risk of complications is lower as a result, and there is a chance to reverse the surgery to reduce complications should there be post-surgical issues. The weight loss may not be as dramatic as traditional gastric bypass, requiring more time to reach an ideal weight.
After-effects
As stated, the risk of a major complication occurring during or after OAGB is lower compared to traditional gastric bypass. However, the possibility still exists and one should take note of any potential complications.
Improvement of comorbidities – The most prominent side effect of the surgery is of course, the loss of weight. The loss of excess weight allows one to control their blood sugar and blood pressure without their body building up resistances to interfere with the regulating process. Comorbidities will gradually improve as the patient continues to lose weight after surgery.
Leaks and infection – The stapled portion of the stomach may leak, which will cause stomach acid and partially digested food to leak out. This will cause an infection and can be life-threatening. The odds of a leak happening are lower for OAGB patients, as there is only one anastomosis compared to two in RYGB patients (hence, why it is called one-anastomosis). However, it is best to be on the lookout for any signs or symptoms. Symptoms may include fever, vomiting, feeling nauseous, rapid heart rate, stomach pain and bleeding.
Dumping Syndrome – Similar to the RYGB procedure, dumping syndrome can occur in OAGB patients due to the rerouting of the stomach. The food travels down to the bowel at a faster speed and causes discomfort in patients. Dumping syndrome causes weakness, dizziness, abdominal discomfort or vomiting, occurring immediately after a high-calorie meal, whereas late dumping syndrome occurs a few hours after consuming too much sugar. It should be noted that while dumping syndrome can be uncomfortable to go through, it is also an effective deterrent as patients will avoid eating too much or eating too quickly so they won’t have to experience dumping.
Malabsorption – Malabsorption is an after-effect of gastric bypass surgeries, as most gastric bypass are malabsorptive procedures. The malabsorption is a key factor in helping you lose weight because your body does not absorb as many calories as before, but that also means your body absorbs less nutrients.
Nutritional deficiency – Malabsorption leads to nutritional deficiency, requiring you to receive essential nutrients and vitamin supplements. Your doctor will also recommend a specific diet plan or types of food to eat so you can get sufficient nutrients for your day-to-day life.
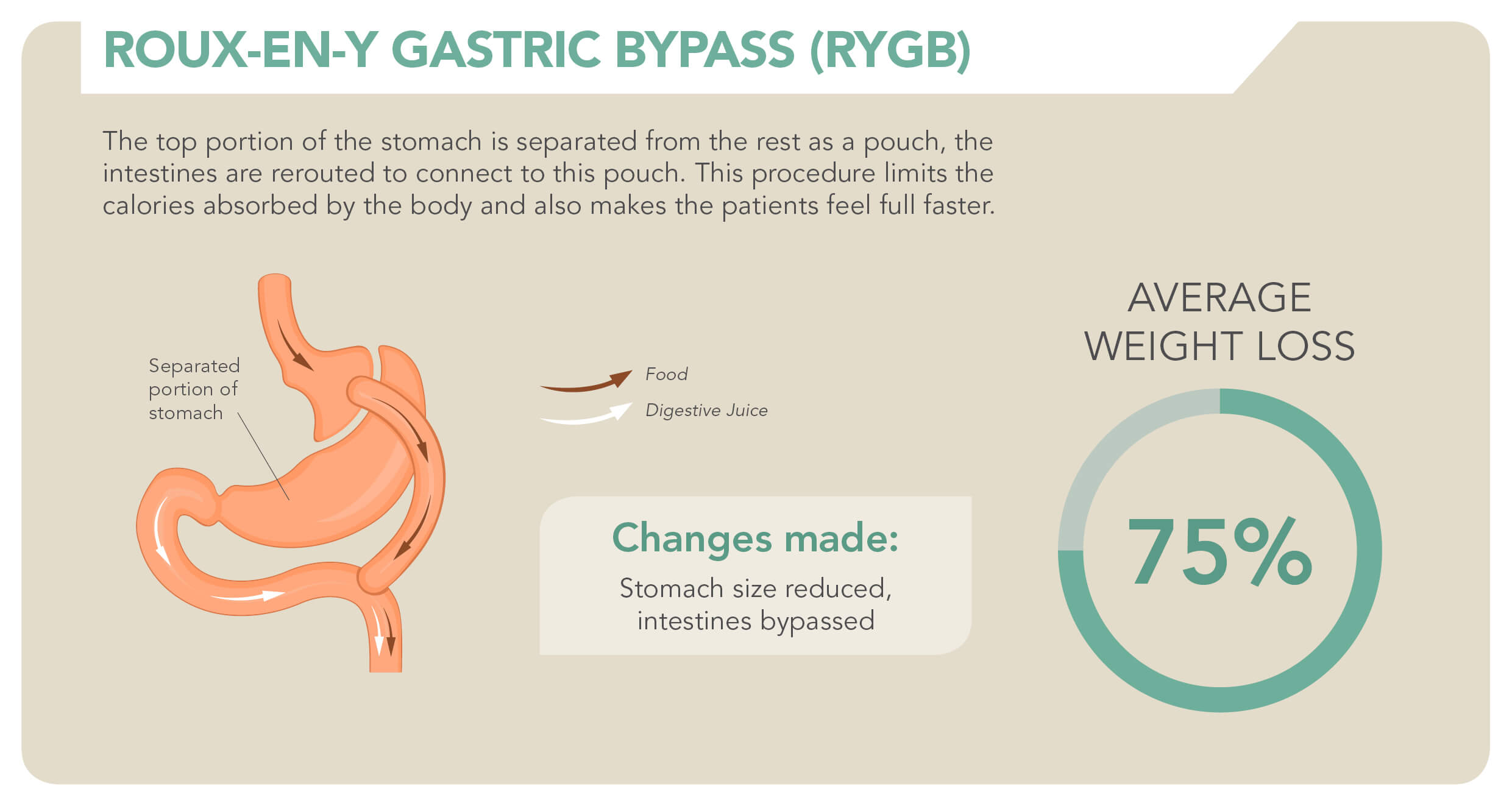
Roux-en-Y gastric bypass (RYGB) – The Roux-en-Y gastric bypass is a bariatric procedure where a small portion at the top of the stomach is separated from the rest, creating a smaller stomach “pouch” to hold food. With this smaller pouch stapled up, patients will feel full faster and eat less.
The small intestine is then separated and sewed onto this stomach pouch, resulting in food bypassing most of the stomach as it enters the small pouch and directly going into your small intestine. While this causes your body to absorb fewer calories to assist weight loss, it also means absorbing fewer essential nutrients.
Roux-en-Y gastric bypass is a malabsorptive and restrictive procedure, meaning the procedure limits food absorption (malabsorptive) while also limiting food intake (restrictive). It is considered to be the gold standard of weight loss procedures as it is highly successful in terms of weight loss and is the most commonly performed weight loss surgery overseas.
Apart from producing a higher average weight loss in patients as compared to the other procedures, RYGB also improves most of the aforementioned health conditions; such as high blood pressure or diabetes. The risks of conditions related to excess weight decrease as excess weight and fat is lost after the operation.
After-effects and risks
Improvement of comorbidities – Health risks influenced by one’s excess weight such as the aforementioned type 2 diabetes, hypertension and osteoarthritis begin to improve after the surgery. Improvements may continue if one maintains a healthy weight and lifestyle after the surgery.
Weight loss – Weight loss produced by RYGB is significant and perhaps the quickest among the procedures, and can be maintained by following the doctor’s advice. Most patients lose up to 75% of their excess weight after RYGB.
Malabsorption – Bypassing a large portion of your stomach and duodenum means skipping past a large portion of where your body breaks down food and absorbs nutrients. This means you absorb fewer calories and nutrients from food, known as malabsorption. Malabsorption triggers initial weight loss after the procedure and helps you maintain weight loss as your body absorbs fewer calories, but the downside is that your body also absorbs fewer nutrients.
Nutritional deficiency – Similar to malabsorption, nutritional deficiency is one of the side-effects of Roux-en-Y gastric bypass. Because your body doesn’t receive sufficient essential nutrients, vitamin supplements will become a major part of your daily life to avoid suffering from nutritional deficiency.
Dumping Syndrome – Also called rapid gastric emptying, dumping syndrome occurs when food and gastric juices move from your stomach to bowel at an uncontrolled speed or if you consume too much sugar. Dumping syndrome causes weakness, dizziness, abdominal discomfort or vomiting. The odds of this happening increases in patients of the RYGB and VSG procedures, as the reduced size of the stomach pouch causes food to travel into the small intestine at a quicker pace compared to people with a full stomach. You will have to be mindful of the pace you eat as well as how much sugar you consume. Dumping syndrome occurs immediately after a high-calorie meal, whereas late dumping syndrome occurs a few hours after consuming too much sugar.
Leakage or infection – The staples around the stomach pouch may fall apart, causing leakage or infection. The chances are extremely low (approximately 1 in 200 patients experience leakage), but it is best to have your doctor updated on your condition and to be wary of any signs or symptoms. Leakage will require surgery to re-staple the stomach pouch. Symptoms may include fever, vomiting, feeling nauseous, rapid heart rate, stomach pain and bleeding from the surgical wound.
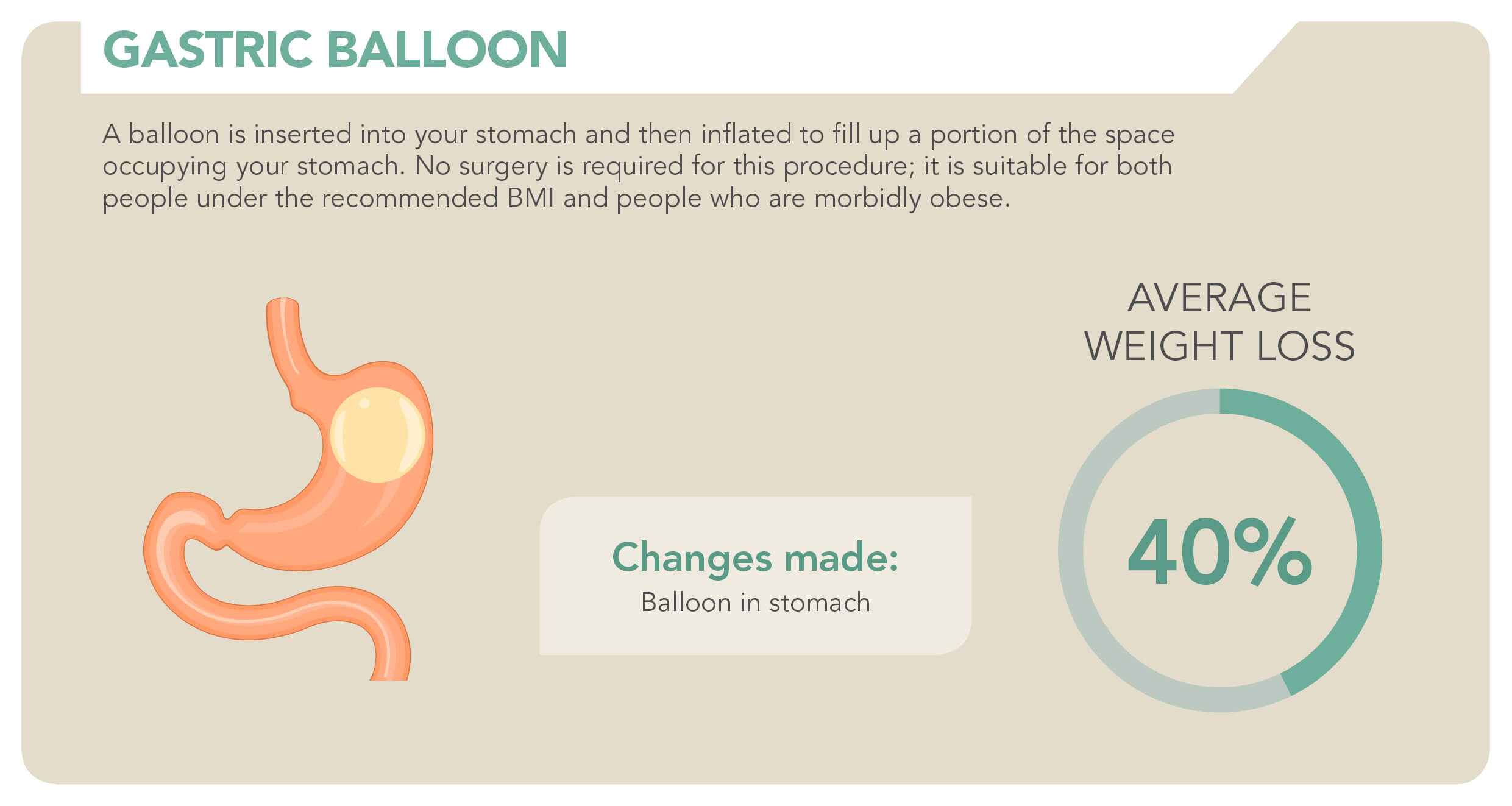
Gastric balloon
A question that might be going through your head is “what if I’m not morbidly obese but I have type-2 diabetes and find it difficult to lose weight?” or “what if I’m not suitable for certain types of bariatric surgery due to health conditions?”. Not everyone may be eligible for surgery, which is why procedures like the gastric balloon exist.
The gastric balloon is also known as the intragastric balloon or endoscopic gastric balloon. This procedure is an outpatient endoscopic procedure. Patients do not need to stay in the hospital, this procedure can be done and the patient returns home after the procedure.
The gastric balloon (some call it the stomach balloon) is a medical device that is placed into your stomach while you are under local anesthesia. As an endoscopic procedure, this balloon is inserted through your mouth. The balloon is only inflated after it is in your stomach, after which you will remain in the clinic to be monitored for a few hours.
The balloon makes you feel full faster after eating, and will remain in your stomach for 6 months. Gastric balloon patients will have to work harder than patients of other bariatric procedures in order to achieve higher weight loss.
The primary advantage of the gastric balloon is that it is quick and done without surgery required. It is suitable for patients who do not meet certain requirements for other surgeries, such as BMI lower than 35, or if it is dangerous for them to go through bariatric surgery due to certain health conditions. Some people have conditions that put them at risk, and they are required to lose some weight before they go through surgery. For them, the gastric balloon is a great alternative to bring their weight down to a level suitable for surgery.
The balloon is removed from the patient’s body after 6 months, restoring the patient’s stomach size back to normal. When considering the gastric balloon, one should treat it as a procedure that helps the patient get used to eating less; preparing them for life after the balloon is removed from their body. If your eating habits are not controlled after the balloon is removed, then there is a high chance you will regain the weight you have lost.
After-effects
The gastric balloon is less complicated compared to other bariatric procedures, but as a result will also require more effort from the patient to produce major weight loss.
Weight loss – The weight loss for this procedure depends on the patient’s efforts. The balloon is responsible for making the person feel full faster, but the patient has to follow the doctor’s diet plan and exercise. After the balloon is removed, patients will regain the weight they have lost if they do not commit to the lifestyle they adopted during their gastric balloon treatment.
Improvement of comorbidities – With the loss of weight also comes the improvement of comorbidities. While not as drastic as the other procedures, comorbidities will still improve as long as the patient loses weight during the period of treatment.
Balloon deflation – Although the chances are very low, there is a possibility that the balloon deflates. If it deflates to a size that is small enough, there is a risk that it will move through your digestive system. This will cause discomfort and blockage that requires surgery to remove the balloon.
Stomach ulcers – Our doctor will prescribe pills for you to take during your treatment, this is to prevent any risk of your stomach developing ulcers or extreme discomfort caused by the balloon.
Stomach discomfort – You may feel discomfort for a while after the balloon is placed, it may take some time to get used to the balloon in your body. If the discomfort persists or you feel worse after a period of time, consider consulting your doctor again to reduce the risk of stomach illnesses developing.
As mentioned, bariatric surgery is often life-changing and brings about permanent results; it will be scary to be put in a position where you have to choose to make changes that you will be stuck with for the rest of your life. The choice is not easy to make, but for some people it may very well be an important consideration if:
Your BMI is over 35
Your BMI is over 32.5 and you experience one or more of the following health conditions:
- Type-2 Diabetes
- Hypertension
- Heart complications
- Sleep apnea
- Frequent soreness or pain in your joints (osteoarthritis)
Your weight causes you to experience difficulty in day to day basic functions such as:
- Breathing
- Walking
- Feeling out of breath after light or moderate physical activity
You are ready for a lifelong commitment
For Sleeve Gastrectomy, One-Anastomosis Gastric Bypass and Roux-en-Y Gastric Bypass, you will have to be prepared to commit to a lifelong habit of a diet given by your doctor; as well as supplements to cope with vitamin deficiency.
For gastric balloon patients, you will have to be ready to make re-visits to the doctor to and be wary of any complications that may arise due to issues with your gastric balloon.
You want to cultivate a healthier lifestyle
Surgery cannot replace healthy habits. Simply controlling food intake is not enough, the proper amount specified by your doctor must be followed to ensure complications do not arise. Physical activity such as exercise or sports for pre-surgery and post-surgery should also be discussed with your doctor.
Apart from the simple baseline of BMI and health risks, there may be other factors that vary based on individuals; hence why personalized screening and testing is required to ensure you are able to go through the procedure. Below are some general considerations that may or may not apply to you, but may help you make sense of the decision-making process and prepare for surgery should you choose to go through with it.
Lose weight – Depending on your current condition, you may be required to lose additional weight before the surgery. Decreasing the amount of fat around your liver and abdomen will allow you to have a laparoscopic surgery rather than an open surgery.
Eating habits – Cut down on sugar, carbohydrates and saturated fats. Do your best to avoid fried food, potatoes, pasta and bread. Slowly exercise portion control, do not binge. You can take supplements like multivitamin or protein shakes to get the essential nutrients your body needs.
Discontinue usage of tobacco and nicotine products – Most if not all surgeons require patients to be tobacco and nicotine free for a minimum of three months prior to the beginning of pre-surgery education, as smoking has been proven to drastically increase the risk of complications during and after bariatric surgery.
Prepare your medications and info – Before visiting our doctors for advice, list down all the medicines, vitamins, supplements you take; as well as any restrictions or allergies. This is to discuss which medicines you can or cannot take leading up to surgery.
Health complications – If you have diabetes, heart complications or any conditions, be sure to inform the doctor too.
Liquid or pureed food – You may want to prepare protein drinks, yogurt, milk, low-fat soups and some sugar free pudding at home for you to eat after your surgery, as your diet will be limited to pureed food for at least a month after surgery.
The duration of your stay will vary depending on which bariatric surgery you undergo, usually your stay will range from 1 to 2 nights after surgery. You should discuss the duration of your stay with your doctor and then pack your belongings accordingly. Generally, you would want to always include the following:
- Shirts
- Loose pants
- Comfortable footwear
- Toothbrush
After the surgery, your diet will begin with liquids for one week as your stomach recovers from surgery. The following three weeks will require you to consume pureed foods, while finally returning to regular foods four weeks after surgery.
Twice a day you will have to take a multivitamin, including a calcium supplement once a day and a vitamin B-12 injection every month. For the first few months after surgery you will have to attend medical checkups to monitor your health and condition, this may vary from laboratory tests to bloodwork and other exams.
As your body reacts to the weight loss after surgery you may experience some of the following:
- Body aches
- Fatigue
- Feeling cold
- Hair thinning or hair loss
- Mood changes
- Dry Skin
The aforementioned dumping syndrome may also occur for RYGB and VSG patients after surgery, it is advised that RYGB and VSG patients exercise a controlled pace of eating.
Can I undergo bariatric surgery if my BMI is not above 35?
Yes. That is the short answer. You do not necessarily need to be morbidly obese to be considered eligible for bariatric surgery. The main benefit of bariatric surgery is not for cosmetic purposes, it is to help with the remission of comorbidities and metabolic syndrome. If you suffer from comorbidities or metabolic syndrome but are concerned your BMI may not be considered “heavy enough” for the procedure, do consult our doctors for an evaluation that will help determine if bariatric surgery is necessary for you.
Is it easy to regain the weight I’ve lost?
It is important to remember that it is not easy to regain weight lost through bariatric surgery unless you are living in an uncontrolled manner. With the reduced stomach size and effects like dumping syndrome occurring when food intake is uncontrolled, patients will have to experience a lot of discomfort to regain weight. This occurs if you are unable to control your impulses and desire to eat even when you are not hungry.
What happens if I regain the weight I’ve lost?
There are medications to assist with weight loss to try and help you to get back into a weight loss cycle. Revision surgeries can be done, but will cost more money and will not be effective in the long run if you are unable to control your lifestyle habits.
Can I use my EPF savings for bariatric surgery?
Yes, withdrawal from EPF account 2 is possible for bariatric surgery and treatment.
How long will I be away from work?
Most patients return to work after one or two weeks depending on the surgery. You will feel tired if you do more than you can handle, and your energy levels will be lower for a while. Most jobs will require you to be back right away, but the safety of your own self and the people around you are more important. You should consider taking half days or working on alternate days, the recommended work-rest balance can be discussed with your surgeon.
The risk of dying from surgery is greater than dying from obesity
If you have been reading up until this point, you will know that this is not accurate. The risk of death is lower for bariatric surgery compared to other surgical procedures. Remember that bariatric surgery is not just for cosmetic purposes, reduction of excess weight significantly improves your health and reduces mortality rate. Life-threatening diseases are also improved or resolved after surgery, meaning the benefits of bariatric surgery far outweigh the risks.
Obesity is a choice
Many often consider being obese as a choice, not a disease. Some believe that in order to stop being obese, one just needs to start exercising and eat less. It is a topic that continues to be brought up from time to time, and perhaps the people around you have said similar things too. Of course, prevention is often better than cure; hence why most people try to keep their weight under control by means of diet or exercise.
What about those who are already obese? While a healthy lifestyle is a choice, for some people, obesity is not a choice. The morbidly obese especially are resistant to weight loss by diet or exercise, or the ability to maintain said weight loss.
There are a number of factors that can affect weight gain and weight loss in people; some of which are beyond our control, some are different for each individual.
Dieting, exercise and weight loss
Cutting down on calories is easier than exercising without cutting down on calories, after all it is easier to eat less than to burn calories through exercise. While it is easier to lose weight by consuming less calories, it is also easier to regain weight that way. A person who diets slows down their metabolism, burning less calories at rest. Continuing to do so will result in slower weight loss, or downright zero weight loss.
The most efficient way is to combine both, using physical activity to counteract the slowed metabolism; while slowly increasing the amount of energy your body burns with continuous exercise. This includes energy expenditure during exercise and also energy expenditure at rest. Resting expenditure is important as it accounts for most of the calories we burn in a day (we don’t exercise non-stop without resting), hence why it is important to counteract the slowed resting expenditure from dieting with exercise.
Just go to the gym
Not everyone can carry out the same training in the gym and obtain similar results. A person’s body type responds to exercise in a different way from another, knowing yours can help you figure out exactly what kind of exercise you need to do in order to lose weight effectively.
Body Type
There are 3 different body types that result in different builds and appearances for people. You may have that one friend who eats a lot but never seems to put on weight, another friend who seems to effortlessly gain muscle without doing intense exercise, or you could be one of those people where you find it difficult to lose weight even though you’re on a strict diet.
The ectomorph is the delicate, long and lean person. They find it difficult to build muscle, weight or fat, usually a result of their fast metabolism. For ectomorphs, their concern may be gaining weight instead of losing it.
Endomorphs or endomorphy is perhaps more common than ectomorphs. Endomorphs have wide builds, storing their muscle and fat in the lower half of their bodies. They have the potential to build more muscles, but at the same time also build more fat. Having a higher endomorphy means having a higher tendency of storing body fat, as most endomorphs have slow metabolism.
Mesomorphs are what the general public would consider to be ideal, as they are neither too lean nor too wide. They find it easier to build muscles compared to the previous two, and also find it easier to lose fat. Mesomorphs are often natural athletics with high metabolism.
Everybody is a mix of the three types, even the most extreme case of mesomorphy would have minor traits of endomorph and ectomorph mixed in. Consulting someone with the knowledge of these body types will help you figure out what kind of exercise is needed for you to lose weight and maintain weight loss, as you could be an endomorph with fast metabolism; or a mesomorph with ectomorph qualities.
Each of the three body types require different levels of intensity to lose weight during exercise, which is why not everyone can lose weight at the same rate even if they do the same thing. Finding out about your body type could help you plan out your exercises to lose weight in the most suitable and efficient way.